🧵Our latest in @BloodJournal
@coleman_lindsley @c_j_gibson @DanaFarberNews
Older patients with AML undergoing HCT have high rates of relapse & non-relapse mortality
We investigated how outcomes relate to both baseline characteristics and molecular MRD
tinyurl.com/4bn76ham
@coleman_lindsley @c_j_gibson @DanaFarberNews
Older patients with AML undergoing HCT have high rates of relapse & non-relapse mortality
We investigated how outcomes relate to both baseline characteristics and molecular MRD
tinyurl.com/4bn76ham
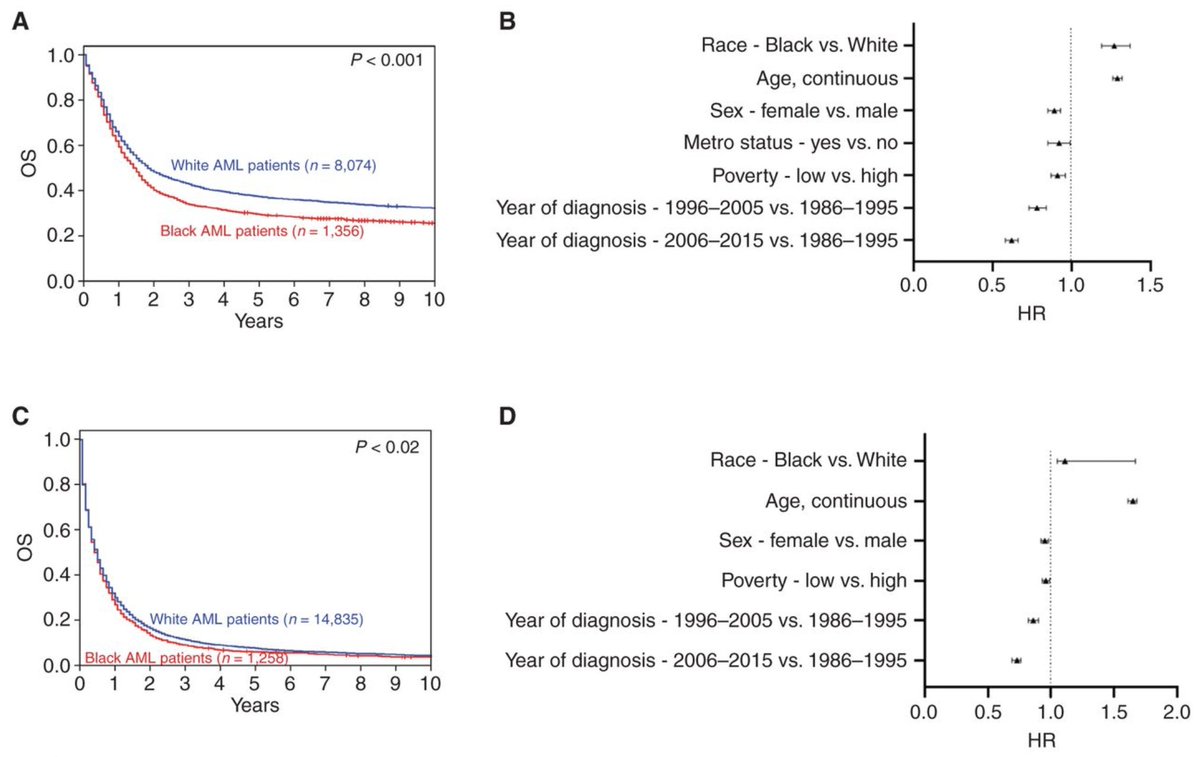
2. @DrChrisHourigan and others have shown that AML pts with mutations at remission (molecular MRD) have more relapse➡️ inferior survival after HCT, especially if receiving reduced intensity conditioning.
tinyurl.com/23rrbjte
tinyurl.com/23rrbjte

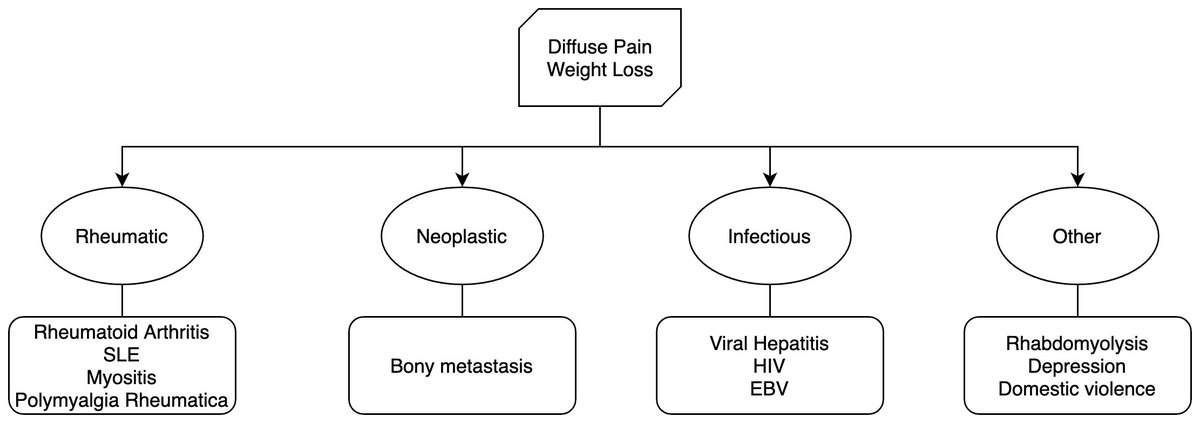
3. We wondered:
1⃣ Is prognostic impact of MRD the same for patients age ≥ 60 (underrepresented in RCTs)?
2⃣ Is mutation persistence related to features present at diagnosis?
1⃣ Is prognostic impact of MRD the same for patients age ≥ 60 (underrepresented in RCTs)?
2⃣ Is mutation persistence related to features present at diagnosis?
4. In 295 pts age ≥ 60 undergoing HCT in CR1, we combined baseline AML genetics and clinical variables to stratify into 4 groups with distinct risk post HCT: 

5. 192 of these pts had a CR1 sample. Comparing to dx allowed us to know which mutations were new vs old.
Mutations present at AML dx persisted in 80% of pts assessed.
In a minority, persistent mutations were only in DNMT3A or TET2, but most had at least one other (“MRD+”).
Mutations present at AML dx persisted in 80% of pts assessed.
In a minority, persistent mutations were only in DNMT3A or TET2, but most had at least one other (“MRD+”).

6. Likelihood of being MRD+ was associated with:
▪️ Secondary-type genetics (as defined here tinyurl.com/3humfzfx)
▪️ TP53 mutations
▪️ Poor risk cytogenetics
Makes sense - all of these features are associated with therapeutic resistance.
▪️ Secondary-type genetics (as defined here tinyurl.com/3humfzfx)
▪️ TP53 mutations
▪️ Poor risk cytogenetics
Makes sense - all of these features are associated with therapeutic resistance.
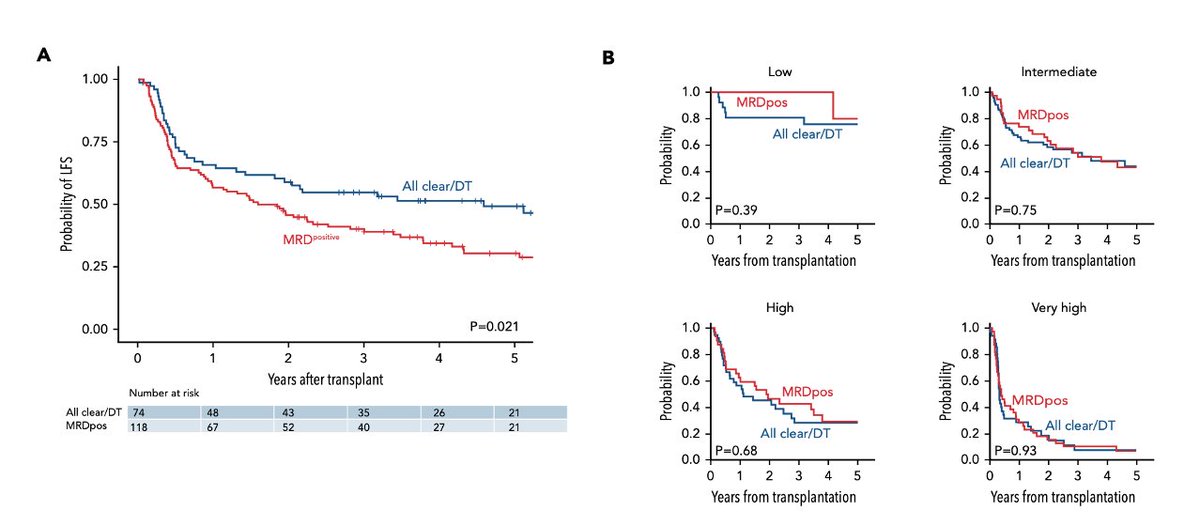
7. In univariable analysis, MRD+ patients had inferior survival.
But...
After considering baseline risk, there was no difference between MRD+ and MRD- patients’ survival.
But...
After considering baseline risk, there was no difference between MRD+ and MRD- patients’ survival.
8. How do we square this with 09-01 findings referenced above? Two thoughts:
First - maybe MRD+ has different impact in our pts than younger RCT-eligible population in 09-01.
Older pts: MRD+ often reflects underlying MDS?
Younger pts: MRD+ more often reflects persistent AML?
First - maybe MRD+ has different impact in our pts than younger RCT-eligible population in 09-01.
Older pts: MRD+ often reflects underlying MDS?
Younger pts: MRD+ more often reflects persistent AML?
9. Second – perhaps for many, MRD+ is a reflection of disease-intrinsic risk, encoded by genetic features:
Chemoresistant AML is more likely to persist after induction
But when comparing to pts with similar baseline risk, MRD+ doesn’t confer additional prognostic information.
Chemoresistant AML is more likely to persist after induction
But when comparing to pts with similar baseline risk, MRD+ doesn’t confer additional prognostic information.
10. MRD in AML is complicated & large prospective studies like MEASURE @CIBMTR clinicaltrials.gov/ct2/show/NCT05… & academia-industry-@US_FDA partnerships through @FNIH_Org biomarkers consortium will help bring rational MRD approaches forward into clinical practice
tinyurl.com/2p8mrwcs
tinyurl.com/2p8mrwcs
11. Many thanks to our collaborators across 6 transplant centers, including @pankitvachhani
@bryanhambley1 @DrMiguelPerales @EuniceWangMD
@LukaszPGondek @DrStevenDevine and others not on twitter!
+ Funding from @ASH_hematology
@bryanhambley1 @DrMiguelPerales @EuniceWangMD
@LukaszPGondek @DrStevenDevine and others not on twitter!
+ Funding from @ASH_hematology
12. Lastly, this project has spanned medical school and residency. Could not have completed this project successfully without the incredible mentorship from @ColemanLindsley and @c_j_gibson in addition to the @DanaFarberNews Bone Marrow Transplant team.
#leusm #bmtsm #MedTwitter
#leusm #bmtsm #MedTwitter
• • •
Missing some Tweet in this thread? You can try to
force a refresh