@Ropivacaine introduces @KalagaraHari for @DalAnesthesia grand rounds: Perioperative POCUS (P-POCUS) 





@KalagaraHari (@MayoClinic @MayoAnesthesia @ASRA_Society) promises a whistle stop tour of P-POCUS following an alphabetical approach (would make @rosie_hogg #oaa3dc2022 proud) during his @DalAnesthesia grand rounds 







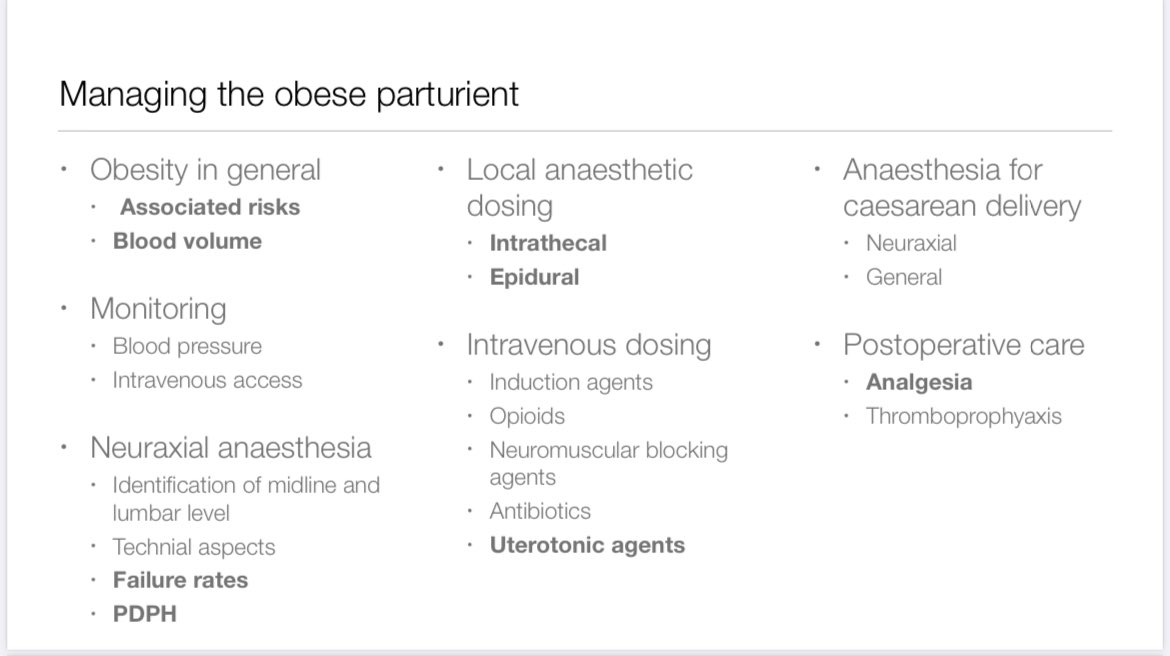
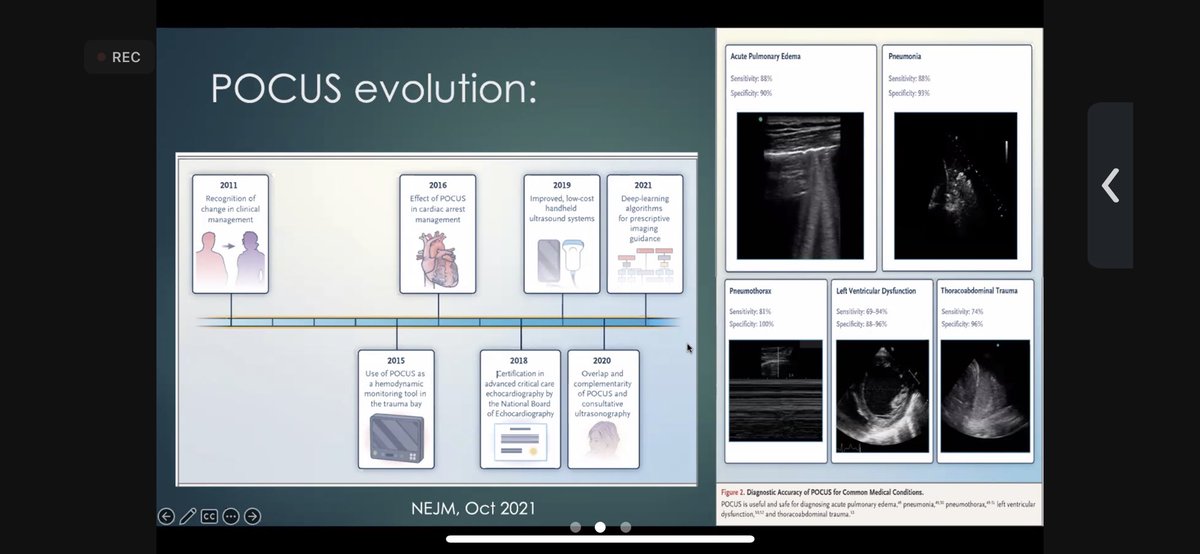
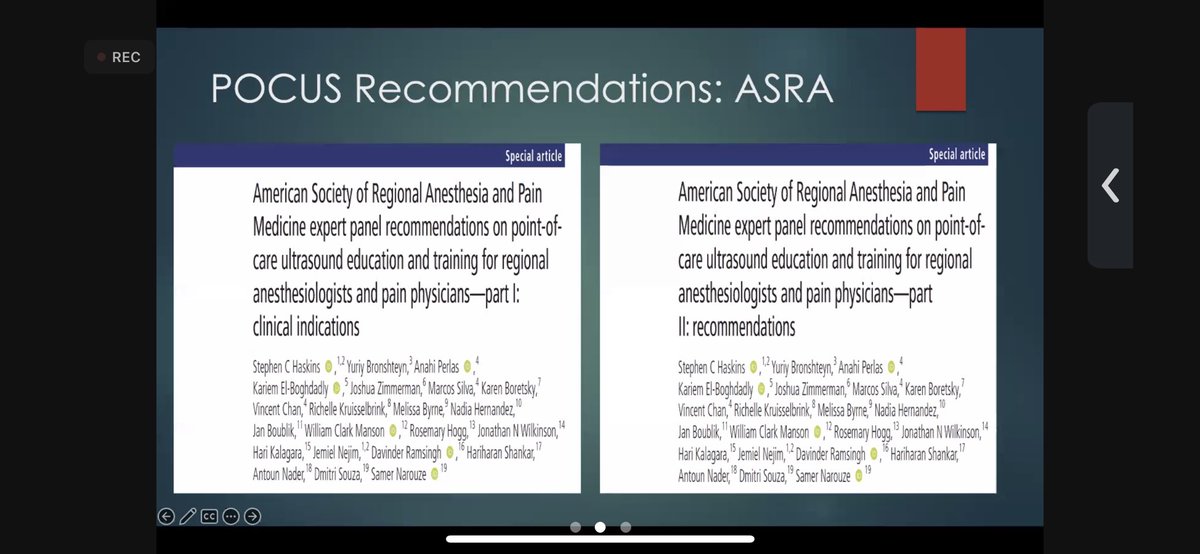
How does it help? Can use POCUS to evaluate almost anything, and perhaps soon everything, giving real time information and assistance with decision making. It has evolved over time, culminating in @ASRA_Society recommendations 



Starting at A - airway, a comfortable space for anesthesiologists. US has multiple uses. @doctimcook would be proud - finding the CTM was not well done. A midsagittal scan assists (altho probably not advisable in an emergency, it should probably be included in airway assessment) 







It’s usefulness extends beyond identification of CTM, also including confirmation of endotracheal intubation and detecting oesophageal intubation. 







P-POCUS offers an improvement over auscultation regards detecting bronchial intubation - even useful for DLT placement & assessment of isolation. PUMA (@UniversalAirway ) guidelines recognize P-POCUS as an alternative for assessment & prevention of oesophageal intubation 



Gastric US (skipping a few letters because it links to airway) - something anesthesia and grandma’s worry about. Aspiration is rare but deadly, even requiring ECMO. Mortality and morbidity from aspiration hasn’t improved over time - aspiration is never normal, always bad. 







Gastric US is a good, quick and easy technique to learn. Differentiating empty from fluid, from solid is key! Latter definitely indicates RSI. It is most useful when a patient is probably not NPO, the emergent case 







B - Lung ultrasound has multiple immediate clinical utilities (especially for regionalists doing brachial plexus blocks). Multiple pathologies can be identified/ suspected. Video works better, but the moving arrow shows lung sliding, associated with inflation. 







P-POCUS more sensitive than CXR, probably earlier detection for pneumothorax. Pleural effusions clear (learning what normal is helps) - significantly improved sensitivity &, because POC, clinical correlation is built in! Also assists in identifying interstitial dx & pulm oedema 







The BLUE protocol for lung P-POCUS allows a diagnostic algorithm. Good sensitivity and specificity in trained hands. LUS was of particular importance & clinical utility during #COVID19 detecting both progression and recovery. 





C - cardiac P-POCUS (always a crowd pleaser) - important to remember at outset, multiple perspectives/views essential for understanding. 5F’s of FoCUS - not cardiologists or echocardiographers (don’t need minutiae) gross information +/- enough. 5E’s of emergency echo (@AnaSjaus) 





I-AIM is key - basic views should be mastered, starting with perhaps the easiest pair: parasternal long axis (PLAX) and parastenal short axis (PSAX) - learn anatomy on normal hearts first, so can recognize when NOT normal 





Apical 4 chamber (A4C), a little trickier but lots to see. Subcostal 4 chamber, always useful to remember what is closest and identify anatomy from there? Assessing fluid responsiveness? Use subcostal window to look at IVC - full (right) versus collapsing (left) 







Regional wall motion assessment/ abnormalities - what coronary vessel involved? (@ASRA_Society POCUS spotlight by @DalAnesthesia’s own @AnaSjaus ) = great resource. International recommendations exist for TTE. 



P-POCUS has utility in evaluating chest pain, including LISA approach. ACLS recognizes utility of ultrasound in resuscitation - from ABC evaluation, to differentiation of subtypes of shock 







Multiple protocols exist - each with pro’s - and POCUS utility in diagnosis or stratification of the most common presenting complaint (dyspnoea) is probably beyond doubt 



And who sees a patient nowadays who hasn’t had a FAST scan? It allows for quick clinical decision making, bypassing potentially fatal delays seeking radiological confirmation/ diagnosis. 





Before the DVT becomes a PE (affecting images in B), P-POCUS can identify clot and even identify a loose threatening clot. 

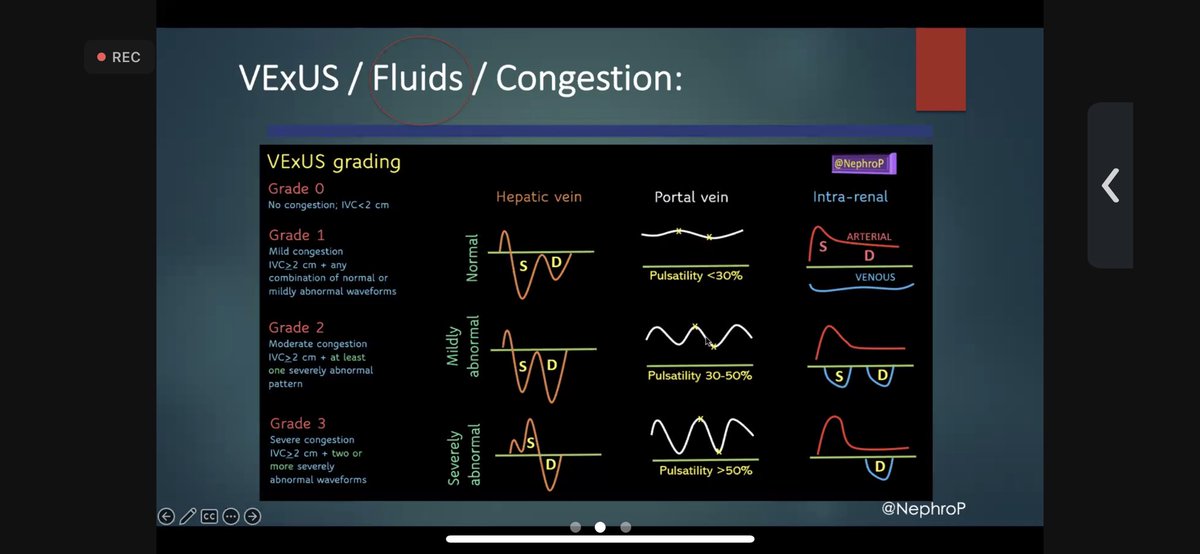
Fluids are drugs! Appropriate fluid management is essential and VExUS allows for grading and assessment of fluid status and congestion 




P-POCUS stewardship is important. Right indication, interpretation and integration is essential. @KalagaraHari’ key points (PRACTICE!), his references, and an invitation to attend POCUS workshops concludes a overwhelming tour of the top of iceberg of P-POCUS. 







Great discussion period - @AnaSjaus highlights the longitudinal POCUS training for staff at @DalAnesthesia. Orlando Hung admits to taking the plunge. @KalagaraHari recommends usabcd.org as a starting point for aspiring P-POCUS users. @Ropivacaine happy in conclusion 







• • •
Missing some Tweet in this thread? You can try to
force a refresh