1/ What are 3 Qs you can ask yourself when looking at non-inferiority trials?
Q1) Was the trial planned i.e. pre-specified as comparing an intervention which is non-inferior to control?
WHY?
Bc changing the analysis *afterwards* introduces bias #StatswithCoreIM
Q1) Was the trial planned i.e. pre-specified as comparing an intervention which is non-inferior to control?
WHY?
Bc changing the analysis *afterwards* introduces bias #StatswithCoreIM

2/ Q2) was the control treatment administered to the full std of care?
The trial relies on strict adherence to full standard of care for the control arm, otherwise the whole confidence interval shifts with a relative⬆️in benefit of the intervention compared to control
The trial relies on strict adherence to full standard of care for the control arm, otherwise the whole confidence interval shifts with a relative⬆️in benefit of the intervention compared to control

3/ Q3) Did investigators perform both a per protocol and intention to treat analysis?
Per protocol:
Exaggerates group difference when intervention is inferior
Less likely to result in false positive
Intention to treat:
Makes groups prognostically 🟰
Benefit of randomization
Per protocol:
Exaggerates group difference when intervention is inferior
Less likely to result in false positive
Intention to treat:
Makes groups prognostically 🟰
Benefit of randomization

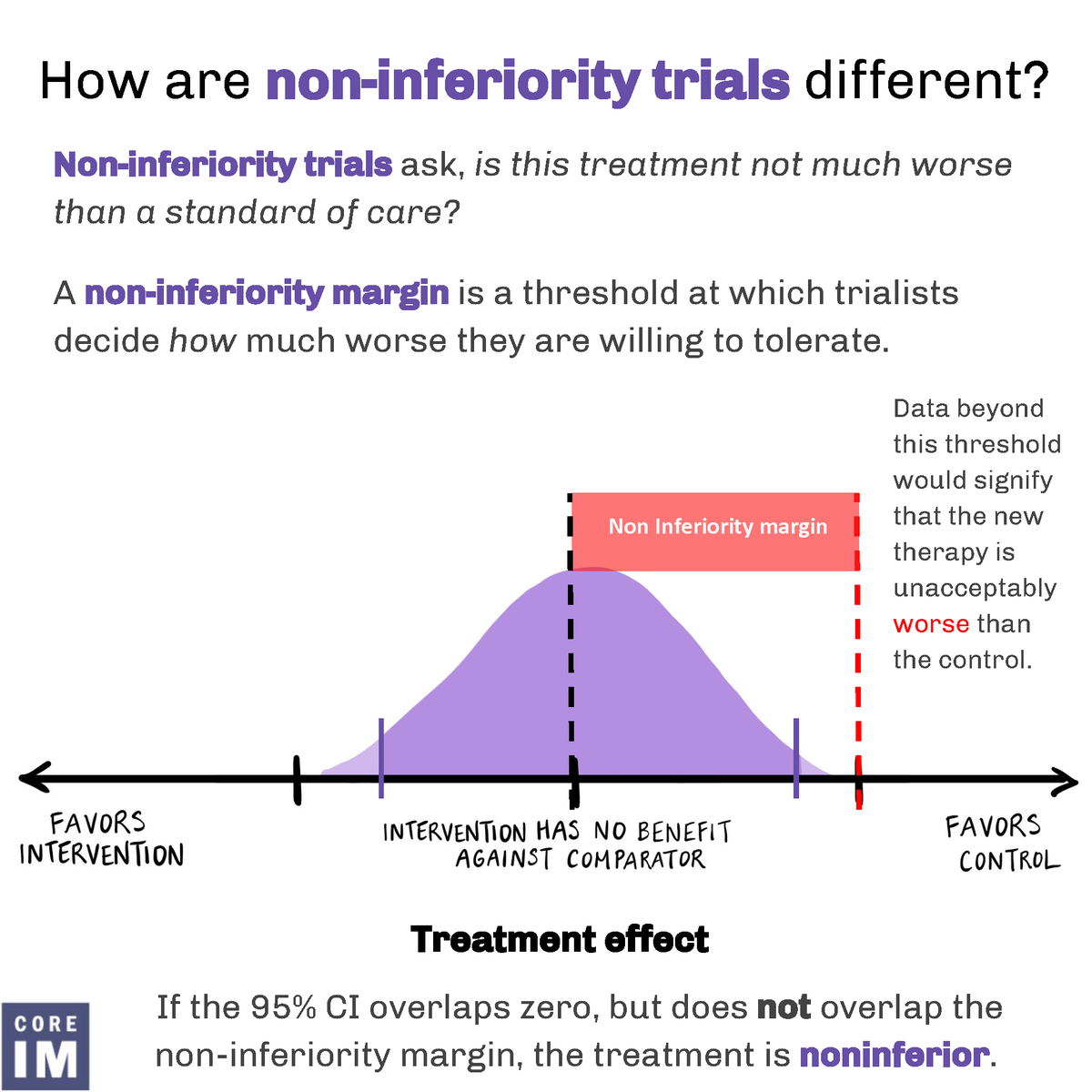
5/ What are the implications of the non-inferiority margin?
Let’s use an example!
The EXCEL trial asked if PCI is non-inferior to CABG in the treatment of left main disease for primary endpoint of death, stroke, or MI
The non-inferiority margin was determined to be 4.2%.
Let’s use an example!
The EXCEL trial asked if PCI is non-inferior to CABG in the treatment of left main disease for primary endpoint of death, stroke, or MI
The non-inferiority margin was determined to be 4.2%.

6/ At 3 years of follow-up, 15.4% of PCI patients vs. 14.7% of CABG patients experienced a primary end-point event (death, stroke, MI).
The between-group difference was 0.7%
The between-group difference was 0.7%

7/ Non-inferiority margin of 4.2% meant that non-inferiority was demonstrated (p=0.02) BUT
- Worse case 4.2% more pts with PCI may suffer an adverse event compared to CABG
- On average 0.7% more pts have an event with PCI
So, reasonable to choose CABG over PCI in low risk pts
- Worse case 4.2% more pts with PCI may suffer an adverse event compared to CABG
- On average 0.7% more pts have an event with PCI
So, reasonable to choose CABG over PCI in low risk pts

8/ Finally, take home points:
Sources of biases:
✔️Retroactive or re-analysis of superiority trial as non-inferiority
✔️Substandard care in control group
✔️Failure to perform both per protocol & intention to treat
Think critically about the non-inferiority margin!
Sources of biases:
✔️Retroactive or re-analysis of superiority trial as non-inferiority
✔️Substandard care in control group
✔️Failure to perform both per protocol & intention to treat
Think critically about the non-inferiority margin!

9/ That’s all for #StatswithCoreIM. Thanks for learning some #biostatistics with us this Wednesday and big shout-out to the author with this byte Dr. Robert Wharton and graphics by @ivannatang
For more #noninferiority trials byte:
For more #noninferiority trials byte:
https://twitter.com/COREIMpodcast/status/1539316668781961216
• • •
Missing some Tweet in this thread? You can try to
force a refresh