Dr. Martin Bogetz, a bereaved father, sharing the legacy of his daughter Alyssa:
- an MSW who cared deeply about wellbeing
- the first non-physician associate program director in Peds at Stanford, who focused on supporting trainees
- sister of @jbogetz, #pedpc wonder ❤️ #hapc23
- an MSW who cared deeply about wellbeing
- the first non-physician associate program director in Peds at Stanford, who focused on supporting trainees
- sister of @jbogetz, #pedpc wonder ❤️ #hapc23

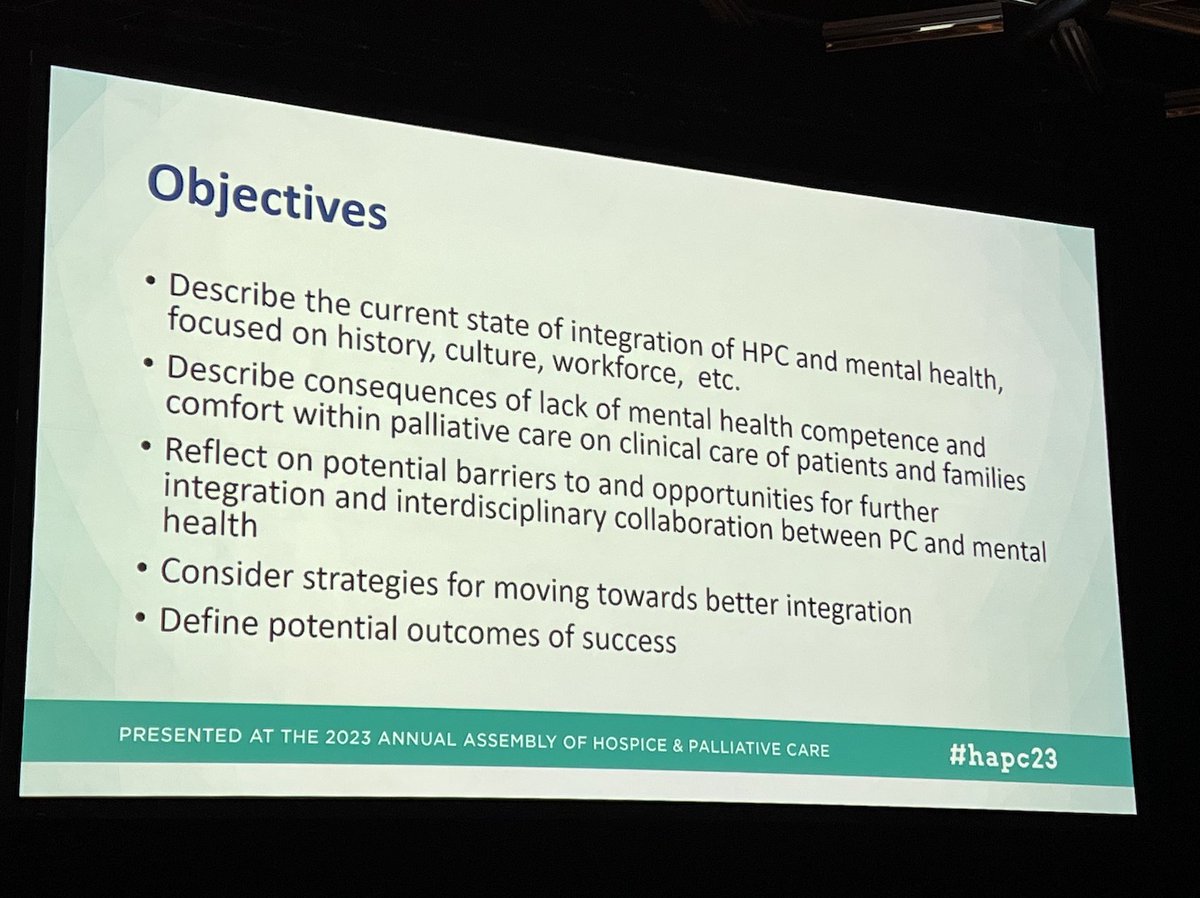
The inaugural Alyssa Bogetz lecture: Dr. Susan Block talking about the state of integration of #hapc and #mentalhealth
Alyssa died of AN. The educational fund was started in her honor @AAHPM w the appreciation that our field needs to grow to support people like her. #hapc23
Alyssa died of AN. The educational fund was started in her honor @AAHPM w the appreciation that our field needs to grow to support people like her. #hapc23
"I think it's a miracle how far we've come." - Dr. Susan Block
We are the 6th largest subspecialty of the largest specialty in the US! #hapc #pedpc #hapc23

We are the 6th largest subspecialty of the largest specialty in the US! #hapc #pedpc #hapc23


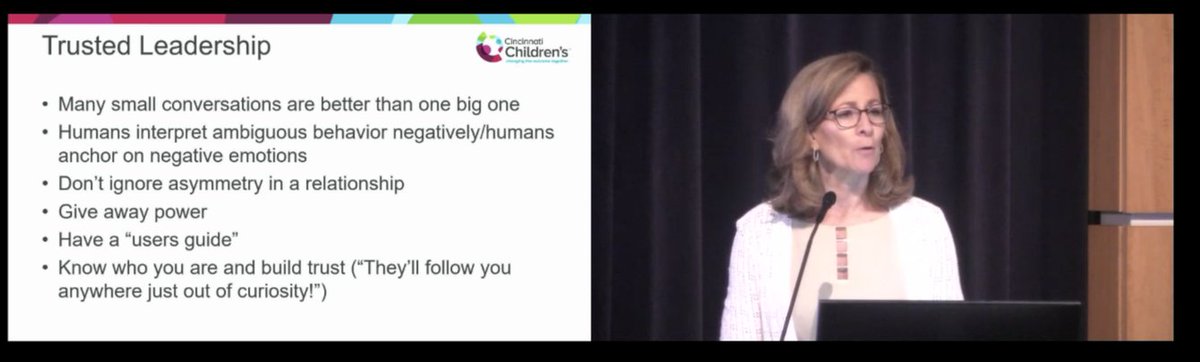
"Our field has tackled communication skills at a really high level...this is something that is quite remarkable and provides a foundation for further development of mental health competencies." - Dr. Susan Block
#hapc23
#hapc23
Yes, AND- as a result we see a much higher level of primary palliative communication skills across our system too!
We teach not just #hapc #pedpc fellows, but also #ICU, #hemonc and other trainees.
Care confs are much better than they used to be! (-me) #hapc23
We teach not just #hapc #pedpc fellows, but also #ICU, #hemonc and other trainees.
Care confs are much better than they used to be! (-me) #hapc23
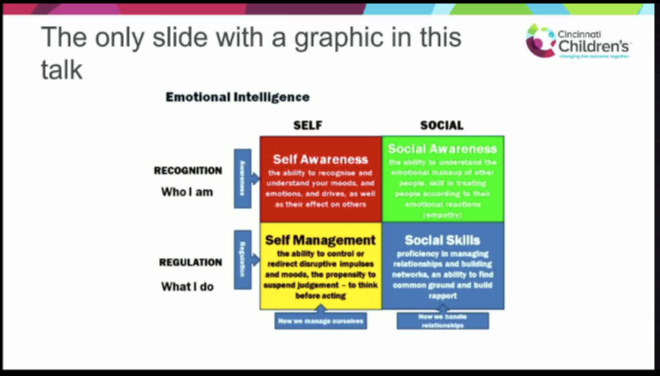
The audience feels much better prepared to manage medical issues in #hapc than psychosocial or #mentalhealth issues.
Also 74% had "a little" training in managing mental health issues.
This is critical- there is an epidemic of psych distress in the US.
#hapc23

Also 74% had "a little" training in managing mental health issues.
This is critical- there is an epidemic of psych distress in the US.
#hapc23


This is so critical. Not feeling competent in managing patients with MH issues is likely a source of burnout for #hapc clinicians.
And we aren't well trained in managing MH issues.
- Dr. Susan Block #hapc23

And we aren't well trained in managing MH issues.
- Dr. Susan Block #hapc23


"Psychological suffering always has a physical component, and physical suffering always has a psychological component...in the biomedical model, the only suffering that matters is physical." - Dr. Susan Block #hapc23
So she asked us- to what extent do challenging patients with MH issues contribute to our feelings of #burnout?
Thank you for highlighting this link, Dr. Block. #hapc23
"Competency is part of wellbeing." YES.
Thank you for highlighting this link, Dr. Block. #hapc23
"Competency is part of wellbeing." YES.

My tweet thread got messed up, sorry!
Restarting here.
Culture eats strategy for breakfast.
And stigma is real.
We have to change the culture of stigma against MH issues in #hapc, and this change starts within each of us. -Dr. Susan Block
#hapc23
Restarting here.
Culture eats strategy for breakfast.
And stigma is real.
We have to change the culture of stigma against MH issues in #hapc, and this change starts within each of us. -Dr. Susan Block
#hapc23
• • •
Missing some Tweet in this thread? You can try to
force a refresh