How to be an excellent clinical teacher in medicine. Tweetorial.
Just my thoughts during a 15 year career as a teacher, with some dabbling in #MedEd research.
Some GI themes but applicable to all I hope.
#GITwitter #MedTwitter
Just my thoughts during a 15 year career as a teacher, with some dabbling in #MedEd research.
Some GI themes but applicable to all I hope.
#GITwitter #MedTwitter
This is practical & based on lived experiences as a learner - training & as a lifelong learner; experiences as a teacher; feedback I've received & how I changed; some literature; & how I've tested some stuff experimentally mainly in #endoscopy
(caveat - not saying I'm excellent)
(caveat - not saying I'm excellent)

1. Safe learning environments
Man this is critical.
I'll use my consult rounds as an example. Everyone seated. I make sure schedule is cleared - nothing lingering. I don't lead - the senior-most house staff leads the rounds.
The environment should be fun and positive.
Man this is critical.
I'll use my consult rounds as an example. Everyone seated. I make sure schedule is cleared - nothing lingering. I don't lead - the senior-most house staff leads the rounds.
The environment should be fun and positive.
➡️No harsh words
➡️No making fun of anyone
➡️Questions will be asked and it's ok to not know the answers
➡️I admit when I don't know
➡️It's ok to use devices to look stuff up in rounds
➡️It's ok to question me
➡️+ feedback often with others
➡️- feedback small groups or in private
➡️No making fun of anyone
➡️Questions will be asked and it's ok to not know the answers
➡️I admit when I don't know
➡️It's ok to use devices to look stuff up in rounds
➡️It's ok to question me
➡️+ feedback often with others
➡️- feedback small groups or in private
And respect for others who are not the same as you.
It's ok to screw up. And you shouldn't be crucified for it.
It's also why I like #simulation so much - it's easy to make the environment super safe.
Safe learning environments are foremost in #MedEd IMO.
It's ok to screw up. And you shouldn't be crucified for it.
It's also why I like #simulation so much - it's easy to make the environment super safe.
Safe learning environments are foremost in #MedEd IMO.
2. Challenge learners appropriately
There is this education theory I love called #challengepointheory - learning is optimized when the difficulty of a task is matched in a sort of Goldilocks zone.
Too easy - they know it, not much gain
Too hard - then can't even tackle it
There is this education theory I love called #challengepointheory - learning is optimized when the difficulty of a task is matched in a sort of Goldilocks zone.
Too easy - they know it, not much gain
Too hard - then can't even tackle it

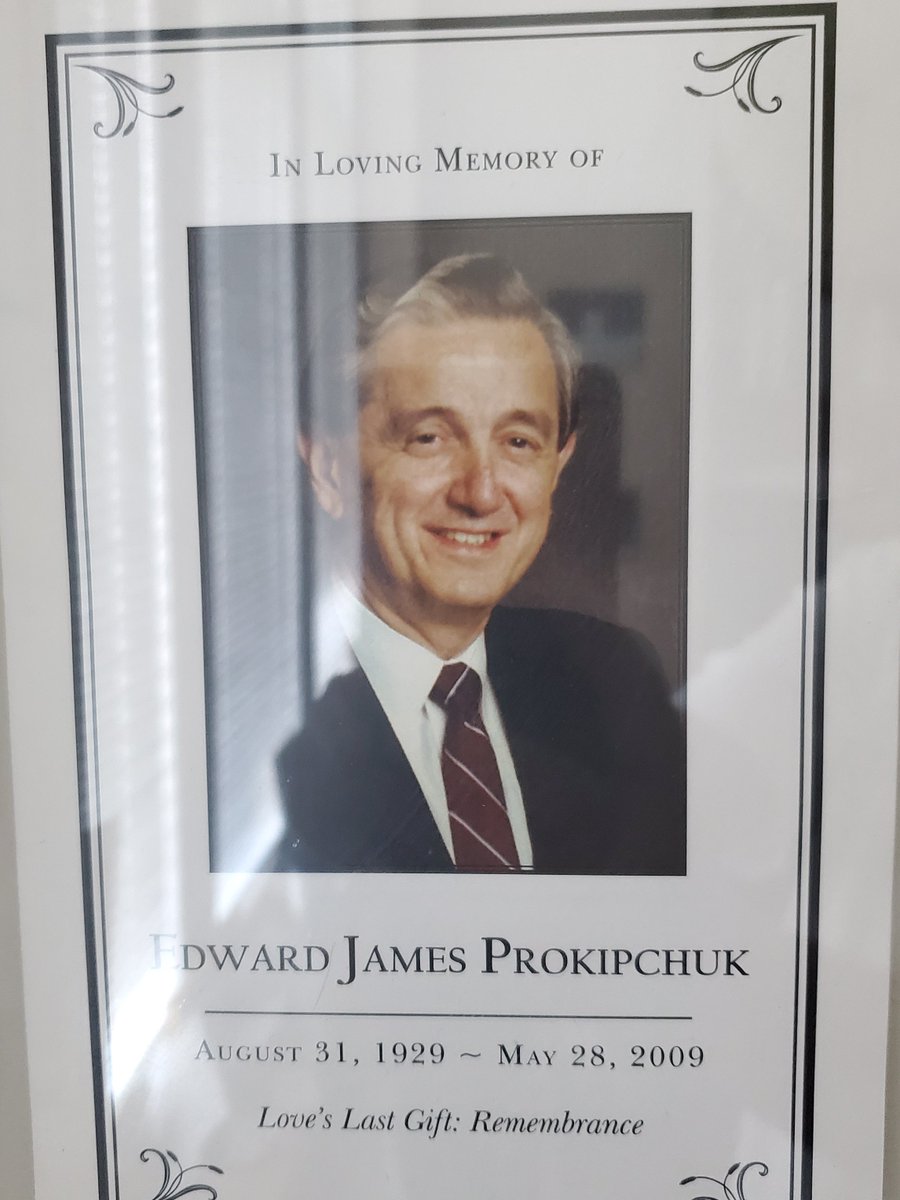
My mentor Jim Kitchens @UnityHealthTO demonstrated this once & it stuck w/ me. 3 learners - me (CC3); a bright R1 in IM & cardiology bound R3
Rounds on MR
He asked me to describe MR murmur (easy)
R1 - which gallop is likely in MR (harder)
R3 - what can an S4 mean in MR (hardest)
Rounds on MR
He asked me to describe MR murmur (easy)
R1 - which gallop is likely in MR (harder)
R3 - what can an S4 mean in MR (hardest)
We apply this to endoscopy education
e.g. for our first-year boot camp - we start new learners on simple box simulators
then onto computer sims. Then add virtual patients, assistants, etc. Then real world.
Progression in challenge improves performance + clinical transfer
e.g. for our first-year boot camp - we start new learners on simple box simulators
then onto computer sims. Then add virtual patients, assistants, etc. Then real world.
Progression in challenge improves performance + clinical transfer
As adult learners, medical trainees thrive on challenge.
You'd be amazed what they can do when given an opportunity to tackle something complex.
You'd be amazed what they can do when given an opportunity to tackle something complex.
3. Give learners autonomy
Entrust learners. Don't be afraid to let them figure out their ways of doing things as long as you are around to help.
Here's one time think I did it well when supervising my now colleague @jmosko29 on a case of massively bleeding rectal varices.
Entrust learners. Don't be afraid to let them figure out their ways of doing things as long as you are around to help.
Here's one time think I did it well when supervising my now colleague @jmosko29 on a case of massively bleeding rectal varices.
GI resident was @jmosko29 & my wife @nadabachi was surgery resident. 1st time they met
I knew they were smart cookies. I let them do their thing while I came in.
They had devised a way to inflate a Blakemore tube for rectal tamponade when I arrived to glue the varices.
Genius.
I knew they were smart cookies. I let them do their thing while I came in.
They had devised a way to inflate a Blakemore tube for rectal tamponade when I arrived to glue the varices.
Genius.

The @Royal_College in Canada has a "Competence by Design" framework based on some really sound theory on assessment
Learners are "entrusted" with tasks & assessed on entrustability.
Faculty should take this to heart. It's ok to let go.
It's the most important part of learning.
Learners are "entrusted" with tasks & assessed on entrustability.
Faculty should take this to heart. It's ok to let go.
It's the most important part of learning.

4. Be authentic
I've been listening to a lot of @naval lately and one of his mantras is that no one can outcompete you at being you. It holds for teachers as well.
The value you have as a teacher comes best when you teach authentically true to yourself.
I've been listening to a lot of @naval lately and one of his mantras is that no one can outcompete you at being you. It holds for teachers as well.
The value you have as a teacher comes best when you teach authentically true to yourself.
I've even been introspective about it - making content, modes of delivery, even assessment schema that are true to me as educator, within my bailiwick.
About 15 yrs ago my friends @RToubassi @KashPrime &al took a trip for the 1st time and we were kind of amazed by seeing art.
About 15 yrs ago my friends @RToubassi @KashPrime &al took a trip for the 1st time and we were kind of amazed by seeing art.
We'd never really seen museums before and were fascinated by art - colours, shapes, knowing the artists and what they were experiencing.
It sort of seemed similar to endoscopic images - colours, and shapes that you had to decipher.
So I started doing rounds on art and endoscopy
It sort of seemed similar to endoscopic images - colours, and shapes that you had to decipher.
So I started doing rounds on art and endoscopy

I put them on every 6 mo or so to PGY1-3s who haven't seen much endoscopy.
It's fun - we go through paintings. I just ask about colours and shapes - and I tell them the little I learned about art.
Then we do endoscopy images & ask the same questions. And get great answers.
It's fun - we go through paintings. I just ask about colours and shapes - and I tell them the little I learned about art.
Then we do endoscopy images & ask the same questions. And get great answers.

It's authentic to me. It's based on the stuff I like.
I get excited about it. I actually love giving these rounds.
Teachers - think about what makes you "you". Bring it into your #MedEd.
No one else can do it. It'll make you unstoppable.
I get excited about it. I actually love giving these rounds.
Teachers - think about what makes you "you". Bring it into your #MedEd.
No one else can do it. It'll make you unstoppable.
5. Have fun.
Now you learn in any circumstance - so much learning in my life has taken place in tough/unpleasant situations.
But people gravitate toward fun things. When your rounds, seminars, small groups, sims, are enjoyable and fun - it's like a switch turns on in learners.
Now you learn in any circumstance - so much learning in my life has taken place in tough/unpleasant situations.
But people gravitate toward fun things. When your rounds, seminars, small groups, sims, are enjoyable and fun - it's like a switch turns on in learners.
We joke, laugh, get to know each other, do fun things during teaching. We've made "serious" games.
And I think it's part of the package is being delivered.
Fun accentuates knowledge and skill acquisition.
And I think it's part of the package is being delivered.
Fun accentuates knowledge and skill acquisition.

And you can enjoy clinical medicine and education without being untrue to patient care.
There's a time and a place for everything - but it's definitely possible to remain empathic to difficult patient situations while teaching and remaining upbeat.
There's a time and a place for everything - but it's definitely possible to remain empathic to difficult patient situations while teaching and remaining upbeat.
These would be the five highlights I would put forth to the #meded community when aspiring for excellence in clinical teaching.
I'd love comments and thoughts from educators, learners, and other stakeholders.
#medtwitter #gitwitter
I'd love comments and thoughts from educators, learners, and other stakeholders.
#medtwitter #gitwitter

• • •
Missing some Tweet in this thread? You can try to
force a refresh