
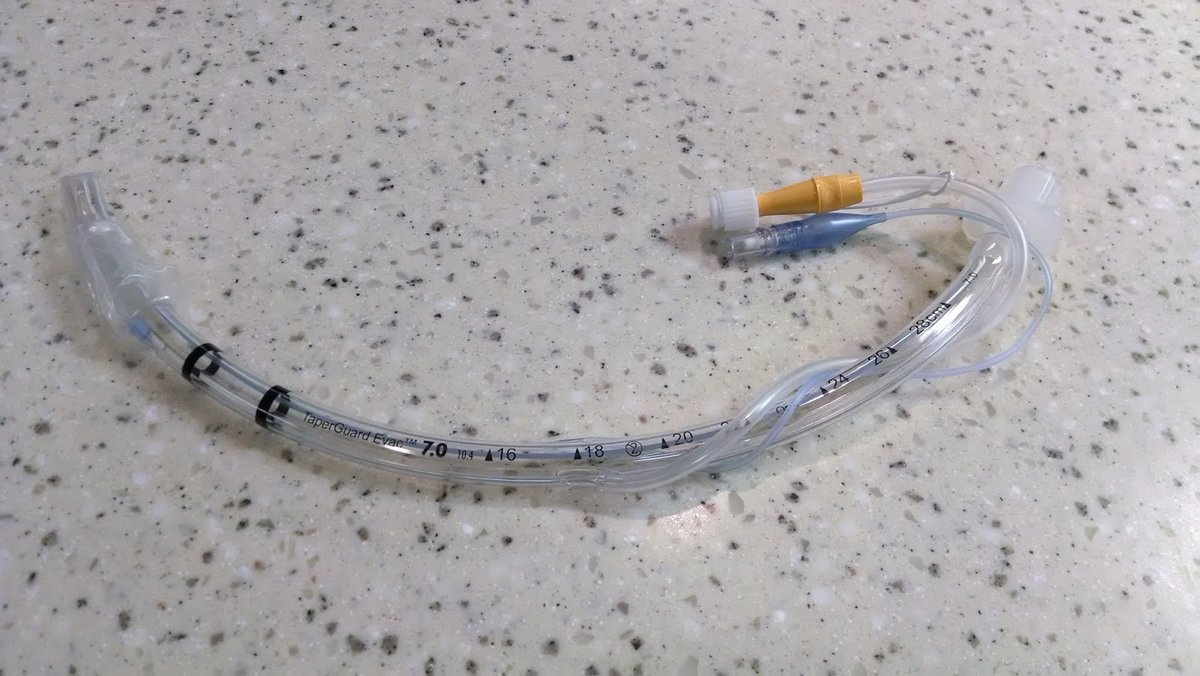
PSA: You *CANNOT* use a "bougie" or Eschmann Intubating Stylet to do an endotracheal tube exchange. I have seen this mistake twice in the past 6 months. You will lose the airway. A simple look at the length of the bougie and an #ETT will make this clear. 

The length of an adult ETT is about 32 cm and the length of the #eschmannstylete is 70 cm. This leaves no room in the center for you to grab it. When you retract the #ETT to the end of the stylet, its distal tip is still in the patient's mouth & entire stylet is covered
To do a tube exchange, you need 2x the length of the ETT and then some additional length to work with, else you risk retracting the exchange device too far and losing the airway. This is why they make an "airway exchange catheter" and its length is 83cm: cookmedical.com/products/cc_ca…
This seems counterintuitive: if you can put the tube in with the intubating stylet, why can't you take it out and replace it? This is because when you intubate with the Eschmann, you don't need control of the stylet on both ends (like a CVC guidewire)
When inserting the ETT you just hold the distal end of the stylet and push the tube forward over it, and any error will push the stylet further into the airway. Like in this video from #EMCrit:
When you reverse the process, and withdraw a tube over the bougie, you risk dragging the bougie out of the airway, so you need control of it at all times. As the diagram makes clear, when the tube clears the proximal end of the bougie, you have to hold the center of it
But the center of it is down at or in the patient's mouth. If you retract the bougie to be able to grab it in the center, the bougie is dangerously close to exiting the glottis and in my experience *WILL* exit the glottis
This is why it's called the Eschmann *INTUBATING* stylet, and why Cook makes a specific *Airway Exchange Catheter* which is 13cm longer. It also goes without saying that you should never do this blindly and always visualize the airway with VL during the process.
If you don't have an airway exchange catheter, the safest thing is to just extubate and reintubate the patient under direct or video visualization, after making careful note of the original intubation record and any difficulties encountered.
Finally, remember: a patient with a cuff leak has an airway. A compromised one perhaps, but it's an airway. If you bungle the tube exchange, they will have the biggest leak you have ever seen: the one that arises from the tube being positioned out of the airway.
#airwaymanagement #tubeexchange #endotrachealintubation #intubation #endotrachealtube #anesthesia #pulmcrit #PCCM #eschmannstylet #airwayexchangecatheter #intubatingstylet
Look at 28cm mark. total length may be closer to 30 cm without the connector interface, but the points still stand 
It has been pointed out that this can be done, by cutting the ETT, lubing the bougie, and in this video, operating down in the mouth (unknown lengths) - I maintain that it is dicey, and if you don't know exactly what you're doing, avoid it.
Note also in the above video that all that room that he needs to operate in the mouth to grab the tube "down there" precludes #laryngoscopy during the exchange, forcing him to "go blind". I don't like it one bit. Too little room for error.
"CANNOT" is too strong a word. You can, but with high inherent danger, so you shouldn't, says me.
• • •
Missing some Tweet in this thread? You can try to
force a refresh






