Critical Care-related tweets, from the CHEST perspective.
See you at #CHEST2023! #CHESTCritCare
How to get URL link on X (Twitter) App


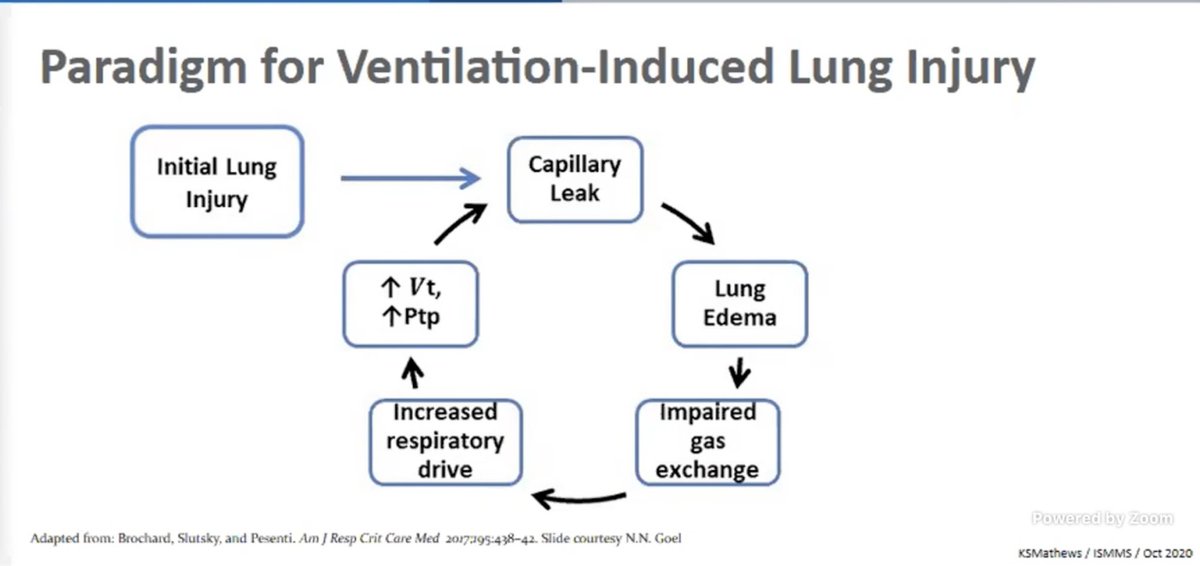
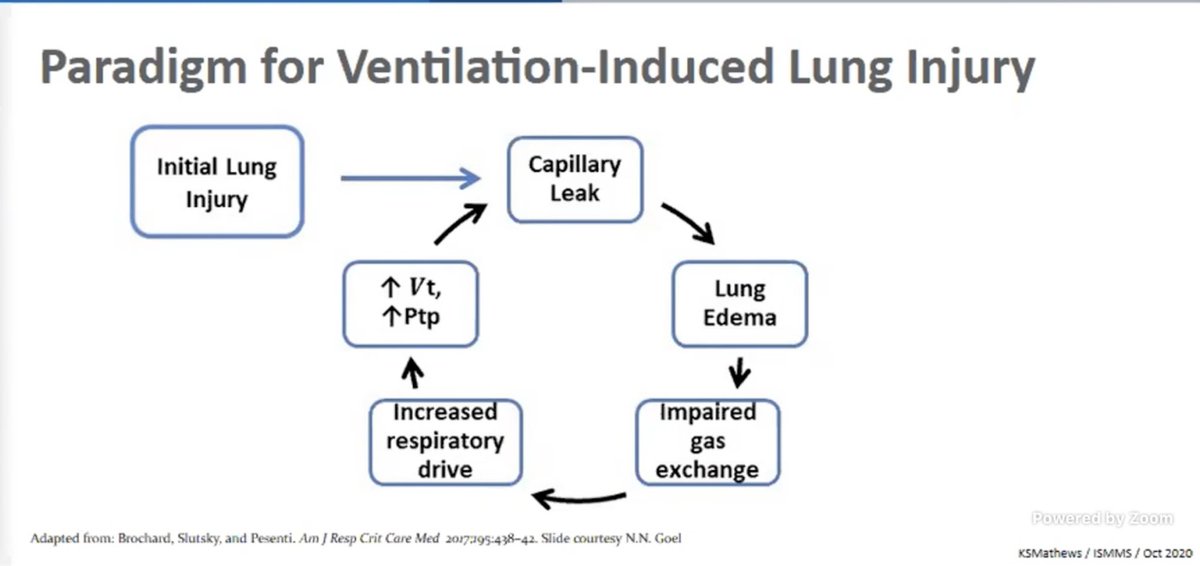
https://twitter.com/virenkaul/status/1318992846582652929Dr. Mathews: Starts with sharing what drives ventilation-induced lung injury. This is "leak" is likely more pronounced in #COVID19

 Up first is Dr. Angel Coz
Up first is Dr. Angel Coz 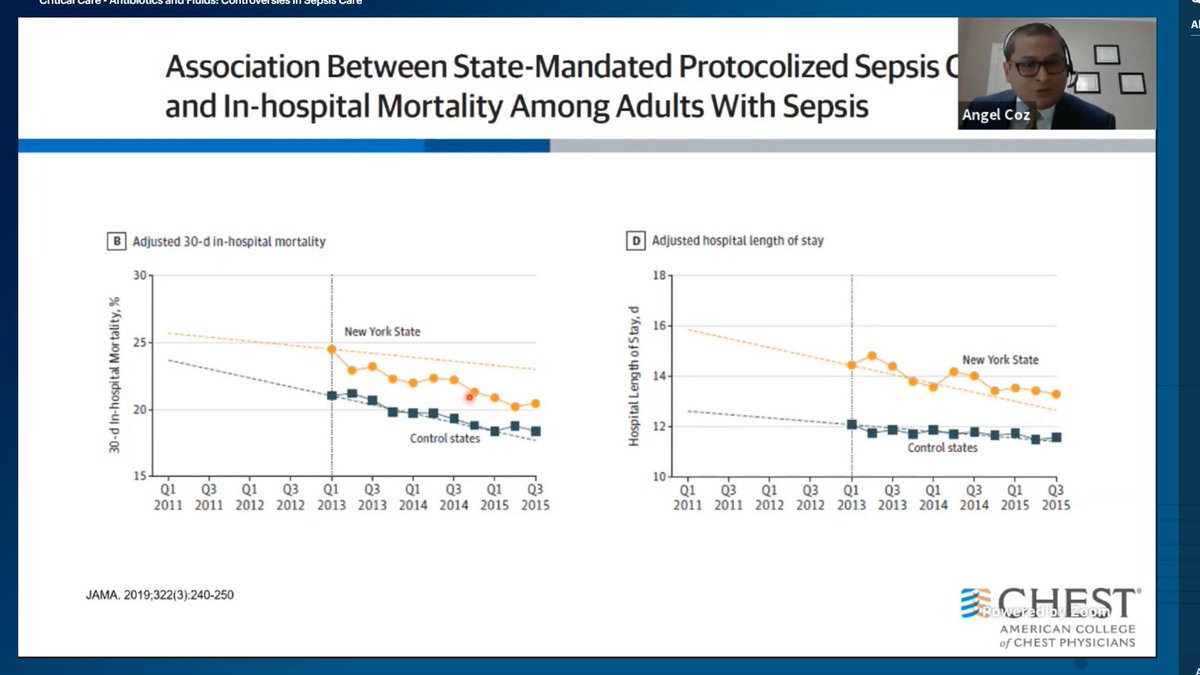



 Up first, Dr. Matthew Churpek discussing machine learning and big data.
Up first, Dr. Matthew Churpek discussing machine learning and big data.

https://twitter.com/virenkaul/status/1318204130167488512.@J_Mendelson_MD: HFNC and proning in severe hypoxic resp failure:


 Vitamin B12 up first by Dr. Jayshil Patel.
Vitamin B12 up first by Dr. Jayshil Patel.

 Here are the competitors:
Here are the competitors:

 @mnarasimhan highlights that as we know more about the natural course of COVID-19 we have seen that #PPE works! Also, that we should try non-invasive ventilation in COVID-19 patients as long as we have appropriate PPE #CHEST2020 #CHESTCritCare
@mnarasimhan highlights that as we know more about the natural course of COVID-19 we have seen that #PPE works! Also, that we should try non-invasive ventilation in COVID-19 patients as long as we have appropriate PPE #CHEST2020 #CHESTCritCare