Latest #infectionsurvey data from ONS shows prevalence rising in all four countries, with E&W turning upwards, a continued rise in S and NI reverting quickly to its previous very high levels.
1/
1/

The growth in prevalence at older ages is of particular concern. For 70+ levels are up over 50% in just two weeks.
2/
2/

Here's the full picture by age bands, showing a levelling off of previous falls at the youngest age group, and increases in all adult ages.
3/
3/

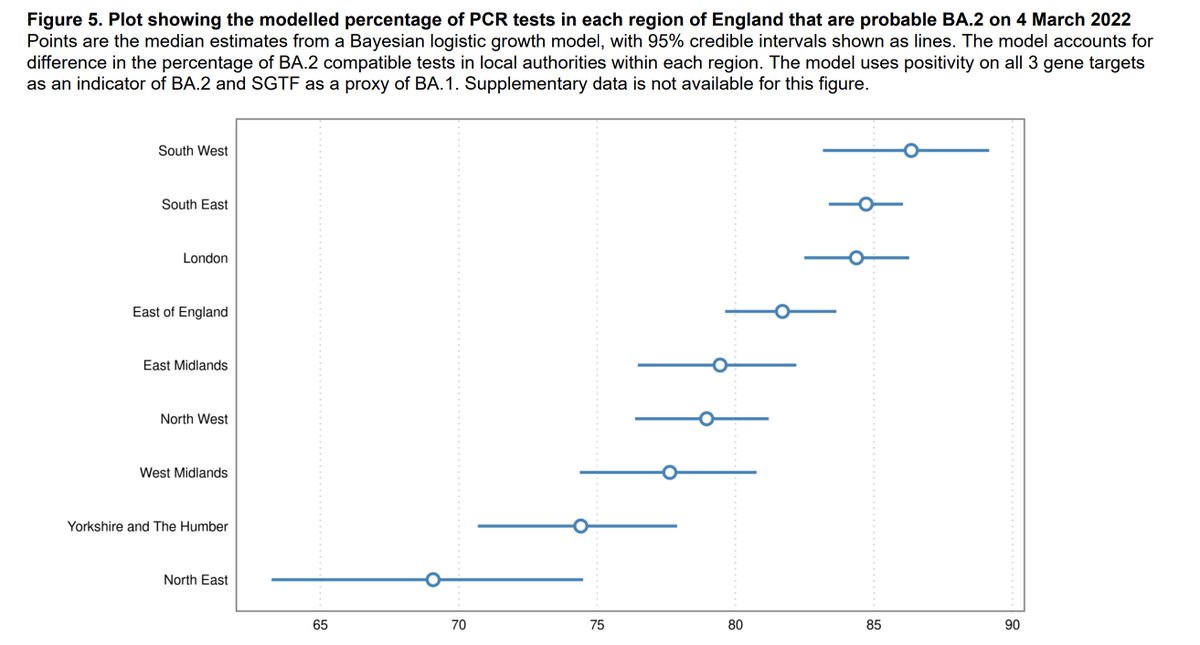
Regionally the East is showing the biggest increase and is now the highest, followed by London. The South West has been an area of concern recently, but the picture here looks more encouraging.
4/
4/

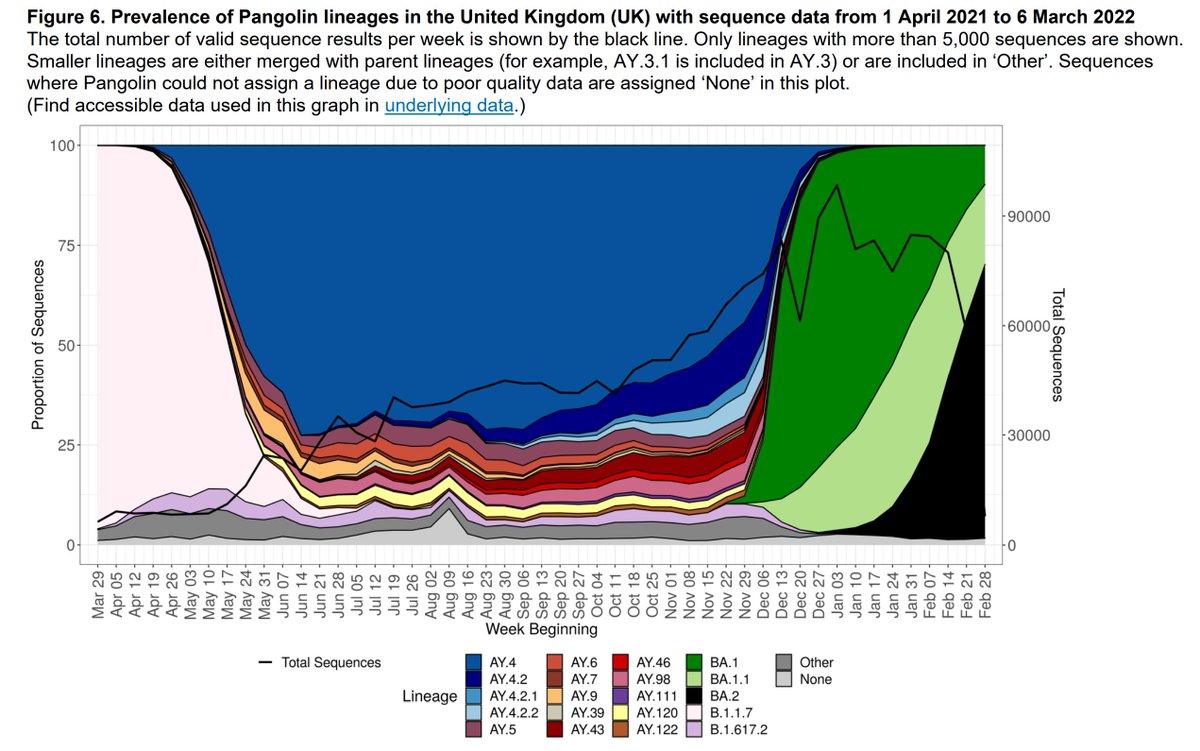
You can see here the rapid growth in BA.2 in both NI and S, and a more gradual increase in E and W. BA.1 is falling in three of the four countries, but appears to be level in NI.
5/
5/

Summary data here. Remember this is randomly sampled data so not influence by changes in the community testing regime.
6/6
ons.gov.uk/peoplepopulati…
6/6
ons.gov.uk/peoplepopulati…

• • •
Missing some Tweet in this thread? You can try to
force a refresh