It's #ResusciTuesday and today we discuss about the use of point-of-care ultrasound (POCUS) during Cardiopulmonary Resuscitation with @NatasaSpr
#ResusciTuesday #ResusTwitter #ERC #RESUS22 #FOAMed #POCUS
#ResusciTuesday #ResusTwitter #ERC #RESUS22 #FOAMed #POCUS
@NatasaSpr POCUS has been adopted by many physicians over the past decades and has been integrated in CA algorithms for the detection and treatment of reversible causes such as pneumothorax and cardiac tamponade. Many different protocols have been proposed. (Anesthesiology 2021;135:508–519) 

@NatasaSpr Pearls and Pitfalls
❌Right Ventricular dilation during CA: In isolation should not be used to diagnose massive PE. It is observed minutes after CA as blood shifts from systemic circulation to the right heart, probably as a result of hypovolaemia, hyperkalaemia and arrhythmia.
❌Right Ventricular dilation during CA: In isolation should not be used to diagnose massive PE. It is observed minutes after CA as blood shifts from systemic circulation to the right heart, probably as a result of hypovolaemia, hyperkalaemia and arrhythmia.
@NatasaSpr ❌Delays in chest compressions: Huis in’t Veld et al showed that use of POCUS significantly increase rhythm check pauses (Resuscitation 2017;119:95-98)
✔️Do not cause prolonged interruptions in chest compressions
✔️Use the most experienced sonographer other than team leader
✔️Do not cause prolonged interruptions in chest compressions
✔️Use the most experienced sonographer other than team leader
@NatasaSpr ✔️Prepare the machine (probe/depth/gain)
✔️Perform one window/pause
✔️Record a clip to review later
✔️Assign a timekeeper
acep.org/emultrasound/n…
✔️Perform one window/pause
✔️Record a clip to review later
✔️Assign a timekeeper
acep.org/emultrasound/n…

@NatasaSpr ❓What about pulse detection?
According to ALS algorithm, return of spontaneous circulation (ROSC) is detected based on rhythm check and central pulse palpation during a 2-second pause. Nevertheless, the accuracy of manual pulse detection varies greatly (63% to 94%).
According to ALS algorithm, return of spontaneous circulation (ROSC) is detected based on rhythm check and central pulse palpation during a 2-second pause. Nevertheless, the accuracy of manual pulse detection varies greatly (63% to 94%).
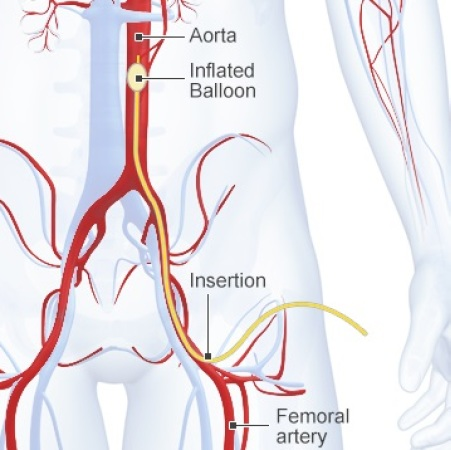
@NatasaSpr In a recent study by Cohen et al, femoral artery doppler ultrasound demonstrated higher accuracy than manual palpation for detection of any pulse (95.3% vs. 54.0%; p < 0.001). (Resuscitation - Published online: February 3, 2022)
@NatasaSpr Prognostication: PEA vs pseudo-PEA
PEA is defined as organized rhythm with neither palpable pulse nor cardiac contractility on POCUS. Pseudo-PEA has an organized rhythm on ECG and preserved cardiac contractility on POCUS, although not enough to generate pulse.
PEA is defined as organized rhythm with neither palpable pulse nor cardiac contractility on POCUS. Pseudo-PEA has an organized rhythm on ECG and preserved cardiac contractility on POCUS, although not enough to generate pulse.
@NatasaSpr But why do we care? According to a recent meta-analysis, pseudo-PEA has +LR of ROSC (6.87) and increased odds of overall survival(Resuscitation 2019;139:159–66) Which means that POCUS findings may identify patients who have a better prognosis and benefit from additional therapies
@NatasaSpr On the other hand, Reynolds et al pointed out that no sonographic finding has sufficient+consistent sensitivity to be used as a sole criterion to terminate resuscitation ➡️
@NatasaSpr ➡️since it is considered unacceptable to erroneously terminate resuscitation in a patients who could have survived. (Resuscitation 2020;152:56-68)
Nevertheless, according to ERC Guidelines 2021 POCUS should not be used as a sole indicator for terminating CPR.
Nevertheless, according to ERC Guidelines 2021 POCUS should not be used as a sole indicator for terminating CPR.
@NatasaSpr What about the future? Although POCUS is not yet the standard of care for CA patients, it is a valuable tool. Another modality, the Transesophageal echo (TEE) in CA is being investigating the past years, but this is a subject for another ResusciTuesday thread! ❤️💙
@NatasaSpr unroll @threadreaderapp
• • •
Missing some Tweet in this thread? You can try to
force a refresh