For those who can't get enough from #ADVOR, below the promised Tweetorial!
Acetazolamide in acute #HeartFailure w volume overload on background high-dose loop diuretics:
👍Increases diuresis & natriuresis
👍More euvolemia after 3 days & discharge
👍⬇️LOS
#ESCCongress #Cardiology
Acetazolamide in acute #HeartFailure w volume overload on background high-dose loop diuretics:
👍Increases diuresis & natriuresis
👍More euvolemia after 3 days & discharge
👍⬇️LOS
#ESCCongress #Cardiology
First, the unsung hero's of this trial, done with a little bit over 2 million €, bargain for largest diuretic #RCT ever!
@KatrienTartagl2 & her team, with only 3FTE, they ran the most successful trial in #AHF
@PieterMartensMD & @JeroenDauw who did most fieldwork
👏
@KatrienTartagl2 & her team, with only 3FTE, they ran the most successful trial in #AHF
@PieterMartensMD & @JeroenDauw who did most fieldwork
👏
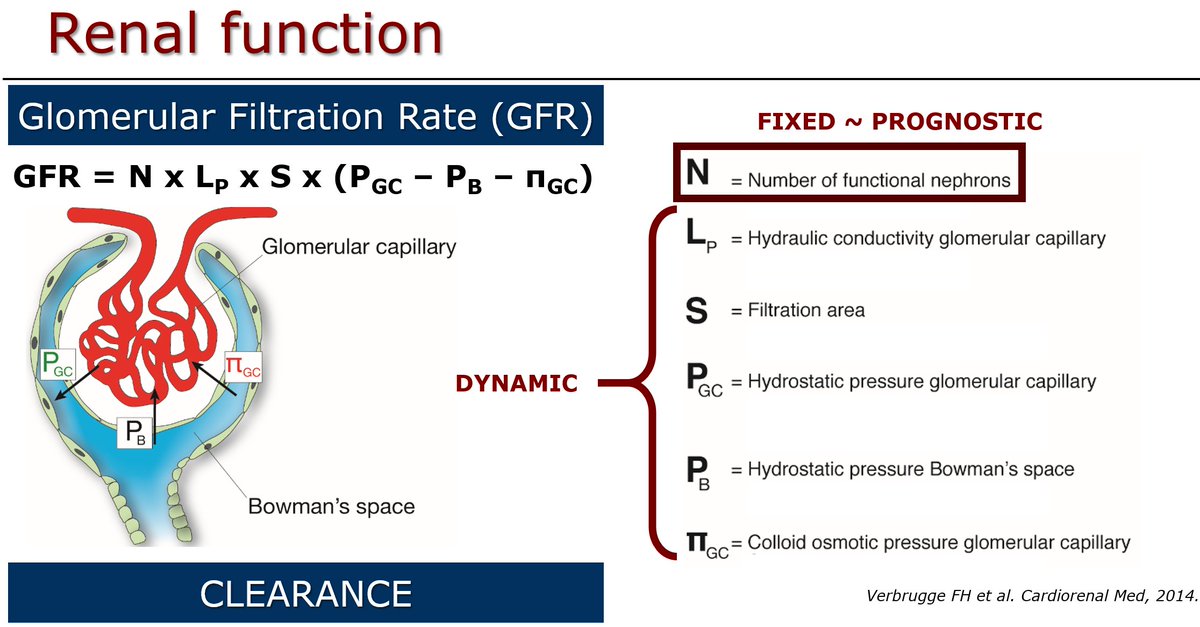
How did we come up with the idea? Actually, cause we all love #physiology. Credits go to Prof. Em. Paul Steels who teached us all how kidneys work.
@GLW_UHasselt
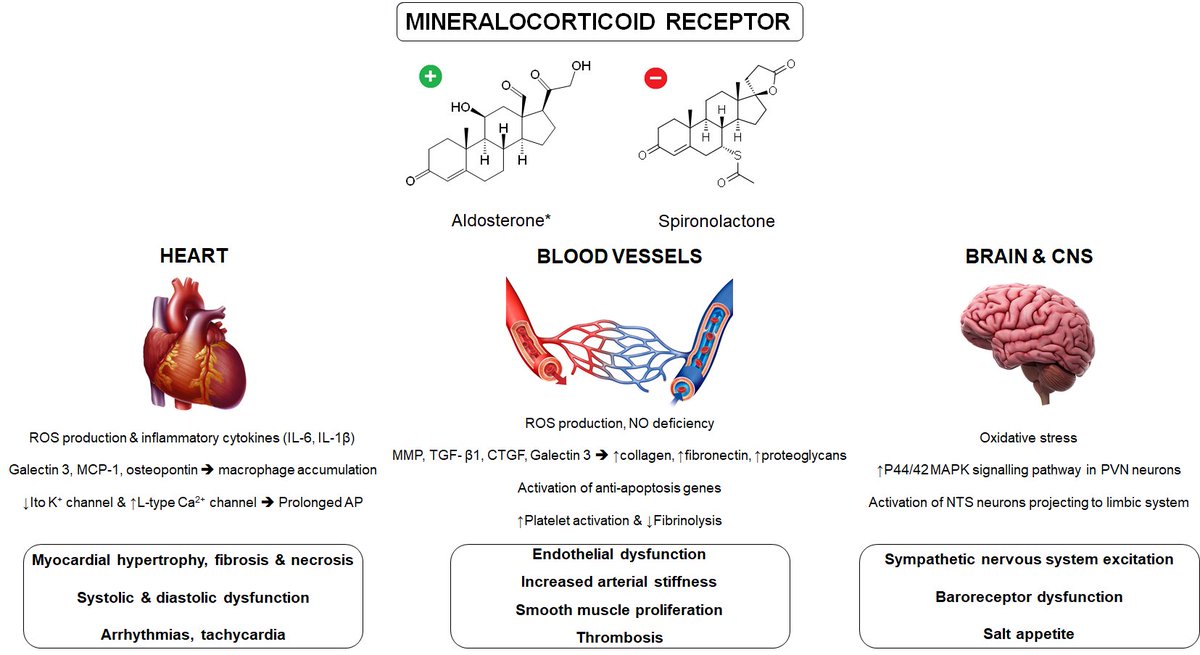
65% of sodium is reabsorbed in the proximal tubules, can be up to 85% in #HeartFailure
@GLW_UHasselt
65% of sodium is reabsorbed in the proximal tubules, can be up to 85% in #HeartFailure

Moreover, kidneys are smart organs:
Proximal = leaky➡️keeps distal nephron flow 🟰
Distal = waterproof ➡️homeostasis
Proximal diuretics ➡️more distal flow➡️give kidneys back control on homeostasis (they are far better than cardiologists)
Proximal = leaky➡️keeps distal nephron flow 🟰
Distal = waterproof ➡️homeostasis
Proximal diuretics ➡️more distal flow➡️give kidneys back control on homeostasis (they are far better than cardiologists)

Also, more chloride from proximal to the macula densa sensor acts like a break on the neurohumoral system.
Read everything about it in our review @ESC_Journals @JACCJournals:
onlinelibrary.wiley.com/doi/10.1002/ej…
sciencedirect.com/science/articl…
Read everything about it in our review @ESC_Journals @JACCJournals:
onlinelibrary.wiley.com/doi/10.1002/ej…
sciencedirect.com/science/articl…

Challenge in #ADVOR: which endpoint in acute #HeartFailure trial?
- Impossible to power for mortality/heart failure readmissions (probably influenced a lot more by chronic treatment & disease severity)
- First idea was natriuresis with secondary endpoint of clinical decongestion
- Impossible to power for mortality/heart failure readmissions (probably influenced a lot more by chronic treatment & disease severity)
- First idea was natriuresis with secondary endpoint of clinical decongestion
Funder @KCEfgov made us promote the secondary endpoint to the primary and gave us the leverage to include more patients.
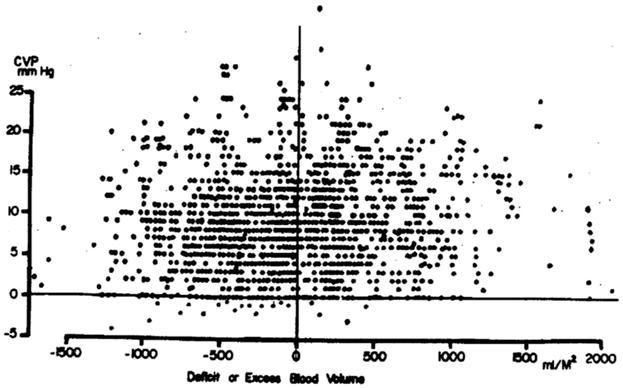
Diuretics treat volume overload🚫pressure, that's why we ended up with these 3 pivotal signs (flash lung edema occur even with normal volume)
Diuretics treat volume overload🚫pressure, that's why we ended up with these 3 pivotal signs (flash lung edema occur even with normal volume)

Pay attention on background infusion of 500 mL Dextrose 5% with 3 g MgSO4, You will lose more magnesium (and potassium) with acetazolamide. Because it increases free water excretion, the dextrose is not a problem. It's the salt You are after!
Importantly, can't make up for a missed opportunity! AFTER randomised treatment period, decongestion curves keep separating. Remember that #acetazolamide is a break on the neurohumoral system. You don't break when Your already over the cliff! 

We could decrease length of stay with 1 day, imagine the impact if this strategy would be employed on a more systematic base worldwide?
My only concern: very cheap drug produced by one generic company, please don't let this become an expensive medicine
#acetazolamideforall
My only concern: very cheap drug produced by one generic company, please don't let this become an expensive medicine
#acetazolamideforall
• • •
Missing some Tweet in this thread? You can try to
force a refresh