In this one, high intakes of seafood, and particularly small fish rich in n-3 fatty acids, was associated with a lower risk of 10-year fatal and non-fatal cardiovascular disease risk in Greek adults with a mean age of 45.2 years. 

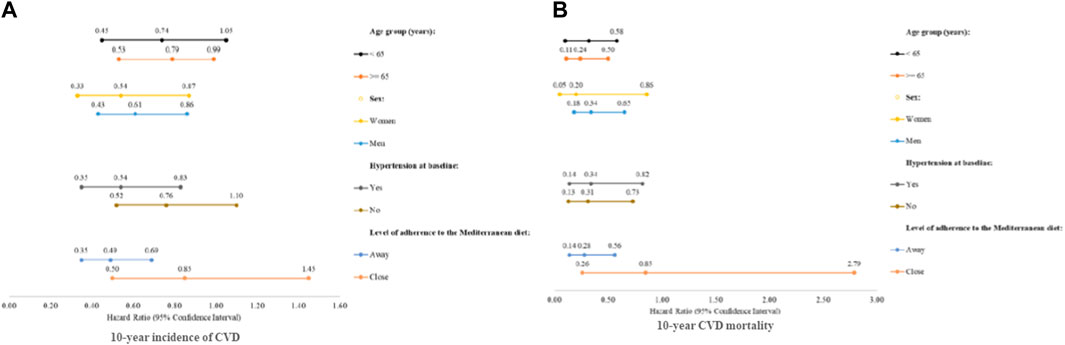

- Less than one-10th of the study participants consumed >1 serving of small fish rich in n-3 fatty acids per week.
- Participants who consumed >2 servings per week of seafood had at least 27% decreased risk of developing CVD and 74% lower 10-year risk of dying due to CVD.
- Participants with high consumption (>1 serving/week) of small fish rich in n-3 fatty acids had a significantly reduced risk of 10-year CVD incidence and exhibited a 76% decreased 10-year risk of dying due to CVD, even among normotensive individuals.
- Interestingly, when the analyses were focused on 20-year CVD incidence and mortality, even though similar associations were detected, these were not statistically significant.
High fish intake rich in n-3 polyunsaturated fatty acids reduces cardiovascular disease incidence in healthy adults: The ATTICA cohort study (2002-2022) (open access)
doi.org/10.3389/fphys.…
#nutrition #diet #PUFAs #Omega3
doi.org/10.3389/fphys.…
#nutrition #diet #PUFAs #Omega3
• • •
Missing some Tweet in this thread? You can try to
force a refresh

 Read on Twitter
Read on Twitter