We're seeing more consult questions for this, and it's also garnering national attention, so let's take a brief moment in #tweetorial format to talk about:
XYLAZINE SKIN ULCERS!
#xylazine #MedEd #FOAMEd #dermtwitter #medtwitter
1/
XYLAZINE SKIN ULCERS!
#xylazine #MedEd #FOAMEd #dermtwitter #medtwitter
1/
What is Xylazine? It was created in the 70s as a veterinary anesthetic. As an analog of clonidine, it has similar effects as an alpha-2 agonist, leading to sedation, anesthesia, and euphoria in the CNS.
2/
2/

Recently, Xylazine has entered the drug supply, moreso in certain cities, but increasingly everywhere. It is often mixed with fentanyl as a cutting agent, and can also be used on its own. It may be called Tranq, Zombie Drug, or anestesia de caballo (horse anesthetic).
3/
3/
This is a big problem that's getting bigger. In fact, 2 months ago, the @WhiteHouse designated xylazine as an emerging threat!
whitehouse.gov/ondcp/briefing…
4/
whitehouse.gov/ondcp/briefing…
4/
Dr. Rahul Gupta, Director of the White House Office of National Drug Control Policy, also co-wrote an article in @NEJM highlighting this issue for the medical community:
nejm.org/doi/full/10.10…
5/
nejm.org/doi/full/10.10…
5/
Okay, let's get back to the clinical! There are a lot of systemic effects, but for today, I'm sticking with skin.
First of all, remember that the skin findings do NOT have to occur where the drug might be injected (injection is the most common mode of administration).
6/
First of all, remember that the skin findings do NOT have to occur where the drug might be injected (injection is the most common mode of administration).
6/
The skin ulcerations that occur are conjectured to be from a mixture of vasoconstriction in the skin, combined with decreased oxygenation of the tissue leading to necrosis. That said, it's not 100% clear. The mechanism is likely multifactorial.
PC: nejm.org/doi/full/10.10…
7/
PC: nejm.org/doi/full/10.10…
7/

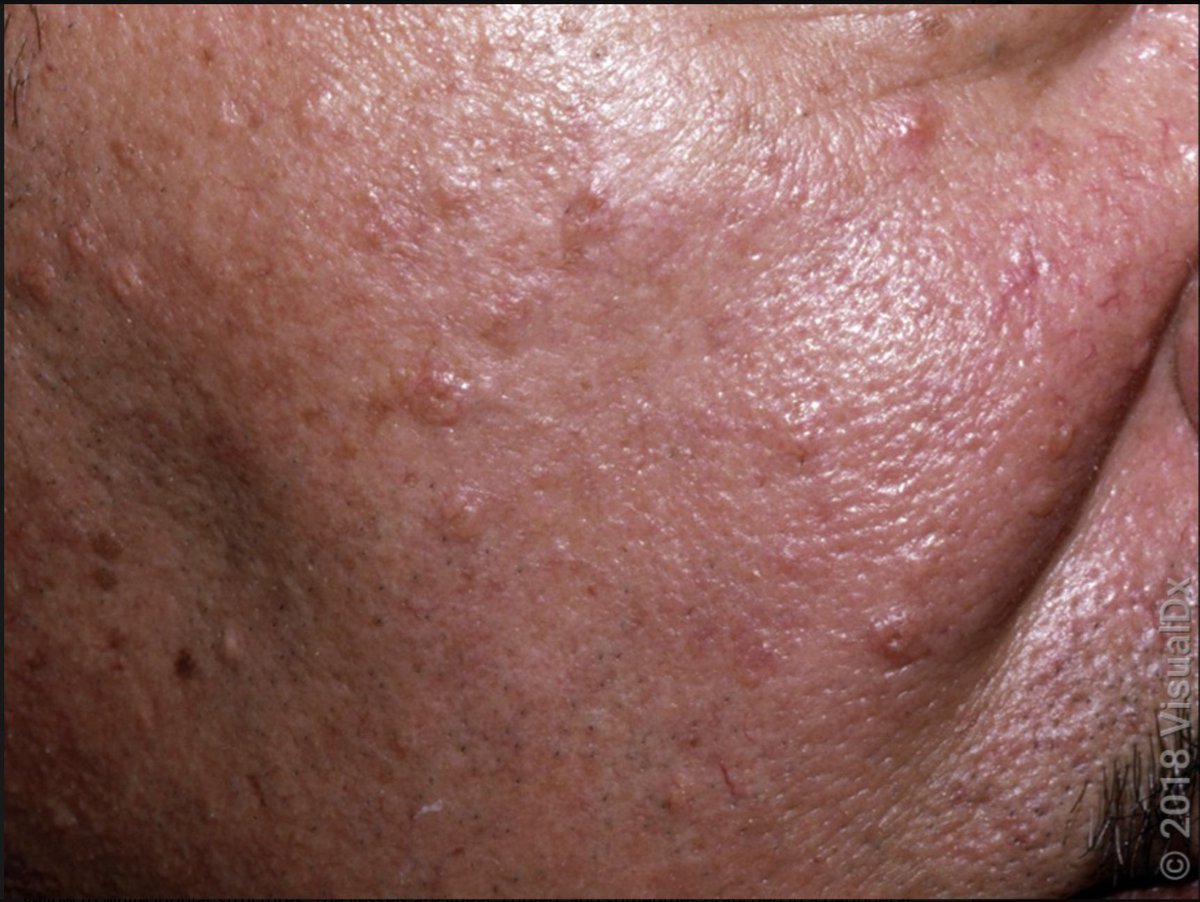
The proposed mechanism of action would lead one to think you'd see retiform purpura, but that really doesn't seem to be the case. Case reports (and cases I've seen in person) have been a variety of morphologies, often oval ulcerations.
PC: aad.org/dw/dw-insights…
8/
PC: aad.org/dw/dw-insights…
8/

Importantly, a biopsy of the skin is not particularly helpful to diagnose a Xylazine induced skin ulceration. Rather, the role of skin biopsy is to evaluate for other possible diagnoses on the differential, things like pyoderma gangrenosum, calciphylaxis, etc.
9/
9/
These wounds often get superinfected and can serve as a portal of entry for a deeper infections as well. Good wound care, potential antibiosis if an infection is suspected, would all be part of the care of patients with these skin findings.
PC:shmabstracts.org/abstract/a-cas…
10/
PC:shmabstracts.org/abstract/a-cas…
10/

SUMMARY
✅Skin ulceration has commonly been seen from Xylazine; the mechanism is unclear & likely multifactorial.
✅Morphology of the ulceration is nonspecific.
✅Biopsy doesn't help diagnose, history is more helpful.
✅Superinfection is common; good wound care is necessary.
11/
✅Skin ulceration has commonly been seen from Xylazine; the mechanism is unclear & likely multifactorial.
✅Morphology of the ulceration is nonspecific.
✅Biopsy doesn't help diagnose, history is more helpful.
✅Superinfection is common; good wound care is necessary.
11/
Thanks for joining! As you can see from the attention this is getting, it's something we're likely to see more of. I'm hoping we'll learn more and refine our ability to diagnose and treat over time!
Also tagging the amazing @DrSarahAxelrath in case I got anything wrong!
12/12
Also tagging the amazing @DrSarahAxelrath in case I got anything wrong!
12/12
• • •
Missing some Tweet in this thread? You can try to
force a refresh

 Read on Twitter
Read on Twitter