1/ A tweetorial- Watchman Left Atrial Appendage Occlusion!
#LAAO #Watchman #StructuralHeartDisease #EPeeps #interventionalcardiology @EPeeps_Bot @RadialFirstBot @EchofirstB @BotPci @TAVRBot
#LAAO #Watchman #StructuralHeartDisease #EPeeps #interventionalcardiology @EPeeps_Bot @RadialFirstBot @EchofirstB @BotPci @TAVRBot

2/ what is the left atrial appendage?
The LAA is derived from the left wall of the primary atrium (embryo). Its diff from the true LA and its suited to function as a decompression chamber during left ventricular systole and during other periods when left atrial pressure is high
The LAA is derived from the left wall of the primary atrium (embryo). Its diff from the true LA and its suited to function as a decompression chamber during left ventricular systole and during other periods when left atrial pressure is high

3/ the appendage is like your fingerprint. No two are the same.
Common shapes are:
🥦Cauliflower/Broccoli (hardest)
💨Windsock (easiest)
🐓Chicken wing
🌵Cactus
#LAAO #Watchman #Structural #Cardiotwitter #EPeeps @EPeeps_Bot @TAVRBot @RadialFirstBot @EchofirstB
Common shapes are:
🥦Cauliflower/Broccoli (hardest)
💨Windsock (easiest)
🐓Chicken wing
🌵Cactus
#LAAO #Watchman #Structural #Cardiotwitter #EPeeps @EPeeps_Bot @TAVRBot @RadialFirstBot @EchofirstB

4/ even with its physiologic functions the LAA seems to propose more risk then benefit especially in the setting of atrial fibrillation.
About 15% of ischemic strokes arise as a result of atrial fibrillation #LAAO #Afib #CVA #stroke
Credit- Jaqueline Shaw, UBC
About 15% of ischemic strokes arise as a result of atrial fibrillation #LAAO #Afib #CVA #stroke
Credit- Jaqueline Shaw, UBC

5/ OACs work well but still carry a 2-5% major bleeding risk/yr. So many factors contribute to ⬆️ bleeding risk and unfortunately many of those same factors share territory with afib. Many patients are left with either no anticoagulation or risk of repeat bleeding events. 

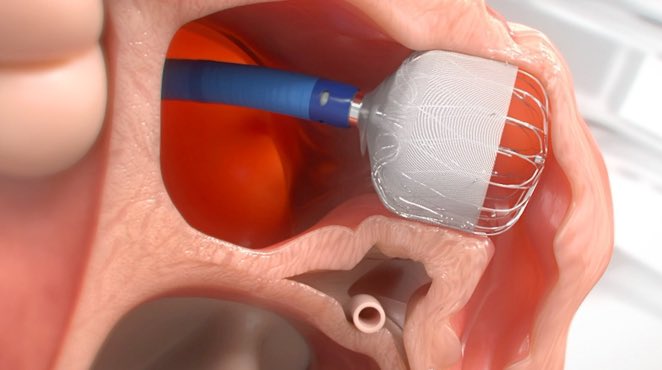
6/ enter left atrial appendage occlusion- specifically The #Watchman
This device was designed to prevent stroke in afib patients that cannot tolerate anticoagulation (long term) #LAAO #Afib

This device was designed to prevent stroke in afib patients that cannot tolerate anticoagulation (long term) #LAAO #Afib

7/Protect AF- After 3.8 yrs of f/u pts w/ nonvalvular AF ⬆️ risk for stroke, perc LAA closure met criteria for noninferiority and superiority, compared w/ warfarin, for preventing outcome of CVA, systemic embolism, and CV death, as well as superiority for CV+ all-cause mortality. 



8/ the first device was novel but had many issues. It was hard to implant, and now we are finding has issues with late leaks and possible device thrombus #Watchman #LAAO 



9/ the real winner- WATCHMAN FLX. As someone that has implanted both, this device has been the definition of a game changer. It’s easy to implant and the way it conforms the the appendage is must better than it’s previous ridged predecessor the 2.5 #LAAO @EPeeps_Bot 

10/ PINNACLE FLX, SEAL FLX, and SURPASS have very promising data. We are still awaiting CHAMPION AF data but all signs point to the Watchman FLX as being a revolutionary change to the LAA closure space. #LAAO 

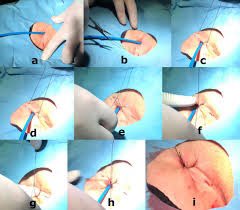
11/ implantation truthfully is all about the #transseptal. A posterior and mid/Inf transseptal is preferred to access the anteriorally located appendage.
#LAAO @adnanalkhouli @Dr_Santangeli @epTicTocDoc @DrCJBradley @RajTayalMD @chadialraies @agtruesdell

#LAAO @adnanalkhouli @Dr_Santangeli @epTicTocDoc @DrCJBradley @RajTayalMD @chadialraies @agtruesdell


12/I’ve started using the #VersiCross and man it’s an amazing way to cross. The sheath is well transitioned to get into the skin and then the moldable sheath engages the septal followed by exposure of the wire. RF ON! then push the wire forward and form a PIG tail in the LA
13/ next pick your right sheath (depends on anatomy)
12F ID and 75cm working length
➰Single curve
➿Double curve (used most often)
〰️Anterior curve
Use echo to choose. If LAA close to ventricle use single, if LAA curves towards atrium use anterior. Double- everything else

12F ID and 75cm working length
➰Single curve
➿Double curve (used most often)
〰️Anterior curve
Use echo to choose. If LAA close to ventricle use single, if LAA curves towards atrium use anterior. Double- everything else


14/ get the sheath into appendage and place your PIG 🐷 . I usually perform appendage-o-gram to help me better understand appendage, however #echofiest should be your go to for complete understanding/assessment @EPeeps_Bot @epTicTocDoc @adnanalkhouli @SachinGoelMD @yourheartdoc1
15/ Next based on echo/CT pick your size
🔸20 mm
🔹24 mm
🔸27 mm
🔷31 mm
🔶37 mm
Your goal is to aim for somewhere between 10-30% compression. Use echo for assessment. @HafizaKMD @NirmanBhatia @SachinGoelMD @doconmoney @DrMarthaGulati @ekgpdx @djc795 @heartdoc45


🔸20 mm
🔹24 mm
🔸27 mm
🔷31 mm
🔶37 mm
Your goal is to aim for somewhere between 10-30% compression. Use echo for assessment. @HafizaKMD @NirmanBhatia @SachinGoelMD @doconmoney @DrMarthaGulati @ekgpdx @djc795 @heartdoc45



16/ prep the watchman and place wet to wet into sheath. Get to the radio opaque line and pull the sheath back. FLX ball time!
This IMO has been one of the great advantages of FLX.
Keys
🔑 ball size should be about double the sheath
🔑 Notice how ball reacts, desheath or push
This IMO has been one of the great advantages of FLX.
Keys
🔑 ball size should be about double the sheath
🔑 Notice how ball reacts, desheath or push
17/ deploy your device and hold forward tension for 10 sec. TEE for
PASS criteria..
P- position (ostium)
A- anchor (tug)
S- size (compression 10-30%)
S- seal (no leak >5mm)
@adnanalkhouli @yourheartdoc1 @epTicTocDoc @EPeeps_Bot @ekgpdx @RajTayalMD @Pooh_Velagapudi
PASS criteria..
P- position (ostium)
A- anchor (tug)
S- size (compression 10-30%)
S- seal (no leak >5mm)
@adnanalkhouli @yourheartdoc1 @epTicTocDoc @EPeeps_Bot @ekgpdx @RajTayalMD @Pooh_Velagapudi
18/ Counter-clock to release. The FLX allows you to recapture and reposition as many times as you want pull everything back into the IVC. Figure 8 stitch to close. Home the same day! #LAAO #Cardiotwitter 
19/ 💊 OAC for 45 days
🔍followed by TEE or CT to confirm no device thrombus or leak
➡️then DAPT for 6 months after.
🙏🏾Hopefully coming data will let us drop the OAC 45 day post period
#Watchman #LAAO @EPeeps_Bot
🔍followed by TEE or CT to confirm no device thrombus or leak
➡️then DAPT for 6 months after.
🙏🏾Hopefully coming data will let us drop the OAC 45 day post period
#Watchman #LAAO @EPeeps_Bot
20/ I’m excited for new techniques in the field as well! 4D volume ICE for LAAO. This would eliminate the need for anesthesia and TEE!
Video courtesy of @Dr_Santangeli
#ICE #LAAO
Video courtesy of @Dr_Santangeli
#ICE #LAAO
21/ watchman is another device in the structural interventionalists tool box!
We couldn’t do it without our amazing structural imagers and coordinators! The device is safe and can change a persons life! Excited to see the field continue to evolve. #Watchman #LAAO #McLarenHeart
We couldn’t do it without our amazing structural imagers and coordinators! The device is safe and can change a persons life! Excited to see the field continue to evolve. #Watchman #LAAO #McLarenHeart

@NadeenFaza @bcostelloMD @CMichaelGibson @DocSavageTJU @pravinp8 @hpatel824 @onco_cardiology @DocStrom @venkmurthy @SureshSharmaMD @MusaSharkawi @Rahul2282Sharma @NirmanBhatia @ekgpdx @RezaEmaminia @echocardiac @ASE360 @robertomlang @ChinnaiyanMD @purviparwani @PinakShahMD
@Pooh_Velagapudi @DrMarthaGulati @mmamas1973 @MDMankad @SVRaoMD @dr_chirumamilla @willsuh76 @DrSuzyFeigofsky @rwyeh @yourheartdoc1 @DrJRicci @iamritu @DeeDeeWangMD @DrCJBradley @AkhilNarangMD @tarun_jain93 @maquinonesmd @agtruesdell @jameschilee @KhandelwalMD @HeartOTXHeartMD
@sarahhudsonuk @avolgman @rahatheart1 @DavidWienerMD @sunnyvmd @monsangh @feelingthepulse @achoiheart @akshitsharmaMD @adcaTicTocDoc @jeredcookmd @rezaemaminia @MartyTamMD @true_EP @sheelakrishmd @skilicmd @ekgpdx @chadialraies @mirvatalasnag @venkmurthy @jameschilee
@Babar_Basir @DrHooksDO @chadialraies @ZaherFanari @motownpaesano @GindiRyan @AKassier @AlQarqazM @BobRabbaniMD @SachinParikhMD @TiberioFrisoli @DrAdaStefanescu @dr_chirumamilla @noshreza @UjjwalRastogiMD @majazayeri @SanChris999 @skilicmd
@rajdoc2005 @VMJ_SVM
@rajdoc2005 @VMJ_SVM
• • •
Missing some Tweet in this thread? You can try to
force a refresh