
#ESCCongress
Let's get straight to the point about #INVICTUS
The only people not surprised by the results are imagers that do TOEs (TEEs) on these patients! No way VKA was going to lose to NOACs here!😂
A 🧵...
#medtwitter #cardiotwitter #echofirst #epeeps
Let's get straight to the point about #INVICTUS
The only people not surprised by the results are imagers that do TOEs (TEEs) on these patients! No way VKA was going to lose to NOACs here!😂
A 🧵...
#medtwitter #cardiotwitter #echofirst #epeeps
#ESCCongress
Patients with rheumatic MV disease typically have very different atrial appearances on TOE. No matter how well anticoagulated, there is very often spontaneous echo contrast in the LA
These atria are just different...why?
Who is this?
Patients with rheumatic MV disease typically have very different atrial appearances on TOE. No matter how well anticoagulated, there is very often spontaneous echo contrast in the LA
These atria are just different...why?
Who is this?

The answer is Ludwig Aschoff (1866 - 1942), German physician & pathologist
He described what are now known as Aschoff bodies - inflammatory infiltrates in the atrial walls that eventually turn to fibrotic tissue, which contributes to the atrial myopathy we see in these patients
He described what are now known as Aschoff bodies - inflammatory infiltrates in the atrial walls that eventually turn to fibrotic tissue, which contributes to the atrial myopathy we see in these patients
#ESCCongress
Anyway, back to the trial!
Now, we know NOACs have completely changed the way non-valvular AF is treated in many countries. VKAs rarely given now in UK for newly diagnosed AF, most get a NOAC
But 'valvular AF' omitted from landmark RCTs
Anyway, back to the trial!
Now, we know NOACs have completely changed the way non-valvular AF is treated in many countries. VKAs rarely given now in UK for newly diagnosed AF, most get a NOAC
But 'valvular AF' omitted from landmark RCTs
#ESCCongress
Now, back in 2019, @ToddNeale reported on behalf of @TCTMD that a retrospective observational S Korean study suggested a benefit for NOACs in mitral stenosis patients
However, discussants wisely suggested this needed to be tested in a RCT
tctmd.com/news/doacs-pat…
Now, back in 2019, @ToddNeale reported on behalf of @TCTMD that a retrospective observational S Korean study suggested a benefit for NOACs in mitral stenosis patients
However, discussants wisely suggested this needed to be tested in a RCT
tctmd.com/news/doacs-pat…
#ESCCongress
So, here comes the INVICTUS trial
Investigation of Rheumatic AF Treatment Using Vitamin K Antagonists, Rivaroxaban or Aspirin Studies
Question - is it safe to give patients with rheumatic MV disease & a history of AF a NOAC instead of a VKA?
Non-inferiority trial
So, here comes the INVICTUS trial
Investigation of Rheumatic AF Treatment Using Vitamin K Antagonists, Rivaroxaban or Aspirin Studies
Question - is it safe to give patients with rheumatic MV disease & a history of AF a NOAC instead of a VKA?
Non-inferiority trial
#ESCCongress
INCL criteria:
Age >18
Echo evidence of RHD
AF/flutter at any time in the past
PLUS ONE OF THE FOLLOWING:
CHADS-VASc score 2 or more
MV area <2.0cm2 on echo
LA spontaneous echo contrast / thrombus on echocardiography
85% had mod-severe MS. ~1/4 had MVA <1.0cm2
INCL criteria:
Age >18
Echo evidence of RHD
AF/flutter at any time in the past
PLUS ONE OF THE FOLLOWING:
CHADS-VASc score 2 or more
MV area <2.0cm2 on echo
LA spontaneous echo contrast / thrombus on echocardiography
85% had mod-severe MS. ~1/4 had MVA <1.0cm2
#ESCCongress
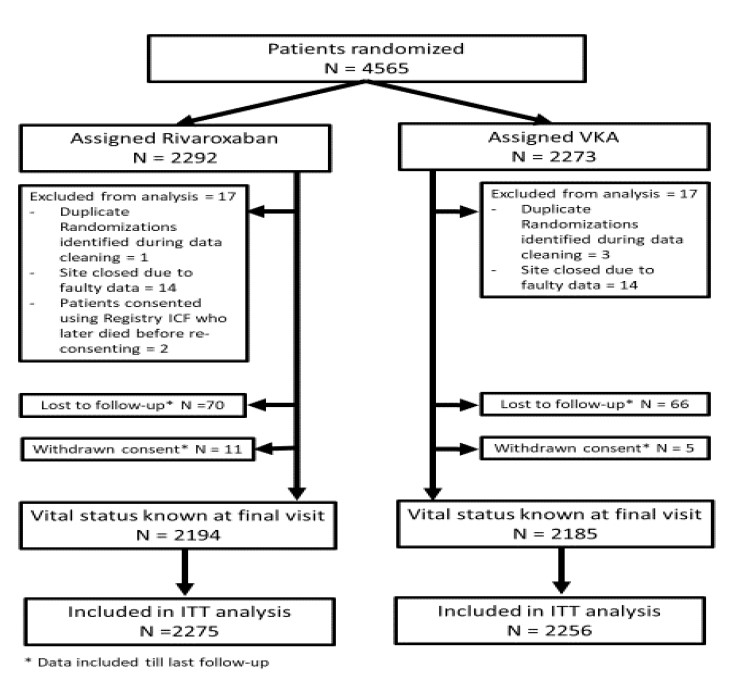
138 recruiting sites across 24 countries
43% Africa, 40% Asia, 8% Latin America, 9% others
4565 patients recruited
Mean age 50
72% female
138 recruiting sites across 24 countries
43% Africa, 40% Asia, 8% Latin America, 9% others
4565 patients recruited
Mean age 50
72% female
#ESCCongress
Trial recruited from Aug 2016 - Sept 2019
Original primary EP had to be changed during the trial due to fewer than expected strokes but more than expected deaths
Primary EP - composite of stroke/systemic embolism/MI/death
Details are here...
Trial recruited from Aug 2016 - Sept 2019
Original primary EP had to be changed during the trial due to fewer than expected strokes but more than expected deaths
Primary EP - composite of stroke/systemic embolism/MI/death
Details are here...

Patients randomised to rivaroxaban got 20mg or 15mg OD based on renal function
Patients randomised to VKA got warfarin (~80%) or acenocoumarol (~20%): target INR range 2.0-3.0
INR control got a lot BETTER for those that had been on warfarin prior to the trial that stayed on it
Patients randomised to VKA got warfarin (~80%) or acenocoumarol (~20%): target INR range 2.0-3.0
INR control got a lot BETTER for those that had been on warfarin prior to the trial that stayed on it

#ESCCongress
What did they find? That patients on rivaroxaban did WORSE:
More death!
More ischaemic strokes!
No diff in major bleeding!
What did they find? That patients on rivaroxaban did WORSE:
More death!
More ischaemic strokes!
No diff in major bleeding!

#ESCCongress
You can read an excellent full write-up about the trial by @michaelTCTMD for @TCTMD here:
tctmd.com/news/invictus-…
@mmamas1973 @ShelleyWood2
You can read an excellent full write-up about the trial by @michaelTCTMD for @TCTMD here:
tctmd.com/news/invictus-…
@mmamas1973 @ShelleyWood2
#ESCCongress
The discussion focuses on how surprised everyone was and what could explain the reason for this unexpected result
Editorial also explores similar issues
But, once again, these results don't surpise me.
Not due to past NOAC data, but due to the RHD hearts...
The discussion focuses on how surprised everyone was and what could explain the reason for this unexpected result
Editorial also explores similar issues
But, once again, these results don't surpise me.
Not due to past NOAC data, but due to the RHD hearts...
#ESCCongress
I do a lot of pre-AF ablation TOE to check the LA appendage. What do we do if find thrombus, even in someone on a NOAC?
Often we switch to VKA with a higher target INR than usual (e.g. 2.5-3.0 or 2.5-3.5) and re-TOE in 3 months. LAA almost always looks better
I do a lot of pre-AF ablation TOE to check the LA appendage. What do we do if find thrombus, even in someone on a NOAC?
Often we switch to VKA with a higher target INR than usual (e.g. 2.5-3.0 or 2.5-3.5) and re-TOE in 3 months. LAA almost always looks better
Purely from my TOE experience, I would never have imagined a NOAC could suffice for rheumatic MS. I know it seemed sufficient in the RIVER trial with bioprosthetic MVR, but this is different, I think
#ESCCongress
Bottom line - for rheumatic MS, keep using VKA and not NOAC
Advantage - VKA is cheap. NOAC is expensive
Disadvantage - hassle of regular INR monitoring, logistics of this in LMICs & challenge of a maintaining decent time in therapeutic range (TTR)
Bottom line - for rheumatic MS, keep using VKA and not NOAC
Advantage - VKA is cheap. NOAC is expensive
Disadvantage - hassle of regular INR monitoring, logistics of this in LMICs & challenge of a maintaining decent time in therapeutic range (TTR)
Final point
A superb reminder of the importance of following through the evidence chain
The retrospective, observational outcome study *suggested* an association between NOACs and better outcomes
But the subsequent RCT actually showed the complete opposite!
@drjohnm
A superb reminder of the importance of following through the evidence chain
The retrospective, observational outcome study *suggested* an association between NOACs and better outcomes
But the subsequent RCT actually showed the complete opposite!
@drjohnm
Observational studies are called that for a reason - one can make *observations*! You can suggest an association but cannot prove causation
Despite PSM in the 2019 study, there must have been residual confounding
So, do the RCT when you can...
Congrats to study authors!
Despite PSM in the 2019 study, there must have been residual confounding
So, do the RCT when you can...
Congrats to study authors!
• • •
Missing some Tweet in this thread? You can try to
force a refresh












