Is it important for physicians to understand mechanisms to treat heart failure? By Legendary #MiltonPacker
@HFA_President @WilfriedMullens @FH_Verbrugge @JavedButler1
@jozinetm @_antocannata @DjawidHashemi
@doctorchecho @h_arfsten
@SotiriaLiori @LauraMeems @escardio



@HFA_President @WilfriedMullens @FH_Verbrugge @JavedButler1
@jozinetm @_antocannata @DjawidHashemi
@doctorchecho @h_arfsten
@SotiriaLiori @LauraMeems @escardio


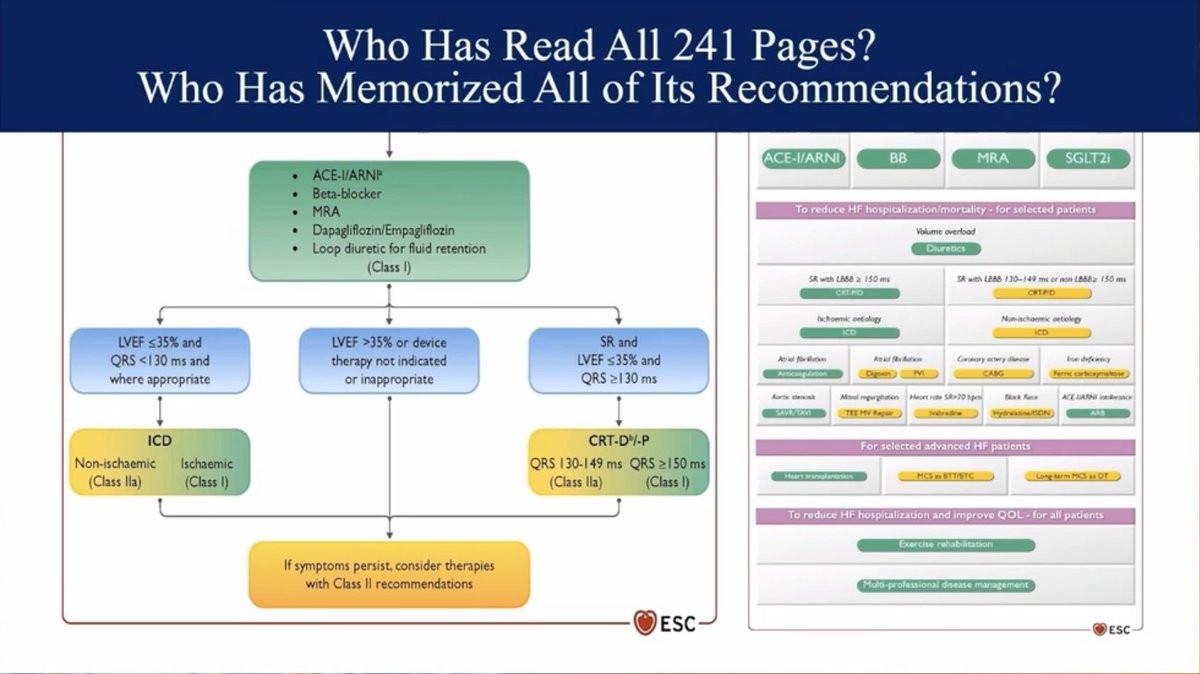

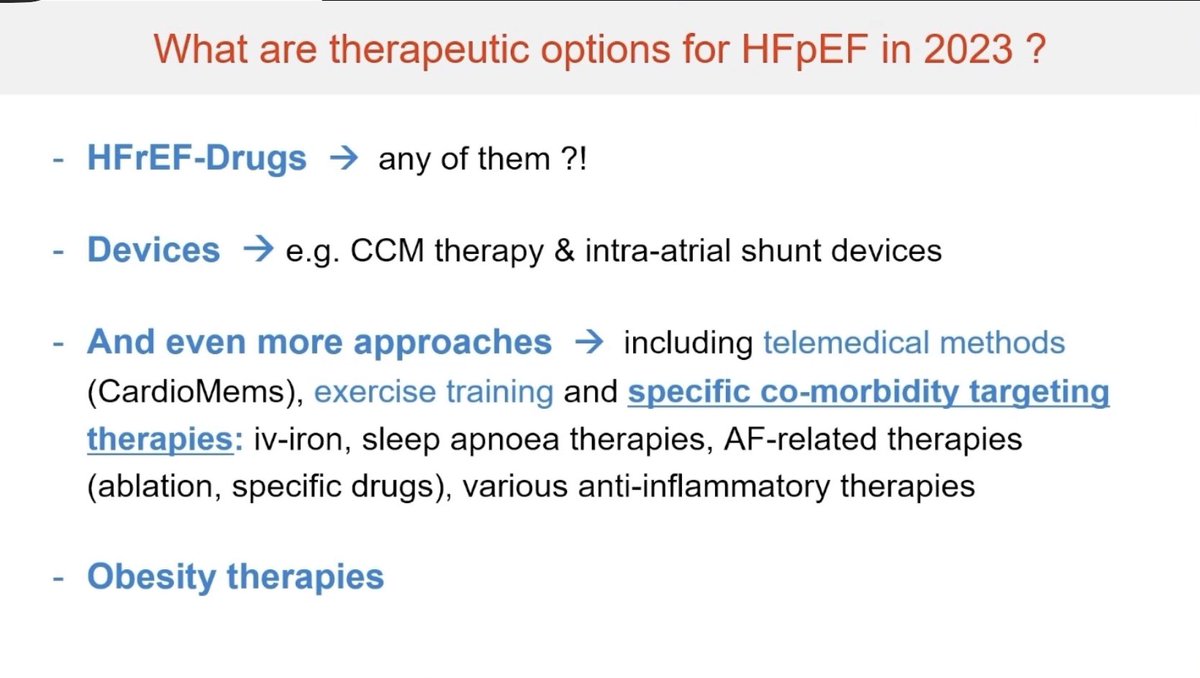
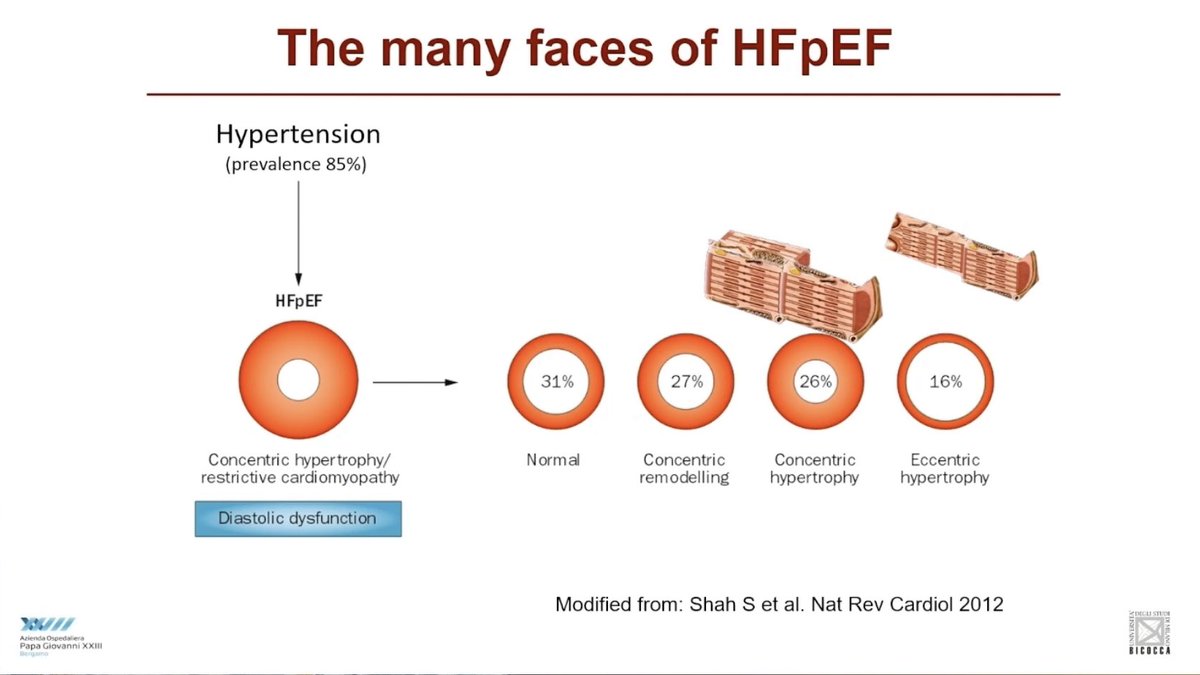
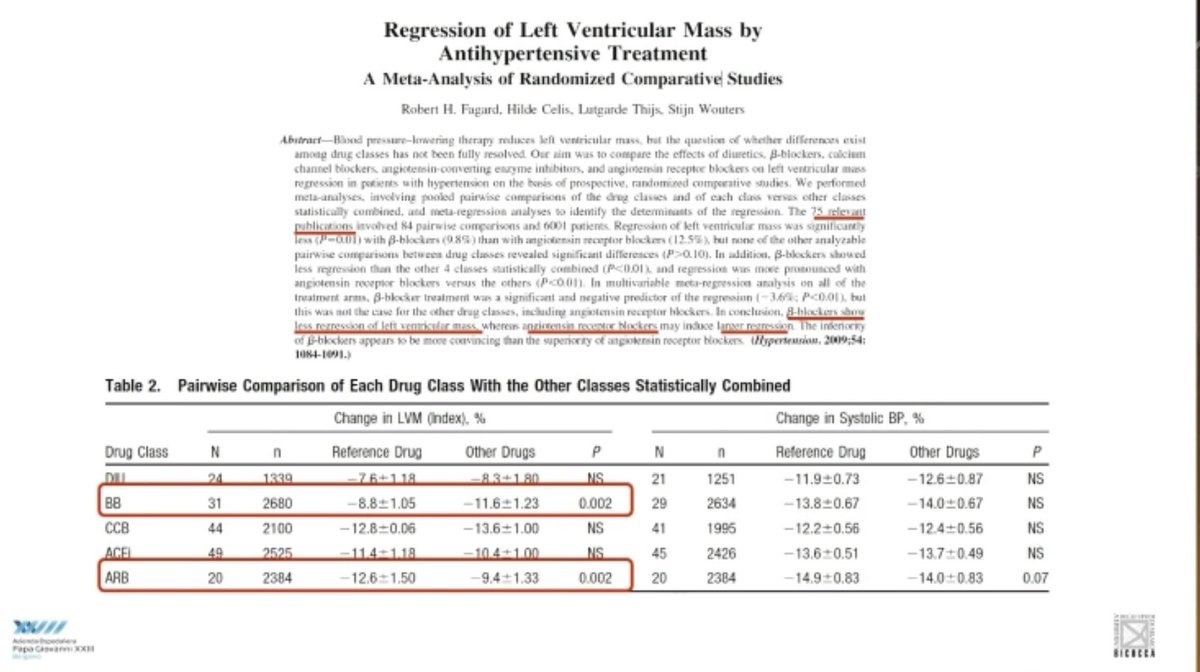
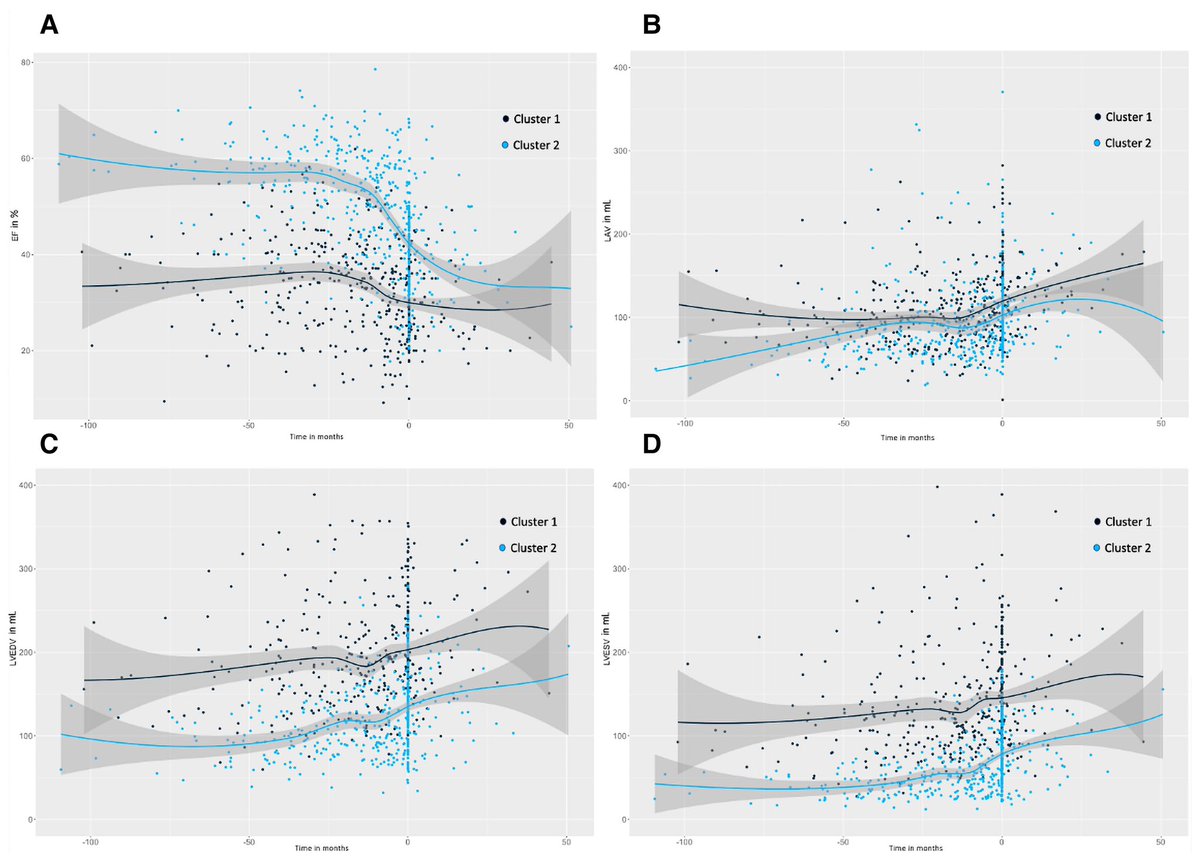
Physicians make decisions NOT by memorizing trials or guidelines, but by having a conceptual framework about drugs and diseases
#HeartFailure2023 @ESC_Journals @escardio @WilfriedMullens @HFA_President @ARakisheva @FH_Verbrugge @WilfriedMullens



#HeartFailure2023 @ESC_Journals @escardio @WilfriedMullens @HFA_President @ARakisheva @FH_Verbrugge @WilfriedMullens




How Physician Thinking and Decision-Making Is Supposed to Work
Dr. #MiltonPacker proved it in these 4 slides
#HeartFailure2023 @HFA_President @JavedButler1 @MarcoMetra @gcfmd @mmamas1973 @pabeda1 @WilfriedMullens @ESC_Journals



Dr. #MiltonPacker proved it in these 4 slides
#HeartFailure2023 @HFA_President @JavedButler1 @MarcoMetra @gcfmd @mmamas1973 @pabeda1 @WilfriedMullens @ESC_Journals




Physicians make decisions NOT by memorizing trials or guidelines, but by having a conceptual framework about drugs and diseases
#HeartFailure2023


#HeartFailure2023



• • •
Missing some Tweet in this thread? You can try to
force a refresh

 Read on Twitter
Read on Twitter