
Microbiologist at @polybioRF: studying how persistent pathogens drive inflammaging, mitochondrial dysfunction & cognitive decline #longcovid #lyme #alzheimers
27 subscribers
How to get URL link on X (Twitter) App


 2/ The work was done by the same Harvard team who previously showed that the amyloid "plaque" in the Alzheimer's brain also forms in response to viral, bacterial, or fungal infections:
2/ The work was done by the same Harvard team who previously showed that the amyloid "plaque" in the Alzheimer's brain also forms in response to viral, bacterial, or fungal infections:

 2/ Specifically, viruses such as the herpesviruses, as well as intracellular bacteria & parasites—express proteins and metabolites capable of interfering with host immune signaling, #mitochondrial function, gene expression, and the #epigenetic environment.
2/ Specifically, viruses such as the herpesviruses, as well as intracellular bacteria & parasites—express proteins and metabolites capable of interfering with host immune signaling, #mitochondrial function, gene expression, and the #epigenetic environment. 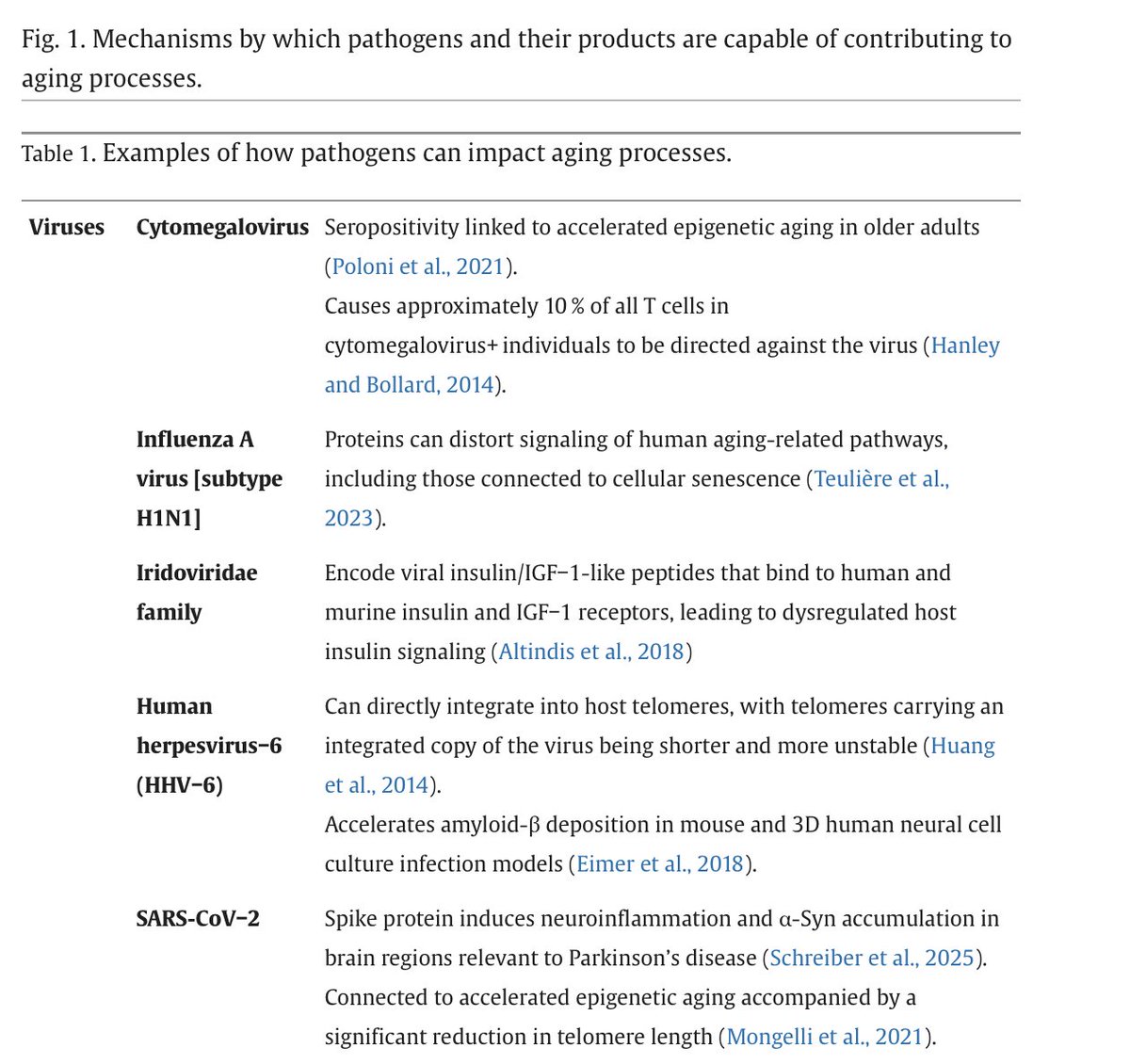

https://twitter.com/davidasinclair/status/19425896263943048432/ Consider for example this study. The team identified dozens of viral proteins that distort human pathway signaling controlling #aging-associated processes such as senescence and apoptosis: pubmed.ncbi.nlm.nih.gov/36649176/

https://twitter.com/SolidEvidence/status/19310156858465693872/ Because the viruses are being identified in wastewater it's possible that some viruses are harbored by animals - for example cattle or birds - whose feces end up in the wastewater

https://twitter.com/microbeminded2/status/17774827565342438272/ The viral proteins were found in participant blood. Where did they come from? As described in our paper below, it’s possible that at least some of the proteins “leak” into blood from persistent reservoirs of SARS-CoV-2 in tissue (gut, lungs etc): pubmed.ncbi.nlm.nih.gov/37667052/

https://twitter.com/r_prior/status/17474181034603316912/ We have formed a global #Consortium to study SARS-CoV-2 persistence: to determine if reservoirs of the #virus in LongCOVID tissue can drive widespread dysfunction including clotting, #microbiome, and neuroimmune abnormalities: polybio.org/longcovid
https://twitter.com/loscharlos/status/17303754409495143702/ Pathogens harbored by a patient at the time of SARS-CoV-2 #infection may serve as a predisposing factor to either persistence of the virus or increased disease in the acute phase
https://twitter.com/VitalikButerin/status/17292518567808291442/ To advance this movement in which novel tools to study & contain airborne #pathogens are actively being built, one must reject the narrative that there are only two paths forward 1) To 'care' abt airborne #infection means lockdowns 2) Freedom means ignoring airborne infection

 2/ Specifically, they found that neuroPASC patients exhibited attenuated systemic antibody responses against #SARS-CoV-2, characterized by decreased capacity to activate antibody-dependent complement deposition, NK cell activation + to bind Fcγ receptors
2/ Specifically, they found that neuroPASC patients exhibited attenuated systemic antibody responses against #SARS-CoV-2, characterized by decreased capacity to activate antibody-dependent complement deposition, NK cell activation + to bind Fcγ receptors




https://twitter.com/Quicktake/status/16310378809309061132/ No one knows whether the coronavirus or its remnants remain in everyone who’s had Covid, or if it’s just a group of patients, said Timothy Henrich, an associate professor of medicine at the University of California, San Francisco.