Medical Therapy for Functional #MR
#GDMT is the first step and prevails as the mainstay in the treatment of #FMR
This review addresses the medical Tx options for FMR Mx and highlight a targeted approach for each FMR category
#HeartFailure #VHDs ahajournals.org/doi/10.1161/CI… @CircHF

#GDMT is the first step and prevails as the mainstay in the treatment of #FMR
This review addresses the medical Tx options for FMR Mx and highlight a targeted approach for each FMR category
#HeartFailure #VHDs ahajournals.org/doi/10.1161/CI… @CircHF


#GDMT plays a pivotal role in LV reverse remodeling (LVRR) in FMR and leads to reduction in severity and improved outcomes for both atrial and ventricular #FMR
#GDMTWorks #VHDs #HeartFailure
#GDMTWorks #VHDs #HeartFailure
Studies report 28% to 50% reduction in grade of #FMR from baseline in patients receiving optimal or maximally tolerated doses of #GDMT (including diuretics) in both ischemic #cardiomyopathy and non-ischemic CMP
#GDMTWorks #VHDs #MR
#GDMTWorks #VHDs #MR
GDMT optimization must be prioritized in all patients with #FMR in an attempt to achieve target doses as attained in clinical trials
#GDMTWorks #VHDs #HeartFailure #CardioTwitter #CardioEdu
#GDMTWorks #VHDs #HeartFailure #CardioTwitter #CardioEdu
In #HFrEF patients with ventricular FMR, it consists of #RAASi preferentially #ARNI, #BBs with most evidence available for #carvedilol, #MRA with clearer evidence for spironolactone, #SGLT2i, and when appropriate consideration of ivabradine, hydralazine, and vericiguat.
For patients with ischemic MR and #HFpEF, consideration for #revascularization and CAD medical treatment are appropriate.
Patients with #HFmrEF and ventricular FMR seem to derive benefit from similar regimen as #GDMT for HFrEF, with most evidence for #BBs, #ARNI/ #ARB, and #MRA
Patients with #HFmrEF and ventricular FMR seem to derive benefit from similar regimen as #GDMT for HFrEF, with most evidence for #BBs, #ARNI/ #ARB, and #MRA
For Atrial #MR and #AF, restoration of sinus rhythm when feasible is advised, and RAASi Rx when concurrent indications exist
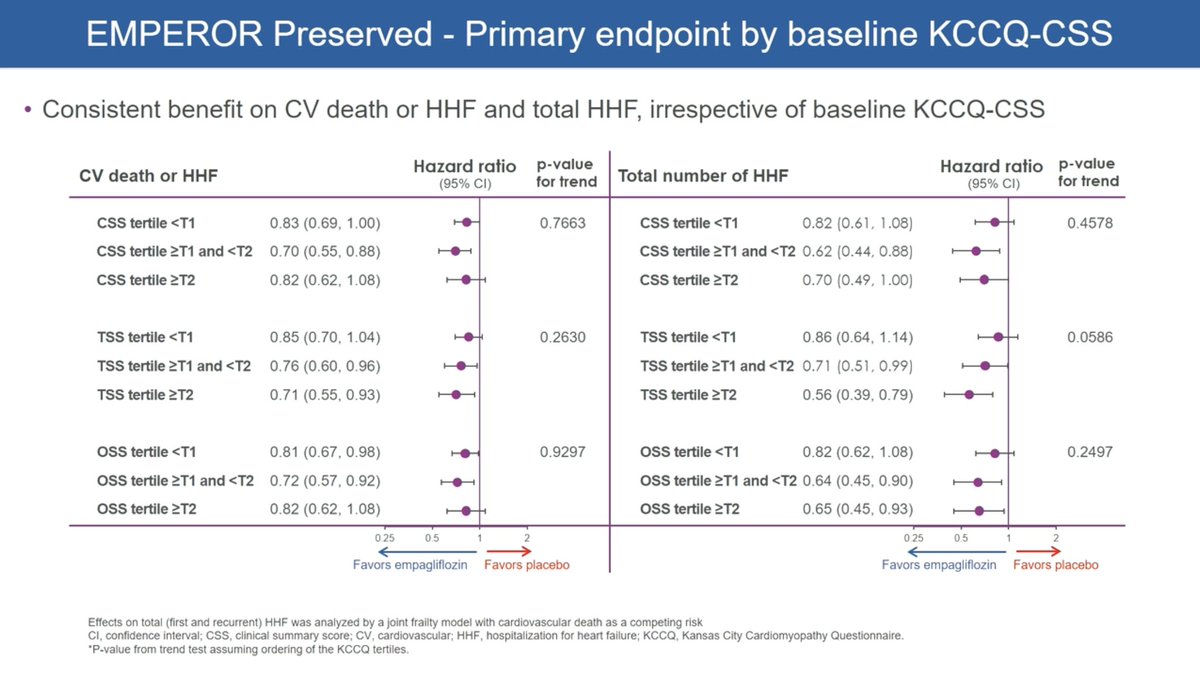
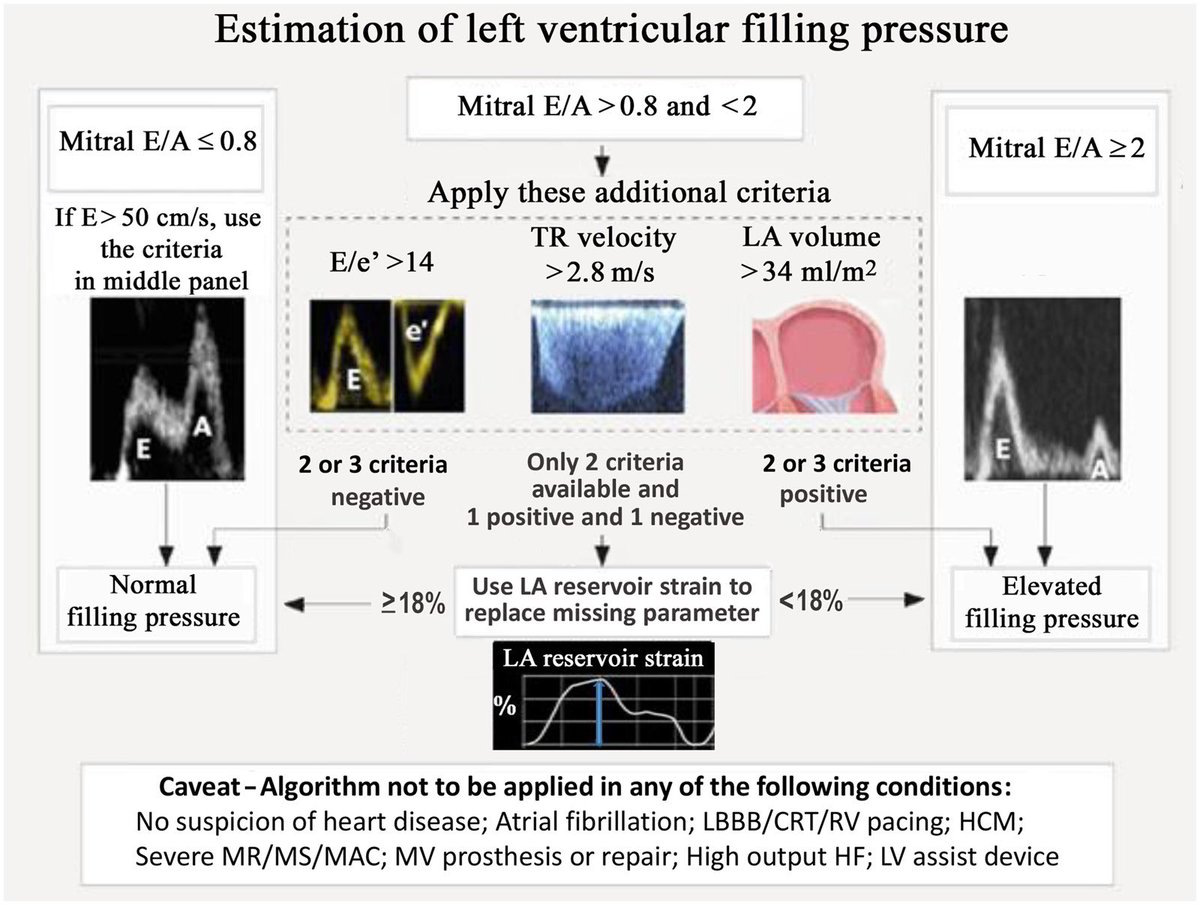
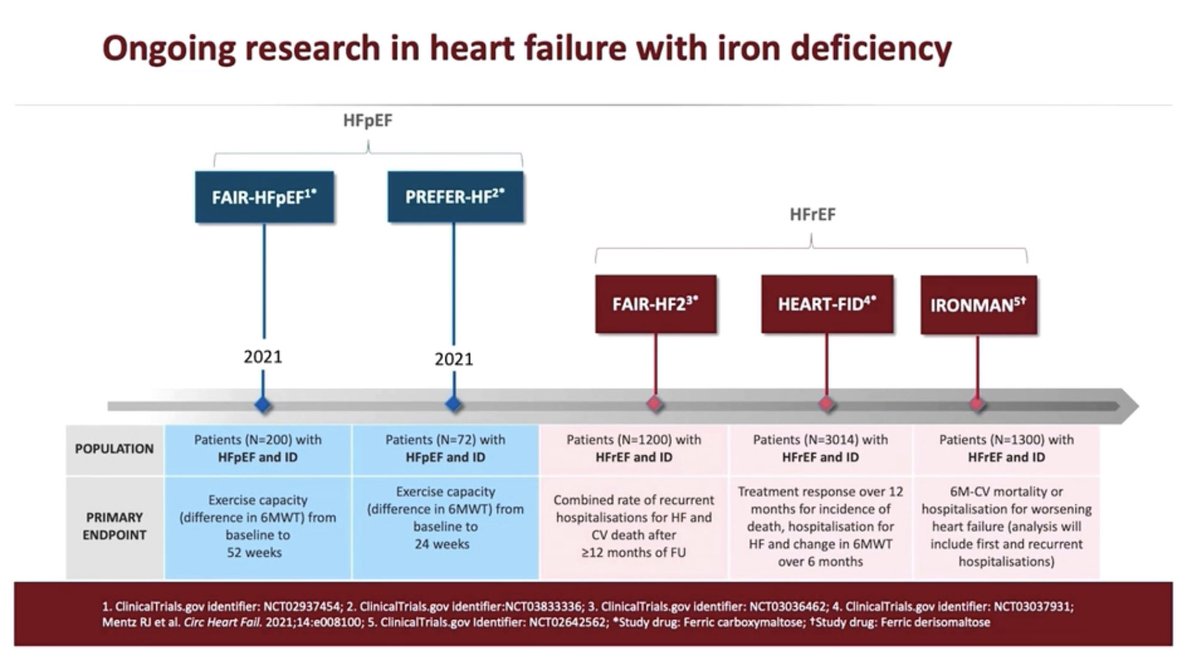
For patients with #HFpEF and either atrial or ventricular FMR, evidence for #GDMT ( ARNI/ARB + SGLT2i + MRA ) seems promising through their effect on LVRR
For patients with #HFpEF and either atrial or ventricular FMR, evidence for #GDMT ( ARNI/ARB + SGLT2i + MRA ) seems promising through their effect on LVRR
unroll @threadreaderapp
• • •
Missing some Tweet in this thread? You can try to
force a refresh