1/Does the work up for dizziness make your head spin?
Wondering what you should look for on an MRI for dizziness?
Here’s a #tweetorial on what you can (and can’t) see on MRI in #dizziness
#medtwitter #meded #neurotwitter #neurorad #radres #HNrad #neurotwitter #stroke #FOAMed
Wondering what you should look for on an MRI for dizziness?
Here’s a #tweetorial on what you can (and can’t) see on MRI in #dizziness
#medtwitter #meded #neurotwitter #neurorad #radres #HNrad #neurotwitter #stroke #FOAMed

2/The etiology for dizziness depends both on how you define dizziness (i.e., vertigo, imbalance) & where you see the patient
For imaging, subtle distinctions in symptoms usually aren’t provided & many common diagnoses are without imaging findings (BPPV, vestibular migraine)
For imaging, subtle distinctions in symptoms usually aren’t provided & many common diagnoses are without imaging findings (BPPV, vestibular migraine)

3/The most important finding on imaging for dizziness is a stroke from vertebrobasilar insufficiency (VBI)
It's a relatively uncommon etiology of dizziness, but its prevalence increases in emergent/acute dizziness populations
Missed VBI can have profound consequences/morbidity.
It's a relatively uncommon etiology of dizziness, but its prevalence increases in emergent/acute dizziness populations
Missed VBI can have profound consequences/morbidity.

4/Dizziness from VBI usually isn’t isolated bc many structures are in close proximity in brainstem/cerebellum, so it's rare for an infarct to only affect vestibular structures.
I remember this bc the brainstem is a VIP & VIPs are never alone, they always have an entourage.
I remember this bc the brainstem is a VIP & VIPs are never alone, they always have an entourage.

5/However, VBI can result in some strokes that present w/only dizziness (nodulus, CN8 root entry, labyrinth & vestibular nucleus).
Importantly, it's not uncommon for there to be a false negative on DWI in the first 24 hrs—so repeat imaging is key if suspicion is high!
Importantly, it's not uncommon for there to be a false negative on DWI in the first 24 hrs—so repeat imaging is key if suspicion is high!

6/Even in the outpatient setting, you should look for remote infarcts that may indicate VBI as a possible etiology of dizziness (remote PICA infarcts, basilar lacunes), even if there is no acute infarct at the time of exam 

7/Next most important finding after stroke is tumor. Most common tumor causing dizziness is a vestibular schwannoma.
A typical ice cream cone appearance is seen—w/the scoop of ice cream as the CP angle component & cone as the long internal auditory canal component
A typical ice cream cone appearance is seen—w/the scoop of ice cream as the CP angle component & cone as the long internal auditory canal component

8/Technically, these tumors should NOT be called an acoustic neuromas—as most arise from the vestibular not cochlear nerve. And they are schwannomas, not neuromas—neuromas are a nerve's response to injury, not a neoplasm 

9/Next most important after tumor is inflammation. Labyrinthitis can have several different appearances on imaging.
Normally the labyrinth should look clean on imaging—clear fluid, without enhancement. Like a perfectly clean living room with no mess
Normally the labyrinth should look clean on imaging—clear fluid, without enhancement. Like a perfectly clean living room with no mess

10/Acute labyrinthitis is where inflammation goes crazy, like a wild party. Inflammatory cells come into the labyrinth like random people crashing your house party
And like any party—the bright lights are on = enhancement. Acute labyrinthitis enhances on post-contrast imaging
And like any party—the bright lights are on = enhancement. Acute labyrinthitis enhances on post-contrast imaging

11/Chronic labyrinthitis follows acute labyrinthitis. So it’s the party aftermath. Trash fills the room
Similarly, fibroblasts & debris fill the labyrinth in the chronic stage, so you lose your normal clean fluid signal (so it’s dark T2). Party is over, so no lights/enhancement
Similarly, fibroblasts & debris fill the labyrinth in the chronic stage, so you lose your normal clean fluid signal (so it’s dark T2). Party is over, so no lights/enhancement

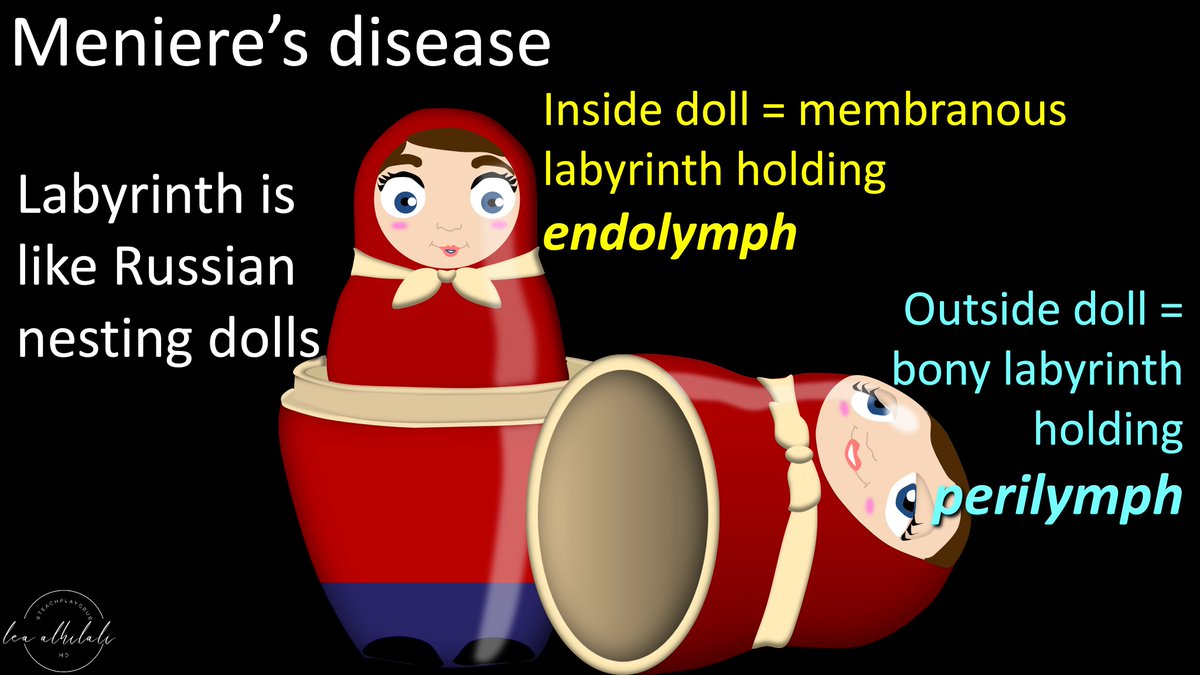
12/Finally, hardest diagnosis is Meniere’s dz (endolymphatic hydrops)
What is endolymph? Labyrinth has layers, like Russian nesting dolls
Outer doll is the bony labyrinth, holding perilymph & a 2nd doll—the membranous labyrinth
Inside the 2nd doll/mem. labyrinth is endolymph
What is endolymph? Labyrinth has layers, like Russian nesting dolls
Outer doll is the bony labyrinth, holding perilymph & a 2nd doll—the membranous labyrinth
Inside the 2nd doll/mem. labyrinth is endolymph
13/Think of the labyrinth like a worm. It has its outer skin, but inside the skin is an intestine like a Russian nesting doll. Instestine is the mem. labyrinth holding endolymph
Endolymphatic hydrops is like when the worm eats too much & the intestine gets big inside the skin.
Endolymphatic hydrops is like when the worm eats too much & the intestine gets big inside the skin.

14/To understand imaging for endolymphatic hydrops, you must understand some labyrinth anatomy
In the coronal plane, labyrinth looks like a bow tie, w/the utricle/semicircular canals on top & cochlea on the bottom. Knot in the middle is the saccule—an important marker in hydrops
In the coronal plane, labyrinth looks like a bow tie, w/the utricle/semicircular canals on top & cochlea on the bottom. Knot in the middle is the saccule—an important marker in hydrops

15/When looking at the vestibule in the coronal plane, the utricle is on top & the saccule is on the bottom
You can remember utricle is superior bc U is for both Utricle & up
You can remember the saccule is inferior bc it hangs down like a sack.
You can remember utricle is superior bc U is for both Utricle & up
You can remember the saccule is inferior bc it hangs down like a sack.

16/So how to image hydrops?
Remember the worm. If a worm is put in dye, it’ll absorb dye into its skin, but not its intestine
Same for the labyrinth. If you give contrast, it’s absorbed into the perilymph, but not endolymph—allowing us to see the endolymph as a filling defect
Remember the worm. If a worm is put in dye, it’ll absorb dye into its skin, but not its intestine
Same for the labyrinth. If you give contrast, it’s absorbed into the perilymph, but not endolymph—allowing us to see the endolymph as a filling defect

17/You must give the contrast via tympanic injection or wait 2 hrs or more after IV injection. Then perilymph will be bright & endolymph dark
On delayed axial post images, vestibular structures look like a bird. Body is perilymph & eye/belly are filling defects from endolymph
On delayed axial post images, vestibular structures look like a bird. Body is perilymph & eye/belly are filling defects from endolymph
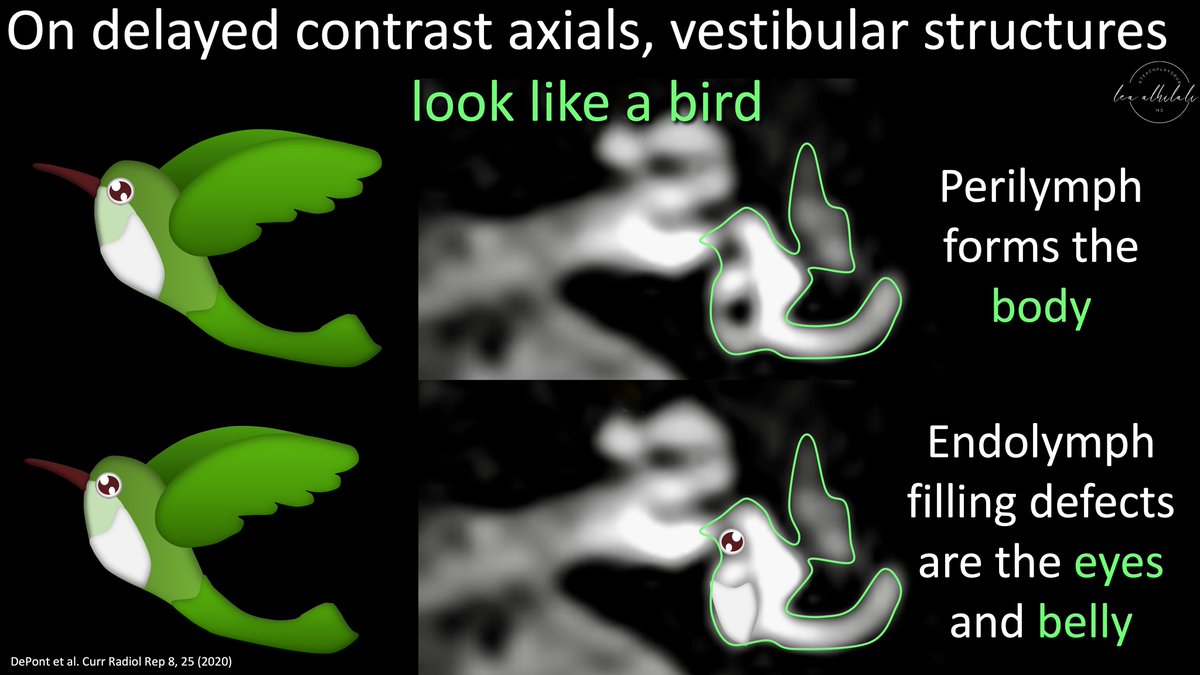
18/The filling defect that looks like an eye is the saccule endolymph. I remember this bc it’s the SACCule & eyes have SACCades
The belly filling defect is the endolymph in the utricle. You can remember this bc utricle means pouch (like uterus) & the belly is just a big pouch
The belly filling defect is the endolymph in the utricle. You can remember this bc utricle means pouch (like uterus) & the belly is just a big pouch

19/An early hydrops sign is when the saccule endolymph gets enlarged (hydropic). Bird’s eye gets huge & runs into the belly
Utricle endolymph may also be hydropic—then you see big eye & belly
Remember when you are dizzy/high, your eyes are wide and your belly get big!
Utricle endolymph may also be hydropic—then you see big eye & belly
Remember when you are dizzy/high, your eyes are wide and your belly get big!

20/Seeing a giant bird’s eye is a common sign of hydrops.
Bird’s eye (saccule endolymph) is usually smaller than the belly (utricle endolymph). In hydrops, this is often reversed—called SURI or saccule to utricle inversion ratio.
Larger the bird’s eye, the more hydrops.
Bird’s eye (saccule endolymph) is usually smaller than the belly (utricle endolymph). In hydrops, this is often reversed—called SURI or saccule to utricle inversion ratio.
Larger the bird’s eye, the more hydrops.

21/But what if there’s no delayed contrast imaging? It’s not usually done & it’s burdensome to wait several hours
Is there a non-contrast finding to help us select who may benefit from delays? We can use saccular morphology. On coronals, vestibular structures look like a rabbit
Is there a non-contrast finding to help us select who may benefit from delays? We can use saccular morphology. On coronals, vestibular structures look like a rabbit

22/Bunny ears are the semicircular canals, eyes/forehead are the utricle, & the nose is the saccule.
The morphology of that saccular nose is key to telling us if there is hydrops. Too large a nose or not seeing the nose at all suggests hydrops
The morphology of that saccular nose is key to telling us if there is hydrops. Too large a nose or not seeing the nose at all suggests hydrops
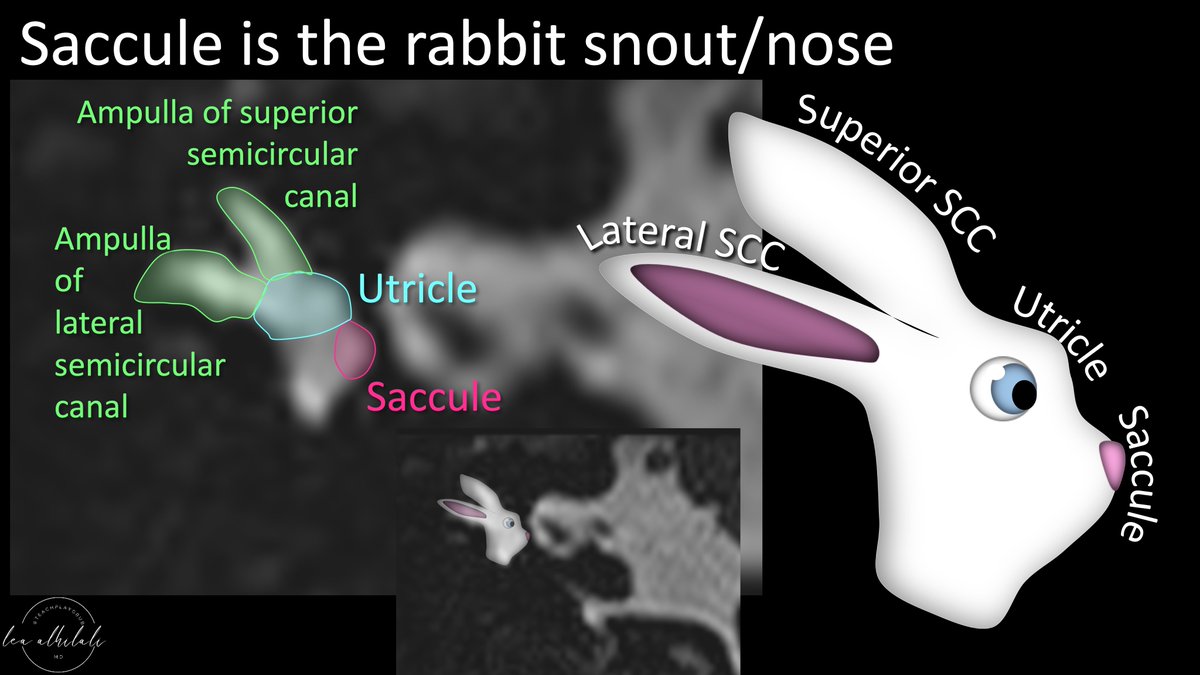
23/Too big a nose or no nose are very specific for hydrops.
There are measurements to define too long a nose (>1.5mm)—but it’s just a screening tool to see who needs delayed contrast imaging, so look for the abnormal morphology before you break out the calipers!
There are measurements to define too long a nose (>1.5mm)—but it’s just a screening tool to see who needs delayed contrast imaging, so look for the abnormal morphology before you break out the calipers!

24/So for every MRI for dizziness, remember the mnemonic VESTIbular to remind you what to look for:
V for vestibular schwannoma
E for endolymphatic hydrops
S & T for stroke/TIA
I for internal otitis (labyrinthitis)
Hopefully now an MRI for dizziness won’t put you off balance!
V for vestibular schwannoma
E for endolymphatic hydrops
S & T for stroke/TIA
I for internal otitis (labyrinthitis)
Hopefully now an MRI for dizziness won’t put you off balance!

• • •
Missing some Tweet in this thread? You can try to
force a refresh






















