Omicron wave of mass infection showing its impact. Too many friends & colleagues reaching out for advice on #LongCovid. Heartbreaking.
A 🧵on Rest & Pace. Biggest advice: don't repeat the mistake that most of us from the first wave in 2020 did i.e. push yourself.
1/
A 🧵on Rest & Pace. Biggest advice: don't repeat the mistake that most of us from the first wave in 2020 did i.e. push yourself.
1/
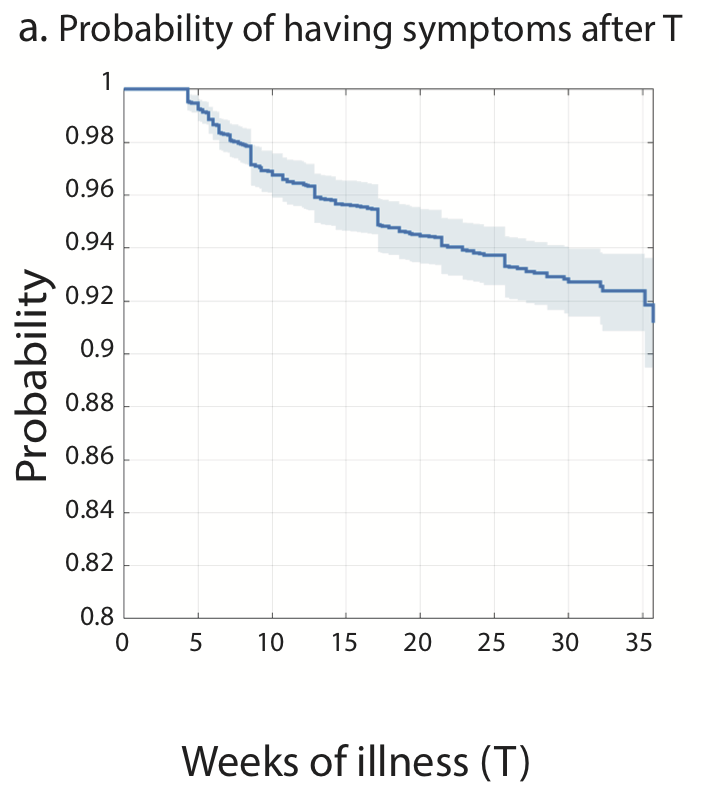
Data suggest recovery after the first few months is infrequent.
Tran et al (France)*:
-Of LC patients who were still sick at 2 months, only 15% recovered by 1 year
-Of those who thought they were better, 33% subsequently relapsed
*Non-vaccinated
2/
nature.com/articles/s4146…
Tran et al (France)*:
-Of LC patients who were still sick at 2 months, only 15% recovered by 1 year
-Of those who thought they were better, 33% subsequently relapsed
*Non-vaccinated
2/
nature.com/articles/s4146…
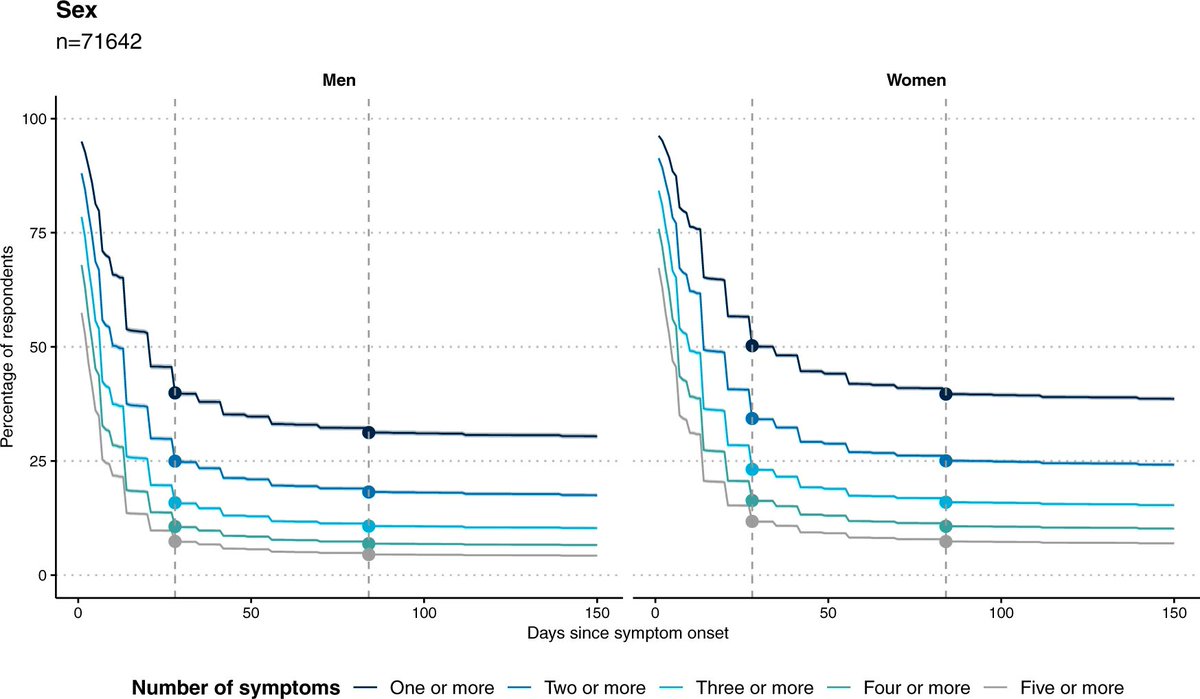
Whitaker et al (UK)*:
- A rapid drop-off in symptom reporting by 4 weeks, a further, smaller drop by 12 weeks, but then very limited further decline (for up to ~22 weeks of study duration) for both men and women.
*Non-vaccinated population
3/
nature.com/articles/s4146…
- A rapid drop-off in symptom reporting by 4 weeks, a further, smaller drop by 12 weeks, but then very limited further decline (for up to ~22 weeks of study duration) for both men and women.
*Non-vaccinated population
3/
nature.com/articles/s4146…
So, most recoveries happen in the first few months. Do your best to help your body to recover. How? By rest & rest & rest.
It's been shown eg in Ziauddeen et al that inadequate initial rest is correlated w long covid later on.
@Dr2NisreenAlwan, @Know_HG
4/
journals.plos.org/plosone/articl…
It's been shown eg in Ziauddeen et al that inadequate initial rest is correlated w long covid later on.
@Dr2NisreenAlwan, @Know_HG
4/
journals.plos.org/plosone/articl…
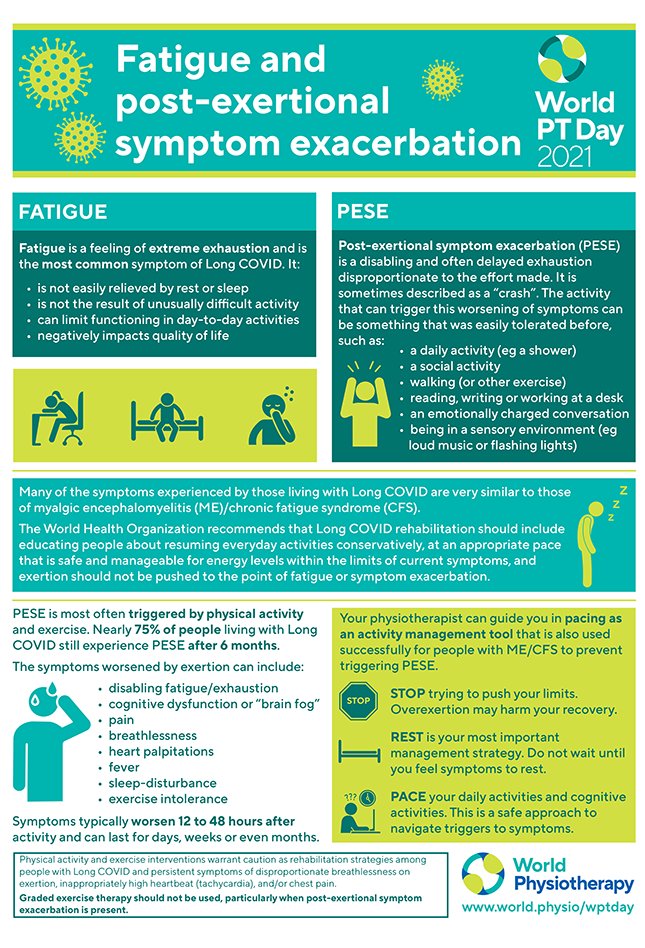
The mistake most of us from the first wave in Spring 2020 did was to exert ourselves, because we didn't know any better, because we were told to do so. This causes Post Exertional Symptom Exacerbation (PESE) or Post Exertional Malaise (PEM) that #pwME knew about all along!
5/
5/
Yes, PEM/PESE is a very well known concept among #pwME and actually is the cardinal symptom for #MECFS diagnosis. Before the COVID-19 pandemic it was 10.4 times more likely to happen in ME/CFS than control groups.
journals.sagepub.com/doi/full/10.11…
6/
journals.sagepub.com/doi/full/10.11…
6/
For those unfamiliar w/ PEM: being sedentary doesn't explain the activity intolerance. In VanNess et al, within 24hrs of the test, 85% of controls fully recovered vs 0% of #pwME. The remaining 15% of control recovered within 48hrs vs only 1 ME patient
7/
pubmed.ncbi.nlm.nih.gov/20095909/
7/
pubmed.ncbi.nlm.nih.gov/20095909/
Initial cases of #LongCovid did not know about PEM/PESE.
In an urge to return to our 'normal' life, we were pushing our way towards pre infection baseline only to find ourselves more and more ill.
Until we stopped, listened, read and learned from the #MECFS community.
8/
In an urge to return to our 'normal' life, we were pushing our way towards pre infection baseline only to find ourselves more and more ill.
Until we stopped, listened, read and learned from the #MECFS community.
8/
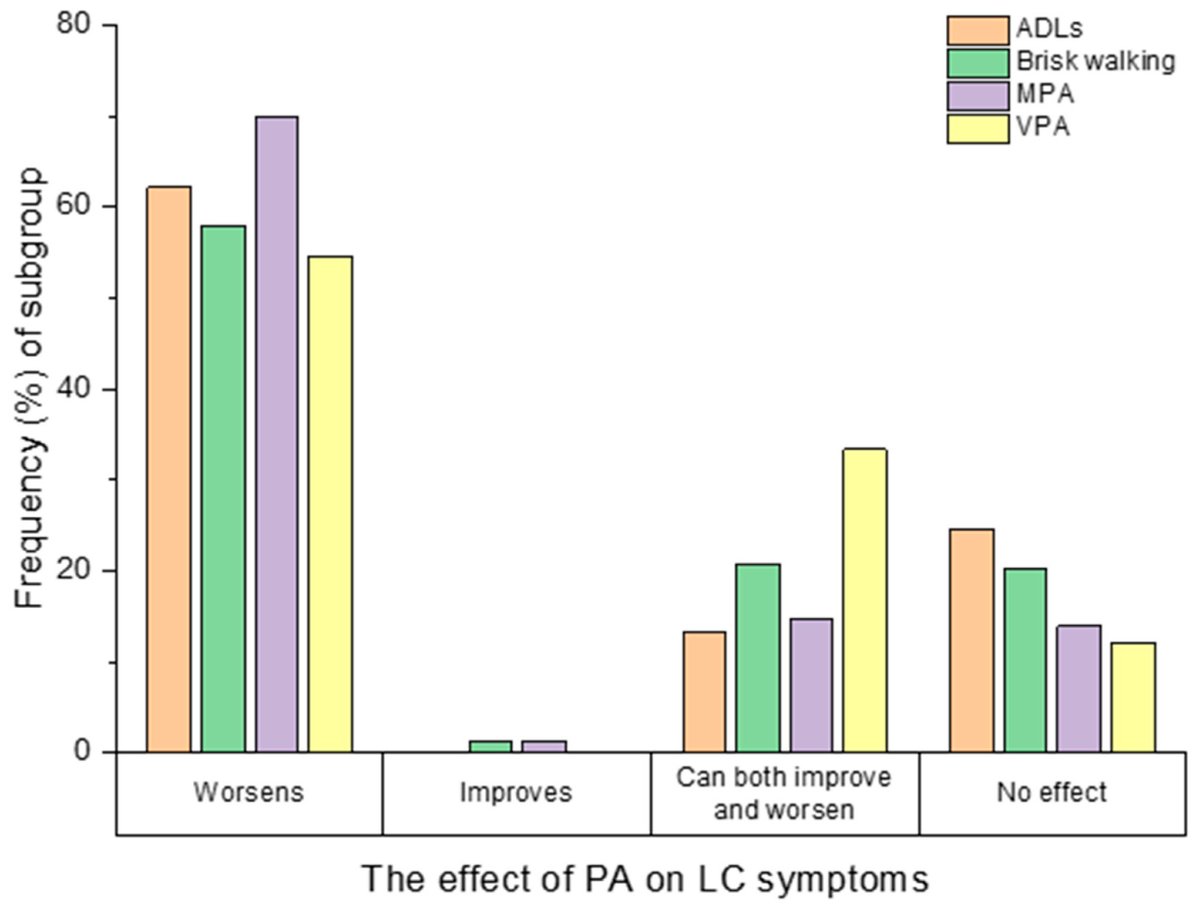
In a cross-sectional study (of 477 participants mean age 45 years, median Long Covid duration was 383.5 days) Wright et al found that physical activity worsened symptoms in 74.84% of participants.
9/
mdpi.com/1660-4601/19/9…
9/
mdpi.com/1660-4601/19/9…
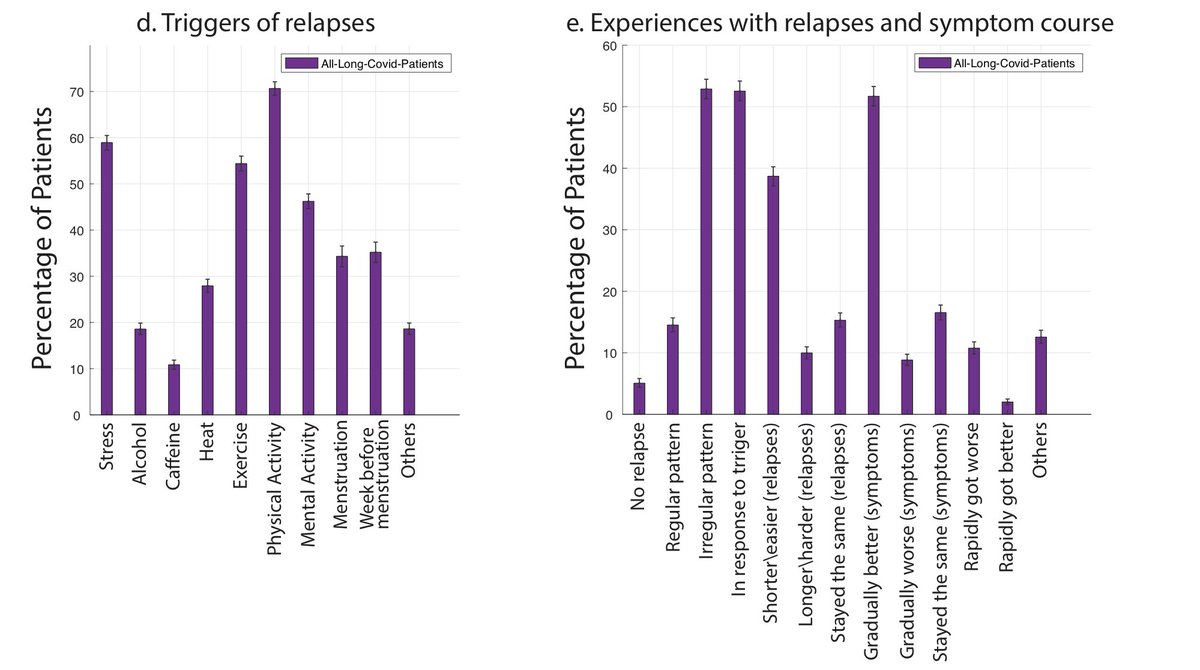
This is similar to what we @patientled had identified before - 89.1% of participants reported experiencing either physical or mental PEM/PESE.
10/
10/
https://twitter.com/AthenaAkrami/status/1343166471938203649?t=-J8VISSR2wYg9H2-JZRgqg&s=19
well, my thread had 20 tweets. It seems @Twitter ate the second half, and doesn't cough it up ... will add them later
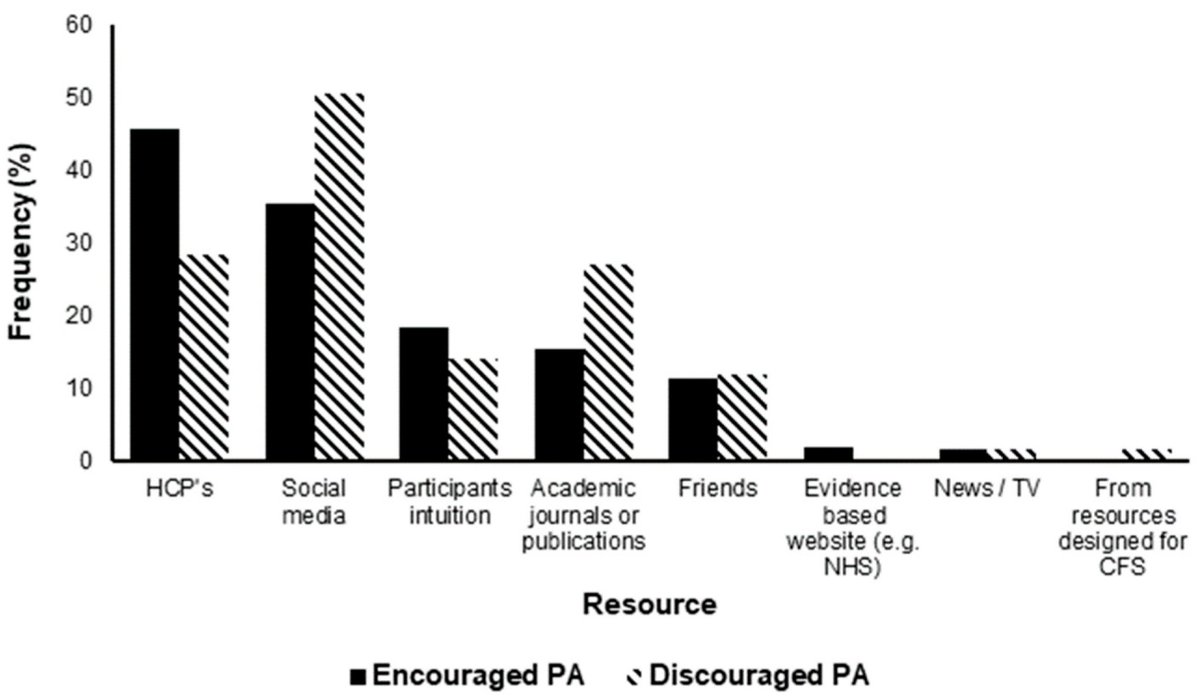
According to Wright et al, unfortunately most of these harmful activities were recommended by health care providers!
Our intuitions are wrong too, since we're biased to think exercise can only do good.
Academic paper & social media know it, thanks to #MECFS
11/

Our intuitions are wrong too, since we're biased to think exercise can only do good.
Academic paper & social media know it, thanks to #MECFS
11/
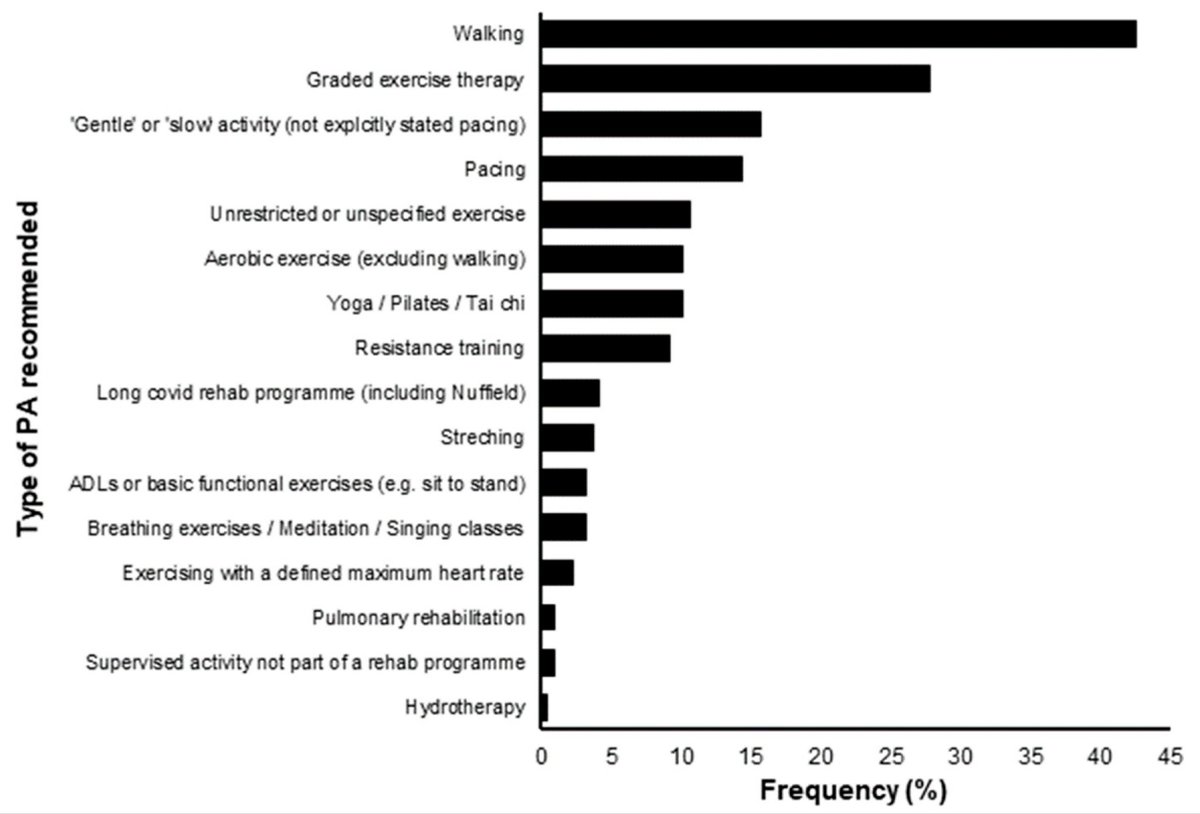
No matter how light or heavy these activities are, they can exacerbate symptoms.
ADLs: Activities of Daily Living
MPA: Moderate Physical Activity
VPA: Vigorous Physical Activity
12/

ADLs: Activities of Daily Living
MPA: Moderate Physical Activity
VPA: Vigorous Physical Activity
12/

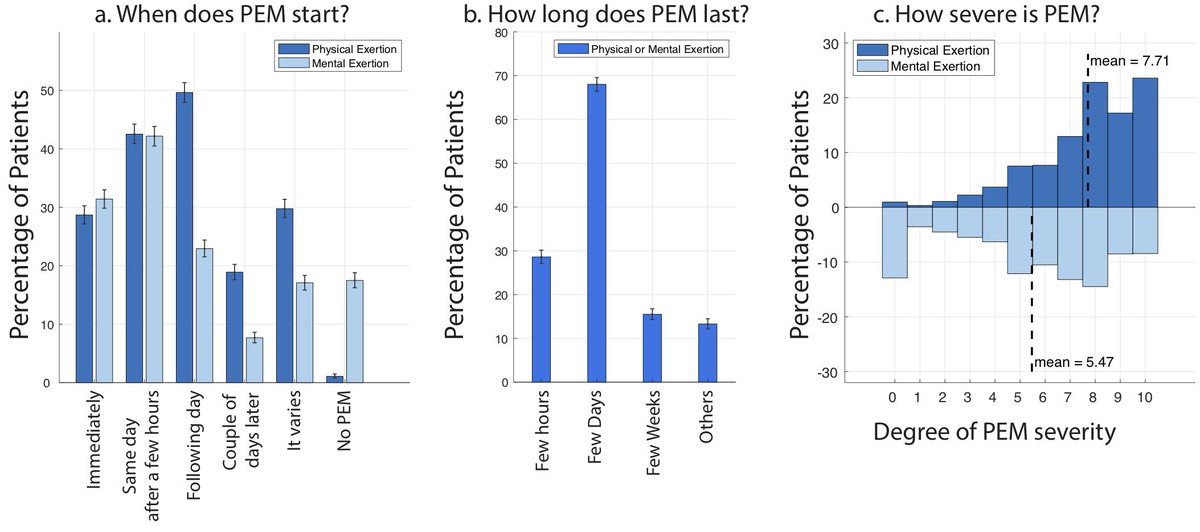
Trickiest thing about PEM/PESE is that symptom exacerbation is usually delayed (few hours, next day) after the trigger. This makes it very difficult to see the pattern and detect the triggers.
And again, triggers are varied and can be both mental and physical.
13/

And again, triggers are varied and can be both mental and physical.
13/
@PutrinoLab has two excellent threads on different types of PEM/PESE.
1. Metabolic-led, where metabolic dysfunction and cell exhaustion can cause a vicious cycle of inflammation, tissue hypoxia and symptom exacerbation.
13/
1. Metabolic-led, where metabolic dysfunction and cell exhaustion can cause a vicious cycle of inflammation, tissue hypoxia and symptom exacerbation.
13/
https://twitter.com/PutrinoLab/status/1523428750309830656?t=FsB4scj45-19gc35vWiydQ&s=19
2. Autonomically-led PESE/PEM, where autonomic nervous system is under strain.
It's quite important to distinguish these two, particularly if you have signs of #POTS or Dysautonomia.
14/
It's quite important to distinguish these two, particularly if you have signs of #POTS or Dysautonomia.
14/
https://twitter.com/PutrinoLab/status/1525172494709182464?t=xpr-dzE4XEXaerkGca_agw&s=19
@LongCOVIDPhysio has a lot of good resources on rehabilitation, fatigue, and exercise. You need to respect your energy envelope and pace accordingly.
15/

15/

You can also join support groups
- Body Politic (@itsbodypolitic, on slack)
- Long Covid Support Group (@long_covid)
where members share a wealth of experience and knowledge on how to navigate pacing and avoid frequent crashings.
17/
- Body Politic (@itsbodypolitic, on slack)
- Long Covid Support Group (@long_covid)
where members share a wealth of experience and knowledge on how to navigate pacing and avoid frequent crashings.
17/
So, if you've had Omicron recently and are still struggling with lingering symptoms, first: I'm really sorry. Second: show down, rest and make it your priority to recover before it's too late.
Of course rest alone is not enough (depending on the damage), but it's essential.
18/
Of course rest alone is not enough (depending on the damage), but it's essential.
18/
In another thread, I'll try to summarize what we know, so far, about LC sub-categories. No matter the underlying pathophysiology, pacing is essential.
#LongCovid sucks. It literally sucks life & energy out of Every Single Cell of your body. Avoid it. Wear 😷, avoid infection
19
#LongCovid sucks. It literally sucks life & energy out of Every Single Cell of your body. Avoid it. Wear 😷, avoid infection
19
• • •
Missing some Tweet in this thread? You can try to
force a refresh