
1) Welcome to a new #accredited #tweetorial on #Bronchiectasis (#NCFB or #bronchiectasis) & its management, by Christina Thornton MD (@Cthornton32), respirologist & clinician scientist in Calgary 🇨🇦. Follow along and earn 0.75h CE/#CME #physicians #nurses #NPs #PAs #pharmacists! 

2) I am very excited to be among the founding faculty in this initiative! FOLLOW US for awesome expert-led education #pulmtwitter!
👍@BronchiectasisR @COPDFoundation @EMBARCnetwork @ELF @profJDchalmers @sunjayMD @DrHollyKeir @becleartoday @ephesians_1_7 @NTMinfo @AlibertiStefano
👍@BronchiectasisR @COPDFoundation @EMBARCnetwork @ELF @profJDchalmers @sunjayMD @DrHollyKeir @becleartoday @ephesians_1_7 @NTMinfo @AlibertiStefano
3) This program is supported by an educational grant from Insmed & is intended for healthcare professionals. Statement of accreditation and faculty disclosures at pulmonarymed-ce.com/disclosures/. CE/#CME credit from @academiccme.
4a) Let's start with a case! A 40F non-smoker presents with progressive dyspnea over 12 wks & one cup daily of productive sputum. PMHx is significant for asthma in childhood & no FamHx of lung disease. 

4b) Her #CF testing previously was negative. A #CXR was done that was reported as normal. What do you do next?
A. Spirometry.
B. CT Chest.
C. Obtain sputum culture, sensitivity +/- AFB +/- fungal.
D. All of the above.
A. Spirometry.
B. CT Chest.
C. Obtain sputum culture, sensitivity +/- AFB +/- fungal.
D. All of the above.
5a) Answer: D: #Bronchiectasis is a multi-modal diagnosis. CXR has limited sensitivity and specificity when diagnosis bronchiectasis especially in mild disease. Thin-section CT has higher sens/spec of 88% and 74%, respectively.
5b) Spirometry evaluates degree of disease. Sputum cultures may help direct etiology and management.
🔓pubmed.ncbi.nlm.nih.gov/30687502/
🔓pubmed.ncbi.nlm.nih.gov/30687502/
6) You get further history from the patient while ordering your tests. What conditions are associated with bronchiectasis?
7) Answer D. #NCFB is associated with many etiologies (>50!!) and are very dependent on age, sex, and geographic location. A complete and detailed history is important to help decide the cause. The most common causes are listed below.
🔓 pubmed.ncbi.nlm.nih.gov/28630359/
🔓 pubmed.ncbi.nlm.nih.gov/28630359/

9a) The CT scans show proximal bronchiectasis with mucoid impaction in a classic #fingeringlove sign with bronchial wall thickening. Now that we are thinking about it….
9b) What are some CT signs of #bronchiectasis?
A. Bronchoarterial ratio >1
B. Lack of tapering
C. Airway visibility within 1cm of costal pleural surface
D. All of the above
A. Bronchoarterial ratio >1
B. Lack of tapering
C. Airway visibility within 1cm of costal pleural surface
D. All of the above
10) Answer D. All of the above. CT scan is the current gold standard of diagnosis. While #MRI has been used in research settings, it’s not ready for prime time!
🔓ncbi.nlm.nih.gov/pmc/articles/P…
🔓ncbi.nlm.nih.gov/pmc/articles/P…
11) You are concerned the patient has #NCFB. Whoa, doc! The patient says she’s never even heard of this. What is #NCFB?! 

12a) First described in 1819, #bronchiectasis refers to abnormal permanently dilated airways, which are typically cylindrical, varicose or cystic in appearance.
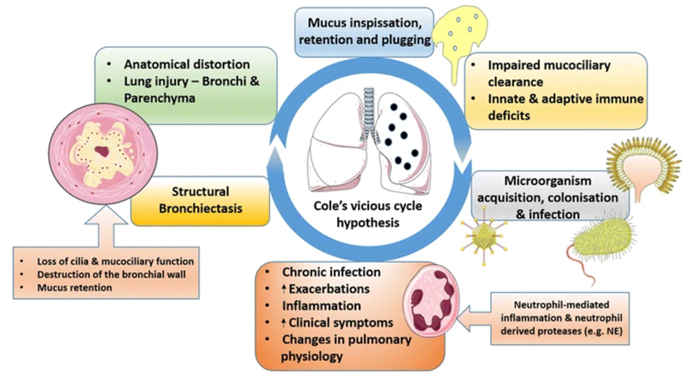
12b) #NCFB is characterized by a vicious cycle of bacterial infection and excessive #inflammation owing to impairment of airway defence mechanisms, otherwise known as the “Cole’s vicious cycle”. 
13) Why is #NCFB a big deal!? This was once considered the ‘most neglected disease in all of respiratory medicine’. While once felt to be an orphan disease, prevalence has increased by 40% in the last decade and up to >550/100,000 women (!!)
🔓 pubmed.ncbi.nlm.nih.gov/35236552/
🔓 pubmed.ncbi.nlm.nih.gov/35236552/
14) The disease is changing over the last decade—so why is #NCFB prevalence increasing?
A. Increasing public and healthcare recognition.
B. Aging population.
C. Improved sensitivity of diagnostics like CT scans (#truthteller).
D. All of the above.
A. Increasing public and healthcare recognition.
B. Aging population.
C. Improved sensitivity of diagnostics like CT scans (#truthteller).
D. All of the above.
15) Answer: D. All of the above. In particular large-scale registries in Europe, the US, India, Australia, Korea, et al 🇪🇺🇺🇸🇮🇳🇦🇺🇰🇷have improved demographics and identifying unique geographic variation for etiology, epi and micro of #NCFB.
🔓 pubmed.ncbi.nlm.nih.gov/29788932/
🔓 pubmed.ncbi.nlm.nih.gov/29788932/

16a) Back to our case. Spirometry shows airflow obstruction without bronchodilator reversibility with normal TLC and increased RV and RV/TLC ratio. You are concerned about #NCFB in this case.
16b) According to @EuroRespSoc 2017 guidelines, what is the recommended primary bundle of tests for all comers?
A. CBC
B. Immunoglobulin levels
C. Sputum culture
D. All of the above
A. CBC
B. Immunoglobulin levels
C. Sputum culture
D. All of the above
17) Answer: D. All of the above. The #ERS 2017, #BTS 2019 and #Spanish guidelines have similar recommendations but with subtle differences. Notice there are no north American guidelines! Great summary here:
🔓 pubmed.ncbi.nlm.nih.gov/35236562/
🔓 pubmed.ncbi.nlm.nih.gov/35236562/

18) While #NCFB guidelines are there across all comers, tailoring investigations based on CT pattern + clinical history + associated medical conditions is personalized to the patient.
19) So, taken together, what do you think this patient has as the cause of her #NCFB?
20) Mark your answer now and return TOMORROW for more on this case and more expert #NCFB and #bronchiectasis education!
wow! glitch much?
21) Welcome back to this #tweetorial on #NCFB and #bronchiectasis! I am @Cthornton32 & you are earning FREE CE/#CME! Thanks for joining us.
Shout-outs to @NYULangonePCCSM @EMBARCnetwork @ELF @COPDFoundation
Shout-outs to @NYULangonePCCSM @EMBARCnetwork @ELF @COPDFoundation
22) So let’s recap. We have a 40 F with asthma and productive sputum. PFTs show airflow obstruction. CT chest shows proximal bronchiectasis with mucus plugging. We ended up yesterday with a poll.
23a) Answer: C. #ABPA is a complex allergic disorder caused by immune reactions against Aspergillus fumigatus. Typical clinical presentation is poorly controlled asthma, recurrent pulmonary opacities and #bronchiectasis.
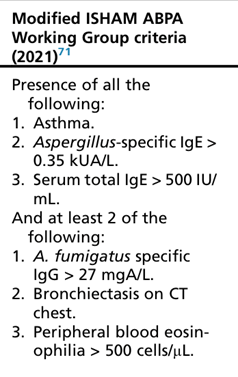
23b) Different criteria exist to define #ABPA but #ISHAM is often used. #ABPA involves predisposing conditions, #IgE elevation #Eosinophillia and exposure to the fungus.
See 🔓 pubmed.ncbi.nlm.nih.gov/35402294/
See 🔓 pubmed.ncbi.nlm.nih.gov/35402294/
24) The patient is now even more confused with this condition she has not heard of! What is the prevalence of #ABPA in #NCFB?
25) Answer: B, 1-10%. While wide ranges are reported across studies, this is in part due to lack of community data and standard diagnostic criteria.
🔓pubmed.ncbi.nlm.nih.gov/30687502/
🔓pubmed.ncbi.nlm.nih.gov/30687502/
26) The patient is quite symptomatic and wishes to pursue treatment. What is first line pharmacotherapy for #ABPA?
A. Anti-fungals (itra, vori)
B. Oral glucocorticoids
C. Anti-IgE drugs (ex: Omalizumab)
D. Anti-IL5 drugs (ex: Benralizumab)
A. Anti-fungals (itra, vori)
B. Oral glucocorticoids
C. Anti-IgE drugs (ex: Omalizumab)
D. Anti-IL5 drugs (ex: Benralizumab)
27) Answer: B. Oral glucocorticoids are the mainstay of treatment given the allergic response. Antifungals may be given as an alternative or adjunct if refractory. Use of other agents including anti-Th2 biologics are often needed in refractory cases.
🔓 pubmed.ncbi.nlm.nih.gov/35236565/
🔓 pubmed.ncbi.nlm.nih.gov/35236565/

28a) You treat the patient for #ABPA for four months and she is in remission but is left with bronchiectasis. One year later the patient returns. Her mMRC is now a 4. She had a recent hospitalisation for #PEx and one other outpatient #PEx.
28b) #FEV1 is now 55% and BMI is 18. Her last cultures showed chronic PA. You review her CT scan and see she has more than 3 lobes affected. What is her #BSI?
29a) Answer: D. Her #BSI is now severe-high. BSI is a validated prognostic score helped to predict mortality and #PEx longitudinally in #NCFB. Other ones often used include #FACED.
29b) Don’t worry you don’t have to memorize it--there’s a handy calculator here: bronchiectasisseverity.com/15-2/
🔓 pubmed.ncbi.nlm.nih.gov/35236562/
🔓 pubmed.ncbi.nlm.nih.gov/35236562/

30) The patient is now very symptomatic with her #NCFB and wants to know the management plan. TBT to our #Coles hypothesis--management is complex and based on part of the cycle.
🔓 pubmed.ncbi.nlm.nih.gov/25792635/
🔓 pubmed.ncbi.nlm.nih.gov/25792635/

31) In general, underlying management as with other respiratory diseases is around good lung health including smoking cessation, vaccinations (influenza, pneumococcus and now COVID!). Identifying & treating, if possible, the underlying cause is important but not always possible.
32) Airway clearance is a cornerstones of therapy in #NCFB but one of the hardest for adherence as it is time consuming. In general, pick the modality that your patient likes and will be able to do both when well and increase when having a #PEx.
🔓 pubmed.ncbi.nlm.nih.gov/35236555/
🔓 pubmed.ncbi.nlm.nih.gov/35236555/

33) Inhaled mucolytics like #hypertonic saline have shown modest benefit with chest physiotherapy. #DNase has been shown to be harmful thus recommended against it.
🔓 pubmed.ncbi.nlm.nih.gov/25792635/
🔓 pubmed.ncbi.nlm.nih.gov/25792635/

34a) Macrolides, the jewel of respiratory medicine, has been shown to be beneficial in several studies including #BAT, #BLESS and #EMBRACE. In general, azithromycin reduces PEx frequency. #ERS recommends it in those with 3 or more PEx per year.
34b) Make sure to do your checklist:
1. Rule out NTM.
2. Monitor QTc
3. Check audiometry/warn patients.
1. Rule out NTM.
2. Monitor QTc
3. Check audiometry/warn patients.
35) While the optimal monitoring of macrolide side-effects is unknown, our small series suggests limited toxicity in most patients without pre-existing cardiac and otologic issues.
🔓 pubmed.ncbi.nlm.nih.gov/35863768/
🔓 pubmed.ncbi.nlm.nih.gov/35863768/
36a) What about all those antibiotics and bacteria we culture!? That is a #tweetorial in itself! In general, new Pseudomonas = bad news bears. There is no standard for management, but several eradication and management algorithms exist.
37) You just said #NCFB is changing rapidly in the last decade, but a lot of these therapies are older. Isn’t there anything new!? There sure is!
38a) The lung microbiome is an exciting avenue of research where we use next-generation molecular sequencing of bacteria, fungi and viruses to allow personalization and stratification of patients into their ‘phenotypes’. This is at the cutting edge of #bench to #bedside. 

38b) Very exciting work to date and more to come! #Mustreadlist @ProfJDChalmers @DrHollyKeir and many others!
🔓 pubmed.ncbi.nlm.nih.gov/33820995/
🔓 pubmed.ncbi.nlm.nih.gov/35236558/
🔓 pubmed.ncbi.nlm.nih.gov/33961805/
🔓 pubmed.ncbi.nlm.nih.gov/36108613/
🔓 pubmed.ncbi.nlm.nih.gov/35436182/
🔓 pubmed.ncbi.nlm.nih.gov/35236558/
🔓 pubmed.ncbi.nlm.nih.gov/33820995/
🔓 pubmed.ncbi.nlm.nih.gov/35236558/
🔓 pubmed.ncbi.nlm.nih.gov/33961805/
🔓 pubmed.ncbi.nlm.nih.gov/36108613/
🔓 pubmed.ncbi.nlm.nih.gov/35436182/
🔓 pubmed.ncbi.nlm.nih.gov/35236558/
39a) Eosinophils are everywhere in respiratory medicine and #NCFB is no exception. Eosinophilic bronchiectasis affects approximately 20% of patients! But what about long-term?
39b) After treatment with antipseudomonal abx, those with higher blood eos had shorter time to #PEx. @ProfJDChalmers @DrHollyKeir
🔓 pubmed.ncbi.nlm.nih.gov/35050830/
🔓 pubmed.ncbi.nlm.nih.gov/35050830/

40a) This is all well and exciting research, but is there any new therapies available now? There sure is! #Brensocatib is the newest kid on the block. This reversible inhibitor of #DPP_1 acts to reduce activation of #neutrophil serine proteases.
40b) In the 24-week trial, there was reduction of #PMN proteases along with longer time to next #PEx. These are exciting results from the latest phase 2 study! @ProfJDChalmers
pubmed.ncbi.nlm.nih.gov/32897034/
pubmed.ncbi.nlm.nih.gov/32897034/

41) The #ASPEN trial is a phase 3 RCT placebo-controlled study ongoing for subjects with #NCFB anticipated to end in 2024. We can’t wait for the results!
clinicaltrials.gov/ct2/show/NCT04…
clinicaltrials.gov/ct2/show/NCT04…
42) In summary, #NCFB is characterized by symptoms & radiographic findings w/ heterogenous etiologies. This is not a ‘one size fit all’ disease & requires multimodal care with the patient at the centre of care. This is an exciting time with advancements in therapy & more to come! 

43) Patients and families can access additional resources and support through advocacy organizations such as @EMBARCnetwork: bronchiectasis.eu/patient-resour…, @EuropeanLung: europeanlung.org/lung-disease-a… and @COPDFoundation : copdfoundation.org/About-Us/Who-W…
44) Resources for the #keeners include the #BTS 2019 guidelines and the #ERS 2017 guidelines.
🔓 thorax.bmj.com/content/74/Sup…
🔓 erj.ersjournals.com/content/50/3/1…
🔓 erj.ersjournals.com/content/58/2/2…
🔓 thorax.bmj.com/content/74/Sup…
🔓 erj.ersjournals.com/content/50/3/1…
🔓 erj.ersjournals.com/content/58/2/2…
46) And that's it--you made it! 🆓 CE/#CME! Just go to pulmonarymed-ce.com/foundations-nf… to claim your credit. And please FOLLOW @pulmmed_CE for more expert-authored programs! I am @Cthornton32
#FOAMed
#FOAMed
• • •
Missing some Tweet in this thread? You can try to
force a refresh






