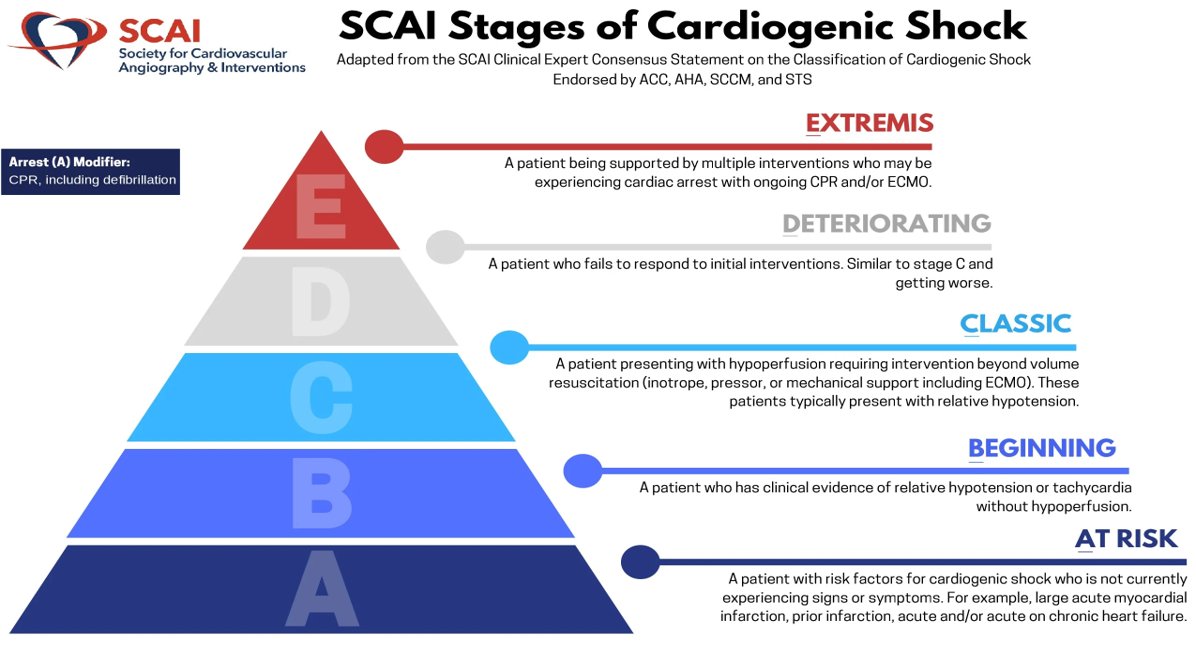
3/ A little out of the realm of this thread, #Impella and other mechanical circulatory support are part of a larger strategy to treat cardiogenic shock. Check out the @SCAI classification system below for more information


https://twitter.com/SCAI/status/1143607245349019648?s=20&t=vCfwbaZnebppfO1VxPQbTA

4/ Impellas are placed via femoral or axillary artery, into the aorta, & across the aortic valve. There is an inlet on the LV side and an outlet on the aortic side. There are a number of different Impellas, each of which have different flow rates, lumen size, and access needs. 👇 

5/ However, the structural design Impellas is grossly similar. The tip of the catheter has a flexible pigtail, intended to prevent mechanical injury of the ventricle (absent on the larger LD and 5.5 models). Important- look at the flow rate, up to 5 LPM with the 5.5! 🤯 

6/ So how does it help? Looking at Pressure-Volume loops with Impella support, the shape goes from a 🟦 to a 🔺 2/2 continuous assisted LV outflow via the pump. As more power (P-level) is added, flow via the Impella ⬆️ and the triangle becomes more distinct. 

7/ A triangle forms because the Impella is continuously unloading the LV & doing the mechanical work of moving blood from LV to Ao. Unlike other devices it produces a triangular pressure-volume area that is shifted to the left with a smaller pressure-volume area 

8/ In short, this is important because the Impella:
⬆️ Cardiac output & end-organ perfusion (including the ❤️)
⬇️Myocardial oxygen consumption
⬇️ End-diastolic volume and pressure (LV unloading)
And... breaks the cycle of cardiogenic shock!
⬆️ Cardiac output & end-organ perfusion (including the ❤️)
⬇️Myocardial oxygen consumption
⬇️ End-diastolic volume and pressure (LV unloading)
And... breaks the cycle of cardiogenic shock!

9/ Don't worry, I'll be back to follow up on the Impella Console, complications to look out for in the ICU (and management tips), anticoagulation, weaning, and a little #POCUS.
Thoughts? Comments? I want to learn from YOU and all the experienced folks out there! Thank you! 🙏
Thoughts? Comments? I want to learn from YOU and all the experienced folks out there! Thank you! 🙏
10/ @MortonKern @eaa5683 @EMinMiami @MRamzyDO @NickJohnsonMD @JenelleBadulak @NavinKapur4 @JumeanMarwan @emcrit @critcareguys @CriticalCareNow @critconcepts @iceman_ex @sbattrawden @IM_Crit_ @Thind888 @emily_fri @anesthesiacbf10 @rishikumarmd @reverendofdoubt @PulmCrit
• • •
Missing some Tweet in this thread? You can try to
force a refresh