Our dream comes true: the #WATERFALLtrial has been published in @NEJM Aggressive fluid resuscitation in acute pancreatitis is not safe & does not improve outcomes #GItwitter #SomosAEG @aegastro
What's behind this publication?
It all started 21 years ago
nejm.org/doi/full/10.10…
What's behind this publication?
It all started 21 years ago
nejm.org/doi/full/10.10…
2001, I started to attend patients with acute pancreatitis as a GI resident in @GVAsalualicante. Books and papers recommended aggressive fluid resuscitation. It was believed that many fluids increased pancreatic blood flow preventing pancreatic necrosis
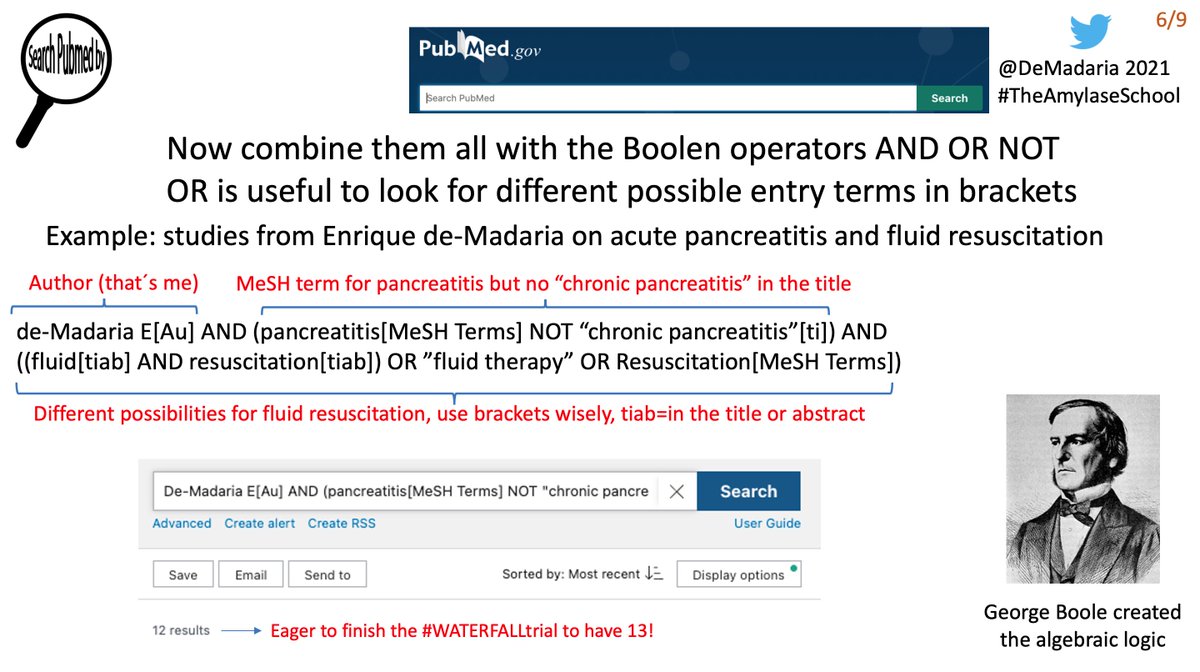
But I asked to myself, what is aggressive fluid resuscitation, how much fluids, and which type of fluids? I looked for specific data, but all was vague. I asked in GI meetings, and the answers of experts were vague, no specific fluid rate, just generalities
In 2005 I started being in charge of @GVAsalualicante pancreatic unit thanks to my boss Miguel Pérez-Mateo, my mentor. The question remained unanswered (and I was obsessed). 2 years later we started a prospective study on the effect of fluid volume on acute pancreatitis outcomes
This observational study showed that patients receiving the highest quartile of fluid volume had WORSE outcomes! It was published on @AmJGastro
journals.lww.com/ajg/Abstract/2…
journals.lww.com/ajg/Abstract/2…
An editorial by Bechien Wu, “fluid resuscitation in acute pancreatitis: striking the right balance” remarked that the study challenged several of our long-held beliefs regarding the benefits of vigorous fluid resuscitation in acute pancreatitis
journals.lww.com/ajg/Abstract/2…
journals.lww.com/ajg/Abstract/2…
Then we became interested in fluid sequestration as an important factor in fluid resuscitation, and a source of bias. In a collaborative study with my friend Vikesh Singh we described the determinants of fluid sequestration @AGA_CGH cghjournal.org/article/S1542-…
For me, this paper was my first collaborative study, my first international study, and an incredible experience, That year I had my first talk outside Spain in the @HopkinsGIHep GI course. This collaboration brought me that awesome experiences, thanks Vik, my friend
With all this experience we hypothesized a new model to understand fluid resuscitation in acute pancreatitis: the dynamic model published in @AGA_CGH cghjournal.org/article/S1542-… 

Then we looked at fluid resuscitation at the very initial phase of acute pancreatitis: fluid boluses administered in the emergency room, we published this observational study on @UEGJournal Patients receiving more fluids did not have better outcomes onlinelibrary.wiley.com/doi/10.1177/20…
We focused then on the type of fluid resuscitation; in our first RCT we compared lactated Ringer solution vs normal saline, we described that Ringer was associated with an anti-inflammatory effect, as suggested by a previous RCT by B Wu in 2011 @UEGJournal journals.sagepub.com/doi/10.1177/20…
In that paper my friend @nielo40 did some basic stuff to complement our single-center RCT on patients, and demonstrated that lactate from Ringer Lactate was the anti-inflammatory molecule, thanks Mestre!
journals.sagepub.com/doi/10.1177/20…
journals.sagepub.com/doi/10.1177/20…
But the old question remained unanswered,
How
much
fluids
should
we
administer
to
patients
with
acute
pancreatitis
?
How
much
fluids
should
we
administer
to
patients
with
acute
pancreatitis
?
In January 2019 I asked Federico Bolado from Pamplona, Spain and James Buxbaum from Los Angeles, USA to develop the #WATERFALLtrial as an international multicenter study to answer the critical question: does aggressive fluid resuscitation improve outcomes in acute pancreatitis
Designing the study was a nightmare, we had to develop definitions of fluid overload, hypovolemia, to develop a very complex electronic case report… a real challenge
Thanks James and Federico! hundreds of emails...
Thanks James and Federico! hundreds of emails...
My friends Pedro Zapater and Patrick Maissoneuve were in charge of statistics, they did a hard job! @Lguilabert1 was in charge of @GVAsalualicante patients and Alicia Vaillo coordinated the whole study, THANKS
We applied and received funding from @SaludISCIII (FIS national grant) @aegastro (Gonzalo Miño Grant) and @isabial_iis, without them #WATERFALLtrial would be only a dream, thanks!!!
18 centers from Spain Mexico Italy and India joined the #WATERFALLtrial Thanks! 

@Lguilabert1 @RodriguezGandia @EdgardLozada @cvsanchezmarin @DiegoCasas8 @EvitaMM81 @DrCasals @Veronica_Ubieto @jedor14 @cobrercaz @GuillermoGR87 @DigestivoHRyC
The funny thing is that I received the final acceptance of WATERFALL while I was writing a Twitter thread about @HarvardMINT2022 @CharuParanjape @krishnanendo , look 👇
https://twitter.com/DeMadaria/status/1542539716947578883?s=20&t=VSLJxVO8Jhna6YA4N-4b3g
So, 21 years after a practical question, a step-by-step learning process, inspired by my mentors and clearly by the @pancreatitis_nl group @MarcBesselink, guys you are the soul of clinical research
Finally, we are particularly proud that we could do this @NEJM study from a 300,000 inhabitants city on the coast of Spain, in a Spanish public hospital, with public funds @SaludISCIII @isabial_iis @GVAsalualicante @aegastro
So,
you can also do it! Just choose the right question, and start to walk, step by step, no rush
Good night
you can also do it! Just choose the right question, and start to walk, step by step, no rush
Good night
Finally!! Thanks to Tim Gardner for his @NEJM editorial on the #WATERFALLtrial! nejm.org/doi/full/10.10…
@EurPancClub @YouppiePancreas @maloehr1 @my_ueg @AmerGastroAssn @aecirujanos @Sociedad_SEMI @semfyc @CirugiaQST @SEMERGENap @LlorensPere @SEMES_
• • •
Missing some Tweet in this thread? You can try to
force a refresh