Read our latest analysis from the #ADVOR trial @JACCJournals. Deeper dive into the relationship of #natriuresis with decongestion & clinical outcomes after diuretic therapy in acute #heartfailure! Tweetorial below...
authors.elsevier.com/a/1h4wr2d9GHwT…
@PieterMartensMD @WilfriedMullens
authors.elsevier.com/a/1h4wr2d9GHwT…
@PieterMartensMD @WilfriedMullens
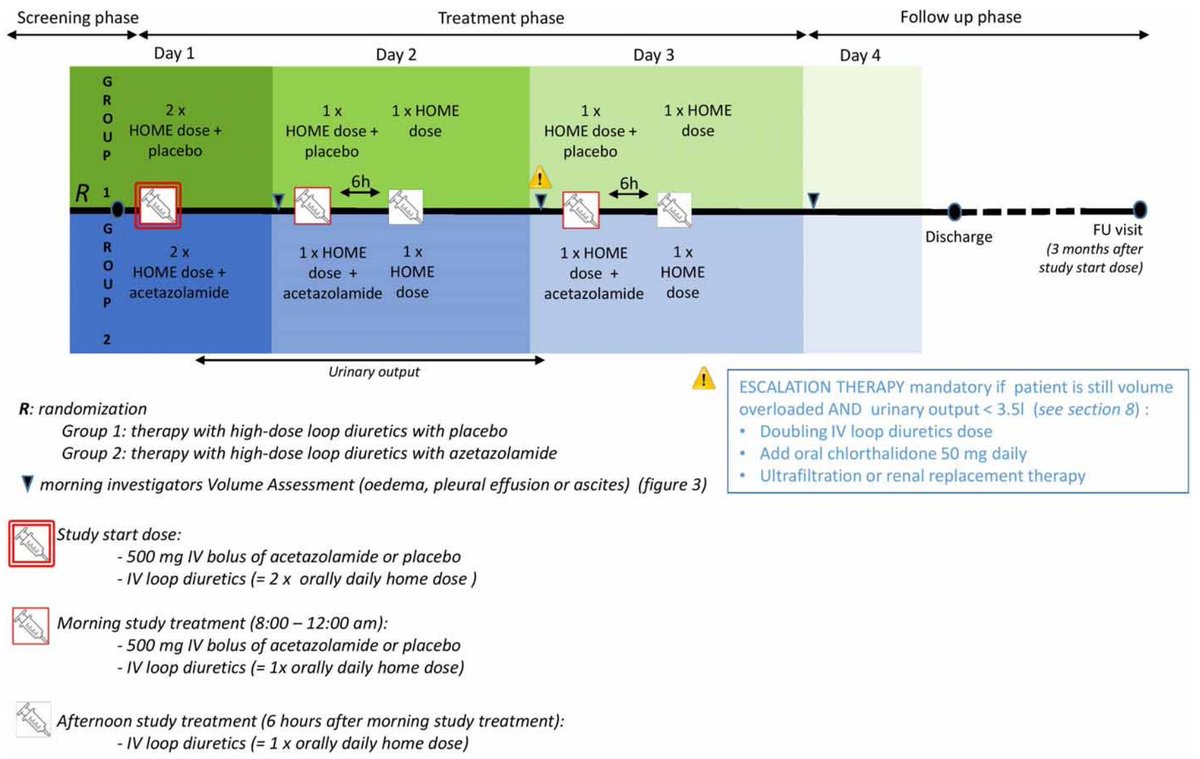
First, look at detailed #ADVOR protocol below:
onlinelibrary.wiley.com/doi/full/10.10…
We did 2 consecutive urine collections:
1. Randomization => First morning (<24 h)
2. First morning => Second morning (=24 h)
If in those 2 collections, cumulative urine output <3.5 L ➡️ Failed decongestion!
onlinelibrary.wiley.com/doi/full/10.10…
We did 2 consecutive urine collections:
1. Randomization => First morning (<24 h)
2. First morning => Second morning (=24 h)
If in those 2 collections, cumulative urine output <3.5 L ➡️ Failed decongestion!
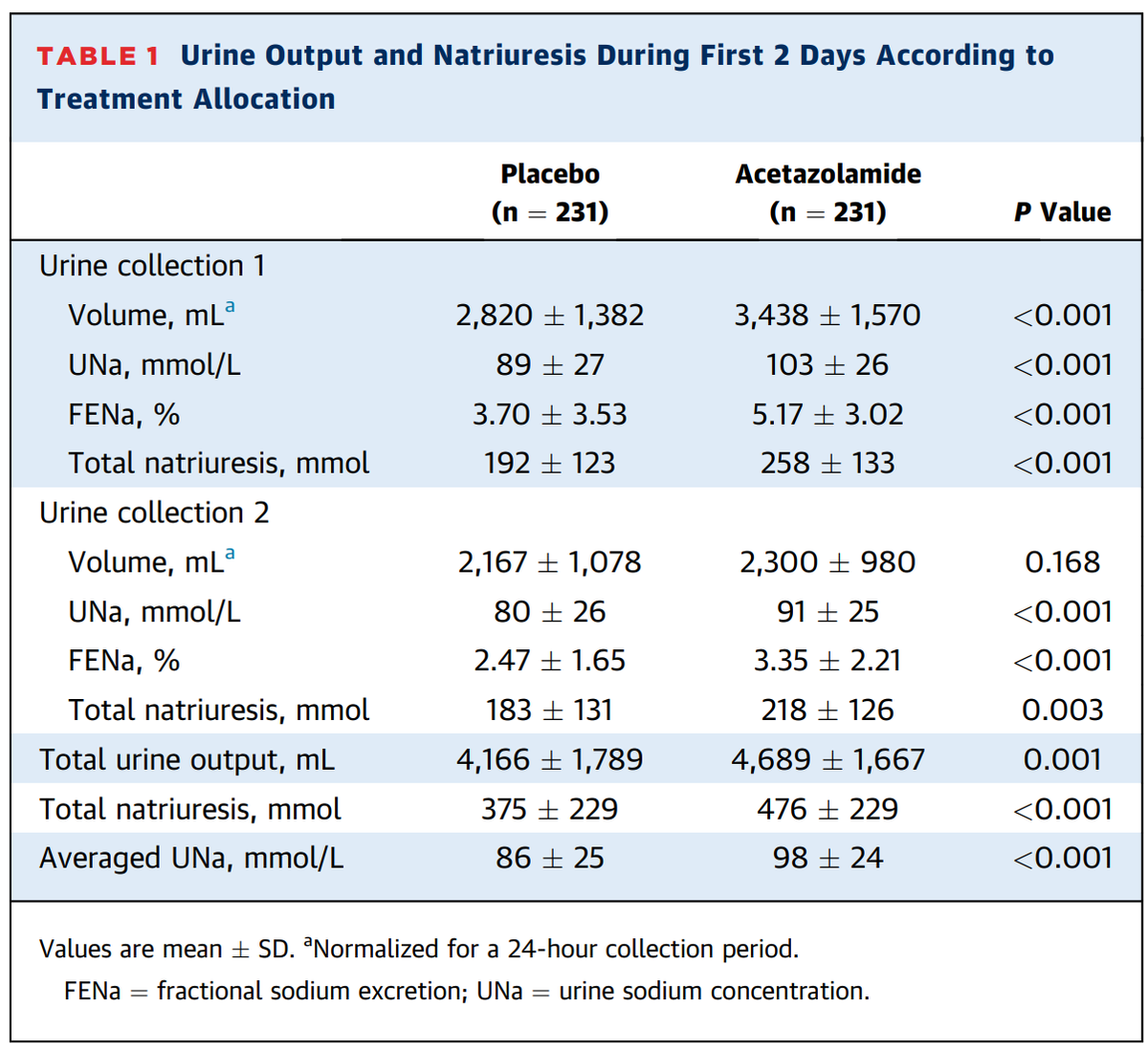
Allocation to #acetazolamide clearly increased:
✅total urine output (+12.6%)
✅total natriuresis (+26.9%)
In relative terms: effect on natriuresis > urine output, UO🚫significant after 1st diuretic dose, natriuresis remained high!
*Normalized UO to 24 h for collection 1.
✅total urine output (+12.6%)
✅total natriuresis (+26.9%)
In relative terms: effect on natriuresis > urine output, UO🚫significant after 1st diuretic dose, natriuresis remained high!
*Normalized UO to 24 h for collection 1.
Moreover, allocation to #acetazolamide by a landslide strongest predictor of both urine #sodium concentration (UNa) AND total #natriuresis (molecules excreted)!
For instance, 5-8x bigger impact than an eGFR change of 10 mL/min/1.73m²
For instance, 5-8x bigger impact than an eGFR change of 10 mL/min/1.73m²

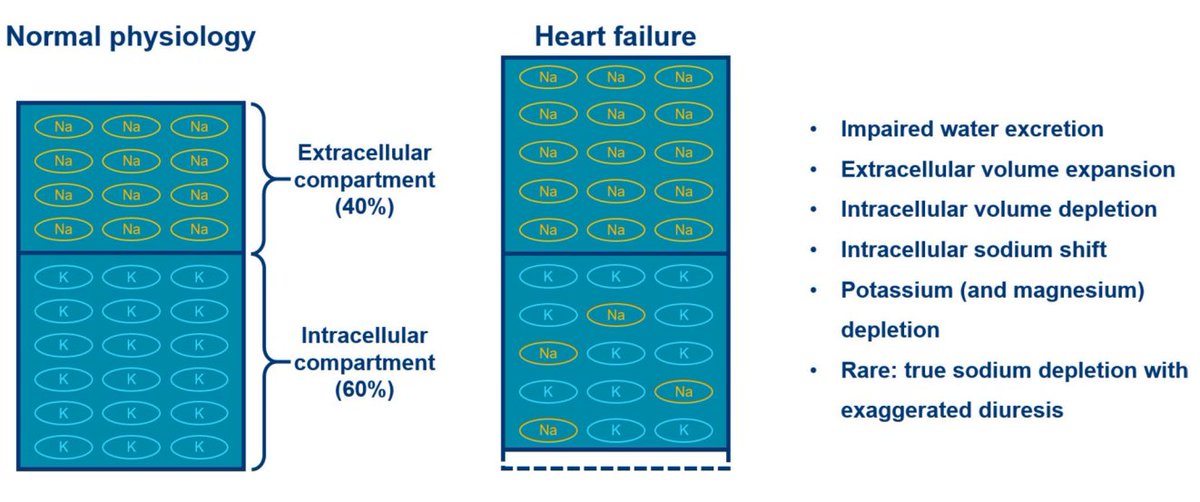
Be wary: total natriuresis and UNa not the same!
Total natriuresis tracks well with UO
➡️Amount of extracellular volume (ECV) DURABLY removed (150 mmol Na ~ 1 L ECV)
❗️Urine is usually HYPOTONIC (UNa <150 mmol/L)
➡️Part of UO reflects #dehydration rather than #decongestion
Total natriuresis tracks well with UO
➡️Amount of extracellular volume (ECV) DURABLY removed (150 mmol Na ~ 1 L ECV)
❗️Urine is usually HYPOTONIC (UNa <150 mmol/L)
➡️Part of UO reflects #dehydration rather than #decongestion

No such strong correlation between UNa & UO!
UNa:
➡️Only partly reflects decongestion
➡️Also reflects neurohumoral activation
➡️Best measurement of sodium avidity
Thus, #acetazolamide
✅Keeps sodium content of urine high, therefore allowing better decongestion for same UO!
UNa:
➡️Only partly reflects decongestion
➡️Also reflects neurohumoral activation
➡️Best measurement of sodium avidity
Thus, #acetazolamide
✅Keeps sodium content of urine high, therefore allowing better decongestion for same UO!

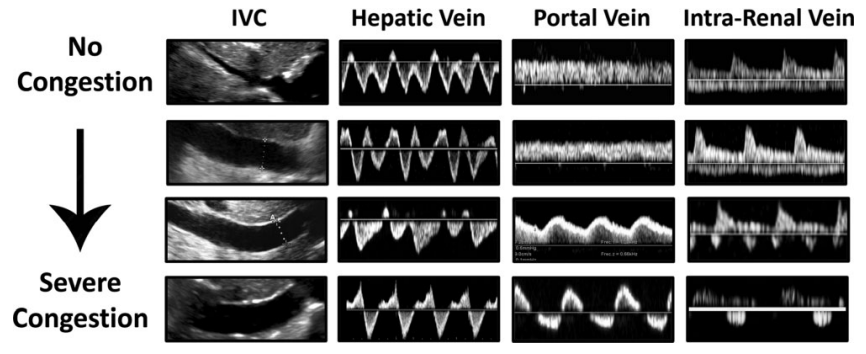
Higher UNa & greater total natriuresis
✅Associated with higher chance of successful #decongestion (no more than trace edema and no ascites/pleural effusion)
✅Associated with higher chance of successful #decongestion (no more than trace edema and no ascites/pleural effusion)

From 1st morning, patients w higher UNa (less Na avidity): significantly greater clinical decongestion!
UNa ≥80 ideal cut-off, indicating excellent response!
❗️Intriguingly, effect of #acetazolamide on decongestion🚫significant after adjustment for natriuresis➡️Mediation?
UNa ≥80 ideal cut-off, indicating excellent response!
❗️Intriguingly, effect of #acetazolamide on decongestion🚫significant after adjustment for natriuresis➡️Mediation?

Consequently, patients with better natriuresis has a shorter length of stay
✅4.5 days shorter for UNa ≥100 versus <50 mmol/L
✅4.5 days shorter for UNa ≥100 versus <50 mmol/L

As shown in other studies, better natriuretic response to #diuretics was associated with better clinical outcome (death or heart failure readmissions) 

Now the intriguing part:
Good natriuretic response (UNa ≥80 mmol/L):
➡️Similar outcome loop diuretic monotherapy & combination with acetazolamide
❗️Many more patients with #acetazoalmide had UNa ≥80 mmol/L (NNT = only 7!)
Poor natriuretic response (UNa <80 mmol/L):
🪦 &🏥
Good natriuretic response (UNa ≥80 mmol/L):
➡️Similar outcome loop diuretic monotherapy & combination with acetazolamide
❗️Many more patients with #acetazoalmide had UNa ≥80 mmol/L (NNT = only 7!)
Poor natriuretic response (UNa <80 mmol/L):
🪦 &🏥

Also, for people that are so concerned about the non-significantly🔼90-day 🪦 with #acetazolamide in #ADVOR:
* Notice LATE occurrence of this effect (45 days after randomization or >30 days after acetazolamide was stopped)
* Mostly in patients with a poor natriuretic response
* Notice LATE occurrence of this effect (45 days after randomization or >30 days after acetazolamide was stopped)
* Mostly in patients with a poor natriuretic response
My interpretation is that by the play of chance, patients in the #acetazolamide arm were probably slightly sicker.
Illustrated as well by slightly higher baseline dose of loop diuretics (80 vs. 60 mg furosemide equivalents).
Illustrated as well by slightly higher baseline dose of loop diuretics (80 vs. 60 mg furosemide equivalents).
Conclusion:
1. Upfront combination of #acetazolamide with loop diuretics in acute #heartfailure helps to keep sodium content of urine high.
2. Strong natriuresis ~ better (and more durable?) decongestion!
3. Natriuretic response ~ clinical outcomes
➡️UNa+ guided diuretic therapy
1. Upfront combination of #acetazolamide with loop diuretics in acute #heartfailure helps to keep sodium content of urine high.
2. Strong natriuresis ~ better (and more durable?) decongestion!
3. Natriuretic response ~ clinical outcomes
➡️UNa+ guided diuretic therapy
Also read this other analysis from the #ADVOR, eloquently discussed by my friend & partner in crime @PieterMartensMD :
It shows nicely that after 48 h treatment with monotherapy loop diuretics, almost every patient develops "contraction alkalosis"
https://twitter.com/PieterMartensMD/status/1655293571363110912
It shows nicely that after 48 h treatment with monotherapy loop diuretics, almost every patient develops "contraction alkalosis"
We need to rename "contraction alkalosis" to "neurohumoral alkalosis", as it is not a sign of hypovolemia per se.
Thus:
➡️Minor congestion requiring 1 or 2 doses of diuretics probably does not need #acetazolamide
➡️In case of any prolonged treatment: UPFRONT!!!
Thus:
➡️Minor congestion requiring 1 or 2 doses of diuretics probably does not need #acetazolamide
➡️In case of any prolonged treatment: UPFRONT!!!
This is a BIG difference with #thiazides, which have shown to break diuretic resistance, can wait until this occurs!
The effect of #acetazolamide resides in braking the neurohumoral system, so need to treat upfront rather than bail-out, which is how #ADVOR was set up!
The effect of #acetazolamide resides in braking the neurohumoral system, so need to treat upfront rather than bail-out, which is how #ADVOR was set up!
For the #physiology fans, here's the paper in which we discussed the proximal nephron hypothesis, leading to the #ADVOR trial @ESC_Journals :
onlinelibrary.wiley.com/doi/full/10.10…
onlinelibrary.wiley.com/doi/full/10.10…

Doing a pilot on UNa guided therapy incorporating ALL diuretic classes (#DECONGEST):
clinicaltrials.gov/ct2/show/NCT05…
@SVanhentenrijk
Don't miss out on:
- ENACT-HF at #Heartfailure2023 in Prague
- PUSH-HF, by @jozinetm & @kevin_damman @escardio 2023 in Amsterdam
clinicaltrials.gov/ct2/show/NCT05…
@SVanhentenrijk
Don't miss out on:
- ENACT-HF at #Heartfailure2023 in Prague
https://twitter.com/JeroenDauw/status/1658810146460409856
- PUSH-HF, by @jozinetm & @kevin_damman @escardio 2023 in Amsterdam
• • •
Missing some Tweet in this thread? You can try to
force a refresh