How I Treat Myeloma: 2022 Update.
10 slides. Hope it's useful for oncologists and patients. @NorthTxMSG @MyelomaTeacher
1/ Risk stratification: This is important both for counseling patients and to decide on treatment options. The more high risk factors, the higher the risk.
10 slides. Hope it's useful for oncologists and patients. @NorthTxMSG @MyelomaTeacher
1/ Risk stratification: This is important both for counseling patients and to decide on treatment options. The more high risk factors, the higher the risk.

2/ Initial therapy. The 3 main choices are VRd, DRd, and Dara-VRd.
I prefer VRd. But the other options are reasonable. Transplant eligible patients need 3-4 cycles, then stem cell collection.
I prefer VRd. But the other options are reasonable. Transplant eligible patients need 3-4 cycles, then stem cell collection.

3/ Initial Therapy. For patients not eligible for transplant, results with DRd are outstanding. But it is more expensive and requires prolonged use of a triplet. 

4/ Future of Initial Therapy: Many trials are evaluating 3 vs 4 drugs.
Quadruplets may come out on top. But are they needed for everyone? Or can patients MRD- after a triplet do just as well without the 4th drug. This is what we are trying to answer in our current RCT @mtmdphd
Quadruplets may come out on top. But are they needed for everyone? Or can patients MRD- after a triplet do just as well without the 4th drug. This is what we are trying to answer in our current RCT @mtmdphd
https://twitter.com/mtmdphd/status/1492143846754508806
5/ Transplant: Auto Transplant is still important. It's role is not in debate. Only the timing. In standard risk patients less than 65-70, early or delayed may be OK. Patient choice matters. Also prefer early transplant in high risk MM.
OS of early vs delayed at 8 years is same.
OS of early vs delayed at 8 years is same.

6/ Maintenance: Lenalidomide for standard risk; Lenalidomide plus Bortezomib for high risk is the current preferred approach.
Our current US cooperative group phase IIIs are looking at adding Dara, or MRD directed escalation or de-escalation.
Our current US cooperative group phase IIIs are looking at adding Dara, or MRD directed escalation or de-escalation.

7/ First Relapse. Thankfully with today's treatment first relapse occurs about 4 years following initial therapy. This will get longer with time.
When relapse occurs a number of options are available. Choice depends on what the patient is refractory to. My approach is below.
When relapse occurs a number of options are available. Choice depends on what the patient is refractory to. My approach is below.

8/ Second or higher relapse. Thankfully the first relapse regimen can usually work for a long time. This is also improving.
There are a number of treatment options available for second or higher relapses.
There are a number of treatment options available for second or higher relapses.

9/ Immunotherapy provides great promise: especially CAR-T and bispecifics. One CAR-T is already approved (ide-cel). One more maybe in a month (cilta-cel).
A number of bispecifics are showing high activity. And unlike CAR-T are "off the shelf". But none are approved yet.
A number of bispecifics are showing high activity. And unlike CAR-T are "off the shelf". But none are approved yet.

10/ In the future we may pick immunotherapy based on the target antigen. We will face the situation of myeloma refractory to BCMA targeted approaches. So I'm glad Talquetamab and Cevostamab target something besides BCMA. 

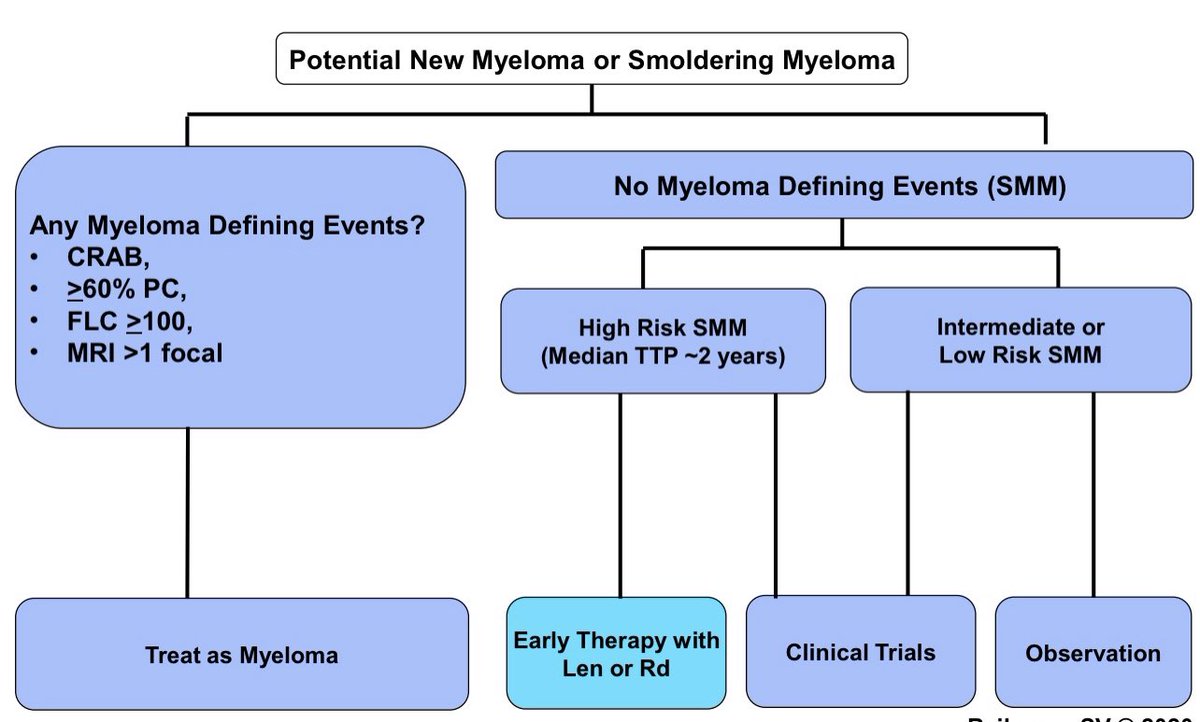
Link to thread from yesterday on How we treat smoldering multiple myeloma. @SagarLonialMD @mvmateos
https://twitter.com/vincentrk/status/1493323860598571010
Here is a summary of active drugs in myeloma and their mechanism of action. #MedTwitter #myelomaVR
Blue font: not yet approved.
Blue font: not yet approved.

• • •
Missing some Tweet in this thread? You can try to
force a refresh