Oral boards for #RadOnc are approaching. Here is advice to anyone taking the exam.
@ARRO_org @ASTRO_org @ACRORadOnc @ACROresident
@ARRO_org @ASTRO_org @ACRORadOnc @ACROresident
1, #RadOnc oral boards are the most clinically relevant exams (vs rad bio, physics, written exam, inservice, etc).
Many of the questions about management come straight from @NCCN guidelines, so use these as a primary reference.
Many of the questions about management come straight from @NCCN guidelines, so use these as a primary reference.
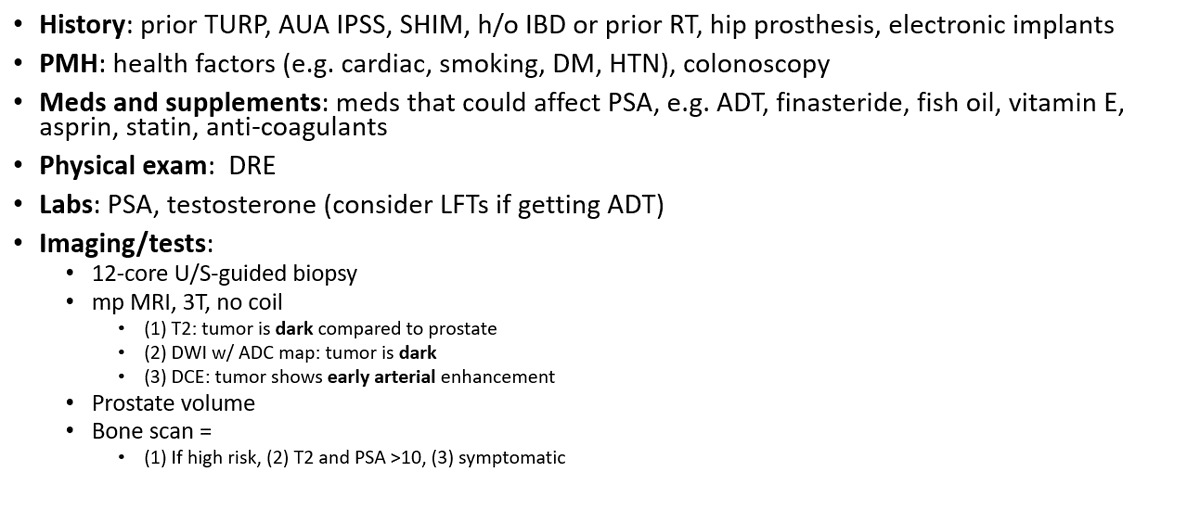
2, have a prepared script of what to say for standard questions. eg, workup, setup, margins, doses
Here is an example for prostate ca history / workup
#pcsm
Here is an example for prostate ca history / workup
#pcsm
3, if there is a metric to assess symptoms, use the metric.
Eg,
🚫“I will ask about GU symptoms”
✅ "I will use the AUA IPSS to assess GU bother symptoms"
Otherwise, the examiner will not know exactly what you are referring to, and it will take extra time to get the info.
Eg,
🚫“I will ask about GU symptoms”
✅ "I will use the AUA IPSS to assess GU bother symptoms"
Otherwise, the examiner will not know exactly what you are referring to, and it will take extra time to get the info.

4, Answer just the question being asked, succinctly.
There is no need to go off on tangent about other treatments, cancers, etc.
There is no need to go off on tangent about other treatments, cancers, etc.
5, when recommending a treatment strategy, consider pausing to say “this pt has cancer X, stage X, risk group X. Based on @NCCN guidelines, my recommended tx is X.”
6, do not go off on a tangent to say “there was a study…”
You examiner may have been on the study and will follow up with a bunch of questions about it.
You examiner may have been on the study and will follow up with a bunch of questions about it.
7, Your goal is to get through as many cases as you can in each session. Eg, aim for 5-6.
If you can only get through 1 case because you spent the whole time discussing workup, it doesn't let the examiner evaluate your understanding of management.
If you can only get through 1 case because you spent the whole time discussing workup, it doesn't let the examiner evaluate your understanding of management.
8, questions are at different difficulty levels. Examiners may keep asking more details until you don’t know.
Lower level = anatomy.
Mid level = stage, treatment options, doses.
Higher level = chemo doses, prep.
You're not always expected to know every high level question.
Lower level = anatomy.
Mid level = stage, treatment options, doses.
Higher level = chemo doses, prep.
You're not always expected to know every high level question.
9, If you don’t know, say you don’t know and you would look it up. You don’t want to recommend the incorrect treatment for the pt.
10, In general, “I would let my dosimetrist/physicist/etc figure this out” is never the right answer.
11, sometimes, the best dose is 0 Gy (i.e., observation)
12, know a guideline concordant dose and constraint set. There are often multiple options, but you may be able to just talk about one that you are comfortable with.
eg, options for prostate ca #pcsm
Thanks to @DrSpratticus for integrating this in @NCCN guidelines
eg, options for prostate ca #pcsm
Thanks to @DrSpratticus for integrating this in @NCCN guidelines

13, say that you will discuss the pt's case at tumor board.
That's what radoncs normally do anyway :-)
That's what radoncs normally do anyway :-)
14, moderate hypofractionation (vs conventional 2 Gy fractions) has become the standard of care for multiple disease sites, eg breast, prostate.
https://twitter.com/NicholasZaorsky/status/1270340517704892418
15, for some disease sites, there is a condensed formula for treatment.
Well done, @jryckman3
Well done, @jryckman3
https://twitter.com/jryckman3/status/1521192064448446467
16, If you don't want to memorize dose ranges, consider picking a number in the range
Thanks @drbeckta
Thanks @drbeckta
https://twitter.com/drbeckta/status/1521224880817065984
17, study with a group and do a ton of cases.
It helped me immensely to have experts like @DanTrifMD ask me about CNS cases and @LeilaTchelebi ask about GI cases.
It helped me immensely to have experts like @DanTrifMD ask me about CNS cases and @LeilaTchelebi ask about GI cases.
18, for younger patients, always consider fertility preservation, treatment impact on GU organs
19, do mock oral boards.
Your residency program should have mock oral exams.
Additionally, some programs have awesome formal mock orals (eg, U Maryland) for anyone in the US.
@MarkMishraMD @SbrtSean
Your residency program should have mock oral exams.
Additionally, some programs have awesome formal mock orals (eg, U Maryland) for anyone in the US.
@MarkMishraMD @SbrtSean
20, for locally advanced definitive chemo RT cases when not meeting dose constraints (eg head and neck, near brainstem), consider:
1, neoadjuvant chemo, assess response
2, resim after a few weeks
3, decrease PTV margin
1, neoadjuvant chemo, assess response
2, resim after a few weeks
3, decrease PTV margin
21, Address emergent issues first. eg, bladder cancer, and CT shown has this, what next?
Address hydronephrosis, eg w stent, before talking about tx options.
Otherwise, your next prompt will be "pt was hospitalized with mental status changes."
Address hydronephrosis, eg w stent, before talking about tx options.
Otherwise, your next prompt will be "pt was hospitalized with mental status changes."

22, for any diagnostic test during workup, ask to compare to prior tests.
eg:
lung ca screening CT
breast ca mammogram
prostate ca PSA
eg:
lung ca screening CT
breast ca mammogram
prostate ca PSA
• • •
Missing some Tweet in this thread? You can try to
force a refresh