1/ Attending: “Sam, what is the level of bilirubin at which scleral icterus is noticeable?”
Sam thinking: [1. I can make a guess, but 2. Who cares?]
Seem like a familiar scenario? Let’s help this attending ask a better question.
Sam thinking: [1. I can make a guess, but 2. Who cares?]
Seem like a familiar scenario? Let’s help this attending ask a better question.

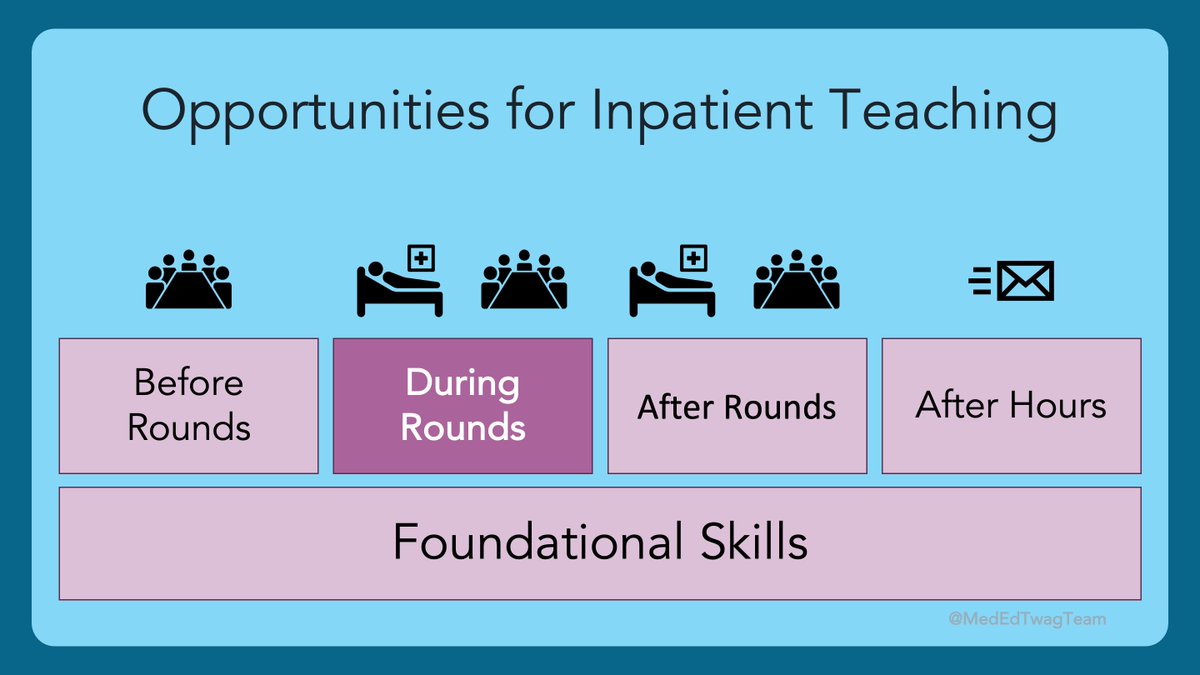
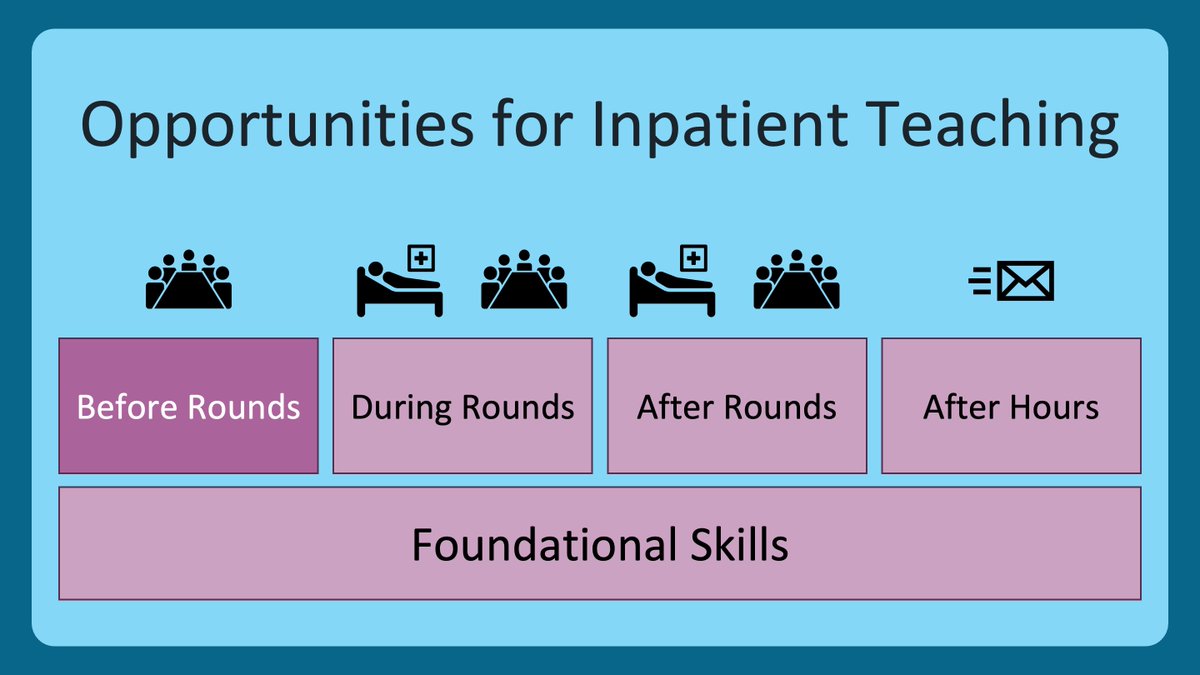
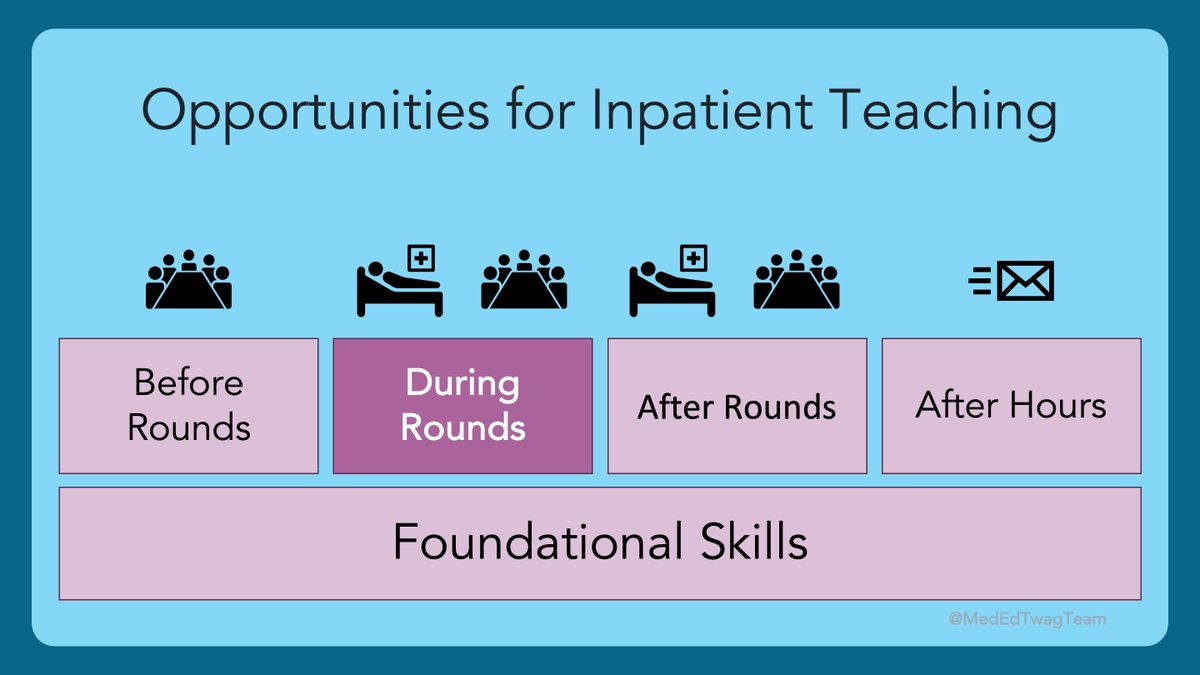
2/ Whether it is in the team room, or at the bedside, asking questions of learners is a skill that requires intention, preparation, and execution. These best practices were a topic I covered a while back, so this will be a refresher. 
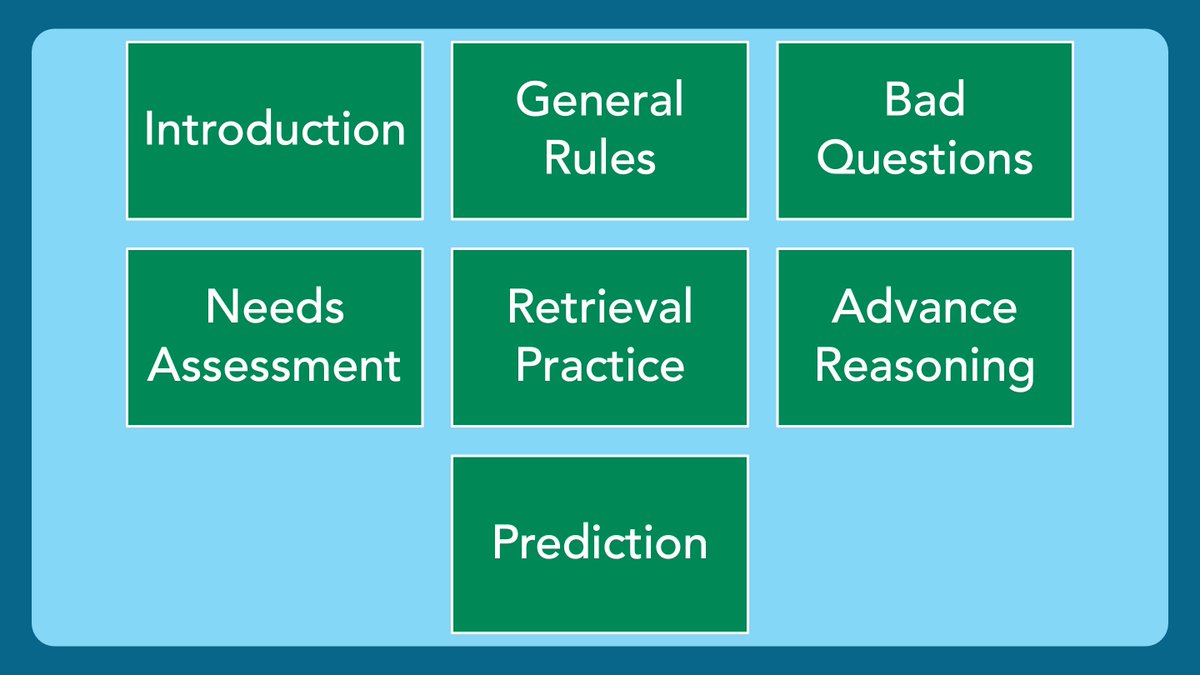
3/ These were all the topics that were covered in that series. Each individual thread can be found here:
twitter.com/i/events/13982…
twitter.com/i/events/13982…
4/ In the intro we talked about ”pimping” and the psychologically dangerous environment it creates, as illustrated by these drawings in this fascinating study:
pubmed.ncbi.nlm.nih.gov/31084222/
pubmed.ncbi.nlm.nih.gov/31084222/

5/ In the @MedEdTwagTeam’s quest to create #PsychologicallySafety in clinical learning environments, we do not condone the practice, nor the term itself.
”Pimping” has got to go!
CC: @kelseycpriest
pubmed.ncbi.nlm.nih.gov/31578151/
”Pimping” has got to go!
CC: @kelseycpriest
pubmed.ncbi.nlm.nih.gov/31578151/

6/ Inquiry, however, is a very valuable tool to promote learning in the clinical setting when used thoughtfully. These are the 8 general rules I follow when asking questions. Check out the whole thread for details. 

7/ We then detailed how even educators with the best of intentions can make a learning environment uncomfortable when they ask questions that are too specific. 

8/ Our first specific purpose for asking questions was to perform a needs assessment of your learner(s), i.e. finding out what they know and don’t know, so you can fill in the gaps. 

9/ We then cited the book #MakeItStick when discussing retrieval practice. Rather than asking learners to recall what they learned in their preclinical years, I ask them to recall what they learned while we worked together. This way, I know they have been exposed to the material. 

10/ Next, we talked about using #BloomsTaxonomy as a framework for thinking about advancing a learner’s reasoning. Once you feel they have a good grasp of a concept at the remember/understand level, push them into the areas of higher cognitive effort/learning. 

11/ We then overlayed the concept of Vygotsky’s Zone of Proximal Development or #ZPD. Identifying the bounds of a learner’s current abilities and supporting them in the #ZPD is key to promoting growth. 

12/ Lastly, I cited the book #SmallTeaching when discussing prediction as a fun and effective way to prepare a learner’s mind for deeper learning. There are emotional and cognitive reasons why this tool is effective. 

13/ But, prediction alone is not enough. After a prediction, one must soon determine whether the prediction was accurate or not. Next, reflection is necessary to solidify reasoning that led to an accurate prediction, or correct thought processes that led to a misguided guess. 

14/ Thanks for joining us for this review of one of my favorite topics. A topic that can only be surpassed by Feedback. But lucky for us, @JenniferSpicer4 will be back in 2 weeks to remind us about best practices.
Tweet you then!
Tweet you then!

• • •
Missing some Tweet in this thread? You can try to
force a refresh