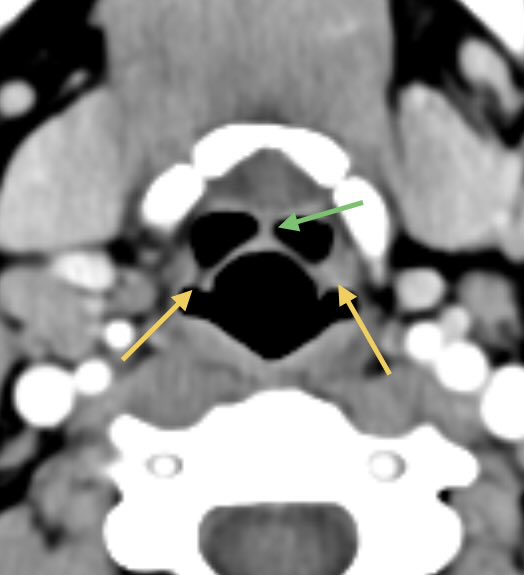
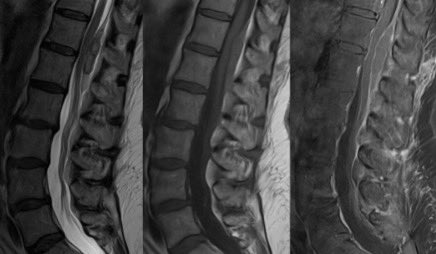
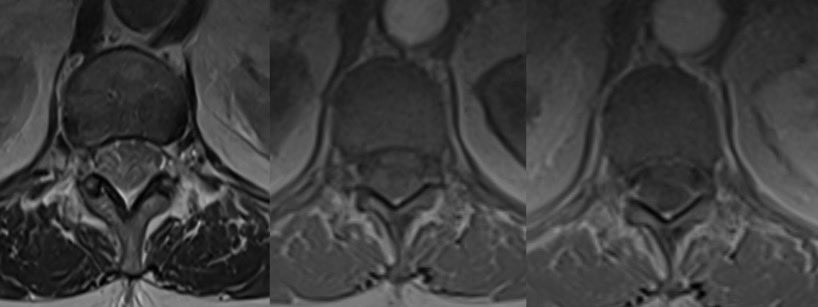
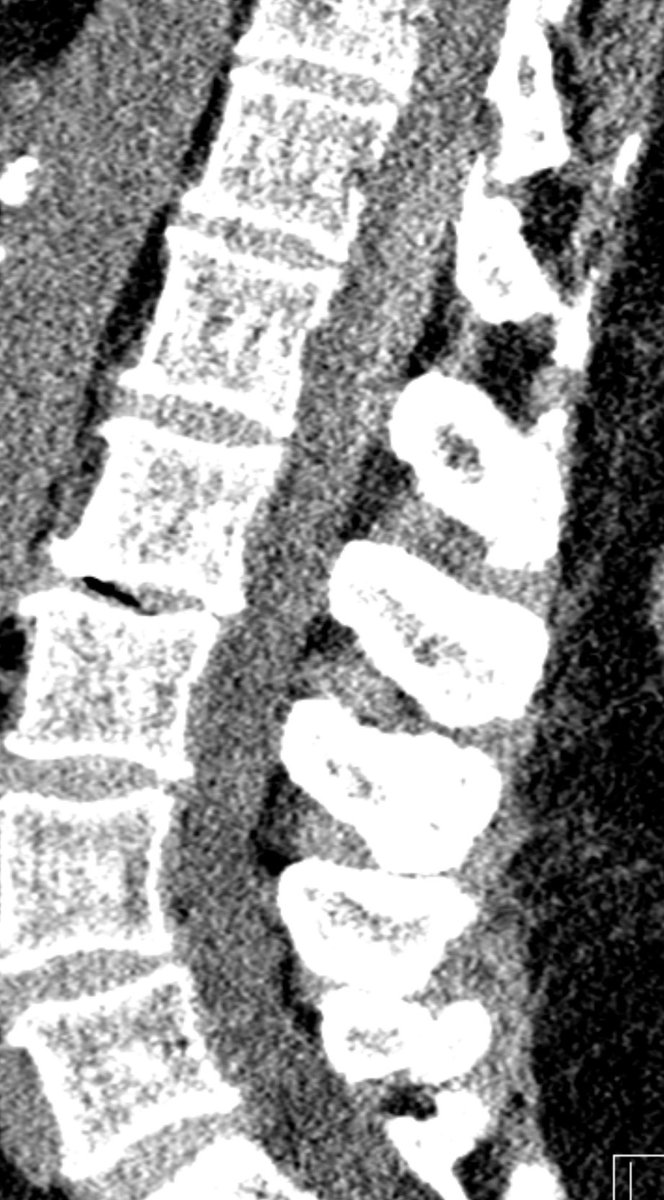
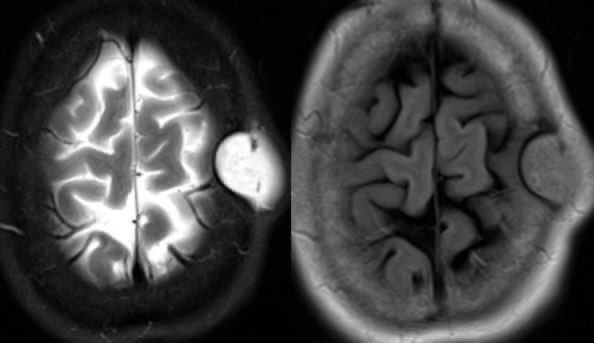
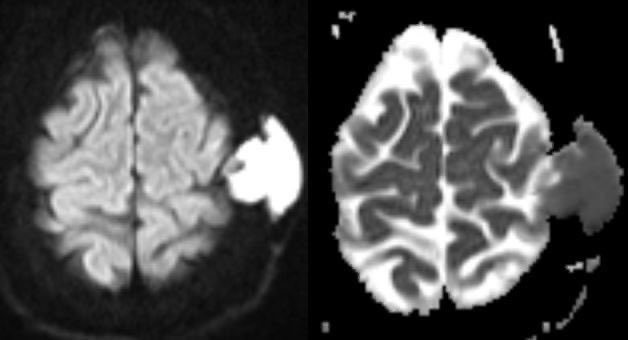
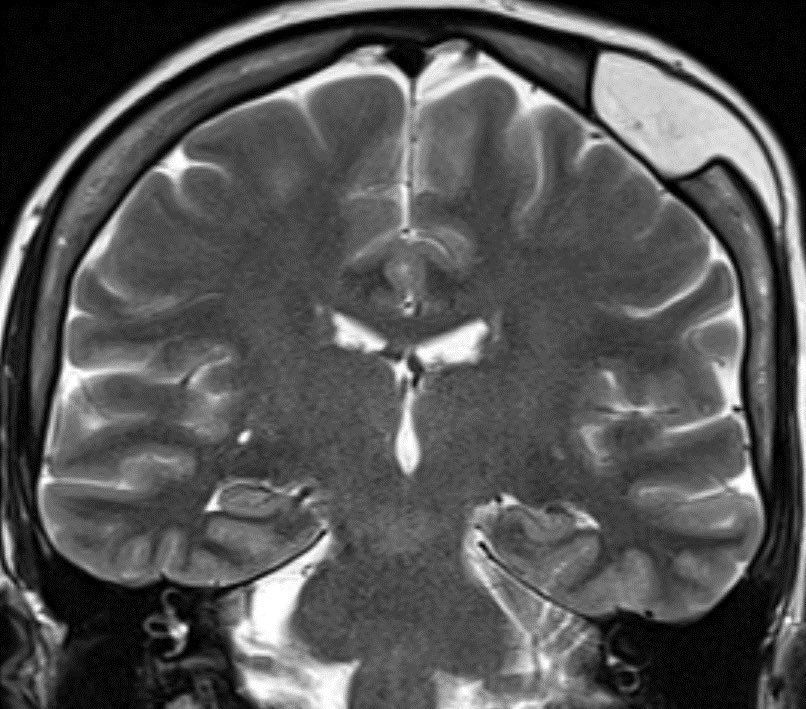
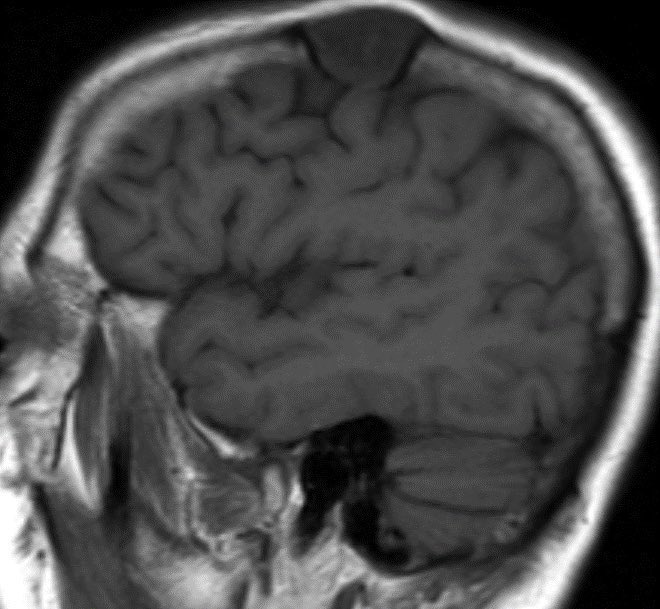
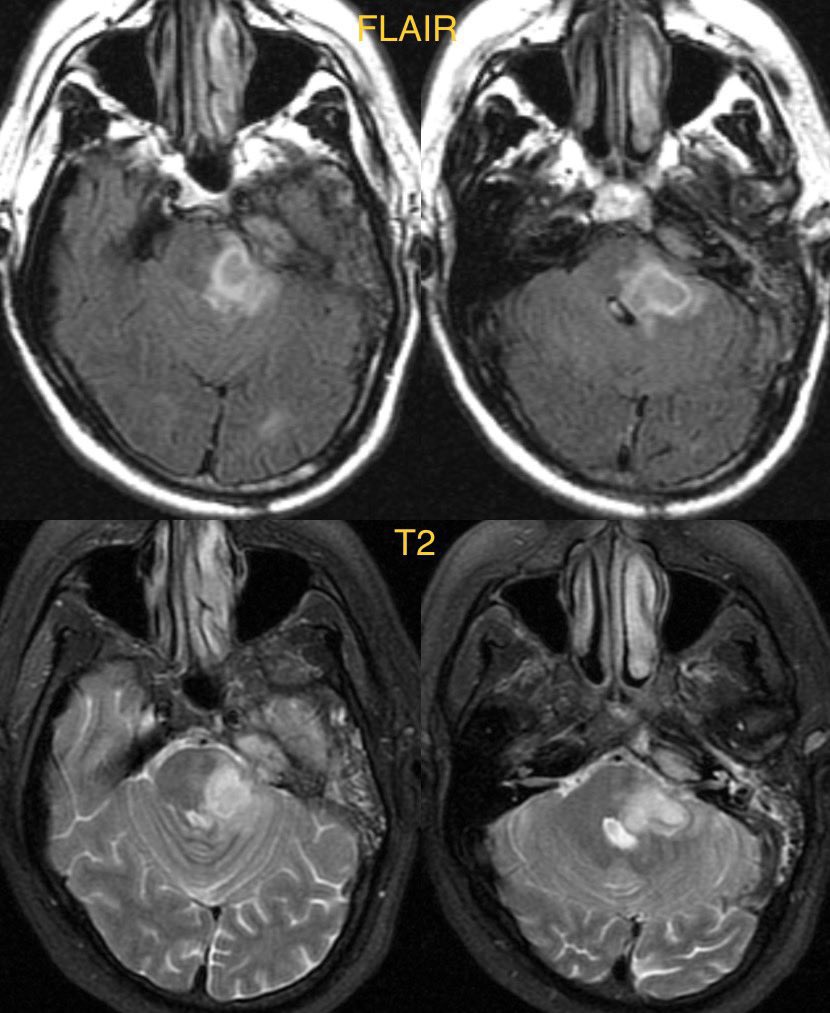
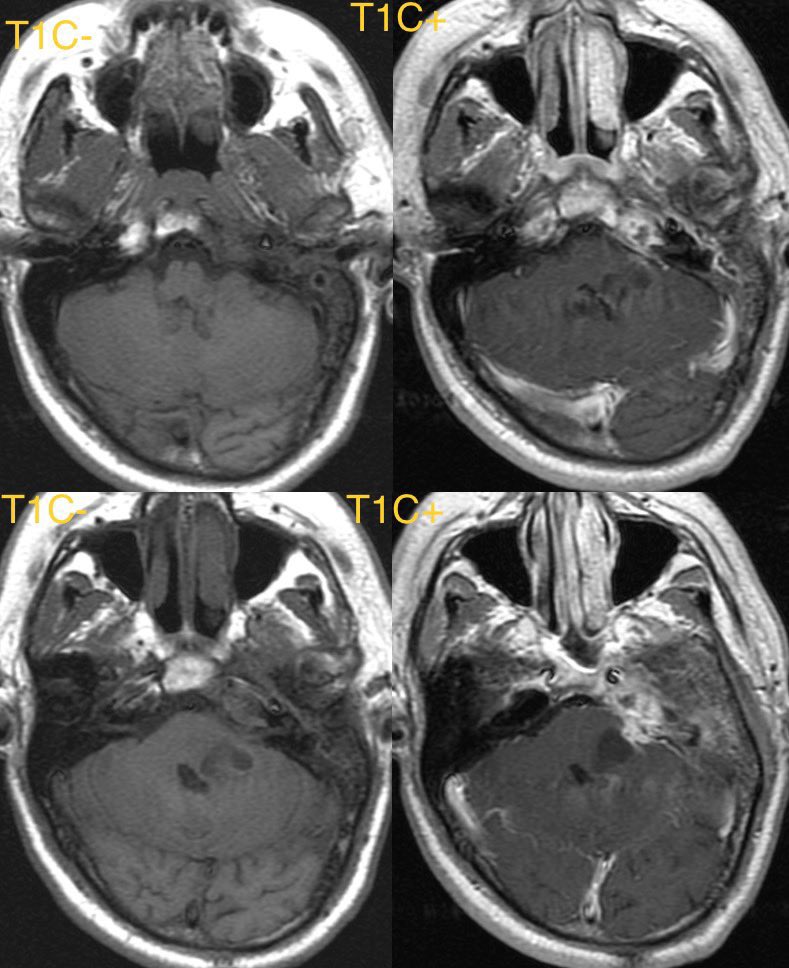
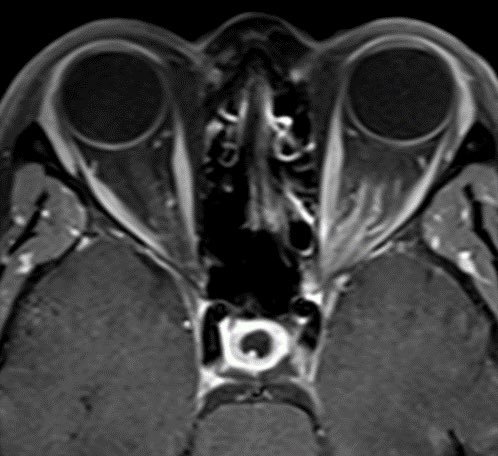
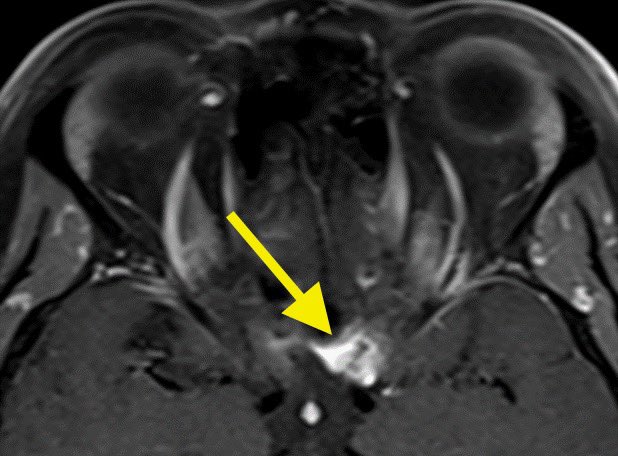
45F presents with painless progressive left eye vision loss. MR shows homogenous enhancement encasing the left optic nerve with an associated lesion at the entrance of the optic canal (yellow arrow)
#radres #futureradres #NeuroRad #MedTwitter @AlbanyMedRadRes


#radres #futureradres #NeuroRad #MedTwitter @AlbanyMedRadRes

Differential Diagnosis:
Optic Neuritis
Optic nerve sheath meningioma
Optic nerve glioma
Orbital sarcoidosis
Orbital lymphoma
Orbital pseudotumor
#Ophthalmology #radtwitter
Optic Neuritis
Optic nerve sheath meningioma
Optic nerve glioma
Orbital sarcoidosis
Orbital lymphoma
Orbital pseudotumor
#Ophthalmology #radtwitter
Diagnosis: Optic nerve sheath meningioma
Remember the optic nerve is an extension of the CNS and therefore, is surrounded by meninges and arachnoid cap cells from which meningiomas arise. Look for the “tram-track” sign of enhancement surrounding the optic nerve
#Ophthalmology
Remember the optic nerve is an extension of the CNS and therefore, is surrounded by meninges and arachnoid cap cells from which meningiomas arise. Look for the “tram-track” sign of enhancement surrounding the optic nerve
#Ophthalmology
Optic neuritis would be painFUL and display enhancement of the nerve itself and perineural fat
Optic nerve gliomas create enlargement of the nerve with variable enhancement typically in NF-1 patients
Other diagnoses are variable though typically present as intraorbital masses
Optic nerve gliomas create enlargement of the nerve with variable enhancement typically in NF-1 patients
Other diagnoses are variable though typically present as intraorbital masses
• • •
Missing some Tweet in this thread? You can try to
force a refresh