Hi #MedTwitter, let's talk about the workup of polycythemia and making a diagnosis of polycythemia vera (PV) vs. secondary polycythemia! #mpnsm #tweetorial @MedTweetorials
Based on the WHO guidelines, the following values constitute polycythemia:
In men: Hgb >16.5g/dL or Hct > 49%
In women: Hgb > 16 or Hct > 48%
Polycythemia should be confirmed by a subsequent CBC. Below is an image of the ddx of polycythemia (Keohane et al 2013)
In men: Hgb >16.5g/dL or Hct > 49%
In women: Hgb > 16 or Hct > 48%
Polycythemia should be confirmed by a subsequent CBC. Below is an image of the ddx of polycythemia (Keohane et al 2013)

Our patient's polycythemia has been confirmed! What to do next? Make sure to ask questions related to hyperviscosity (eg chest pain, dyspnea, headache, vision changes, confusion), thrombosis/bleeding hx, and PV-related symptoms (pruritus after baths, erythromelalgia, B-symptoms)
Other important history tidbits to review: smoking/tobacco history, chronic cardiopulmonary disease, OSA hx, potential carbon monoxide exposure, performance enhancing drugs/supplements, signs/symptoms concerning for malignancy
What do we look for on exam: evidence of cyanosis, cardiovascular findings concerning for a shunt, facial plethora or ruddiness, hepatosplenomegaly, and check a pulse ox on room air
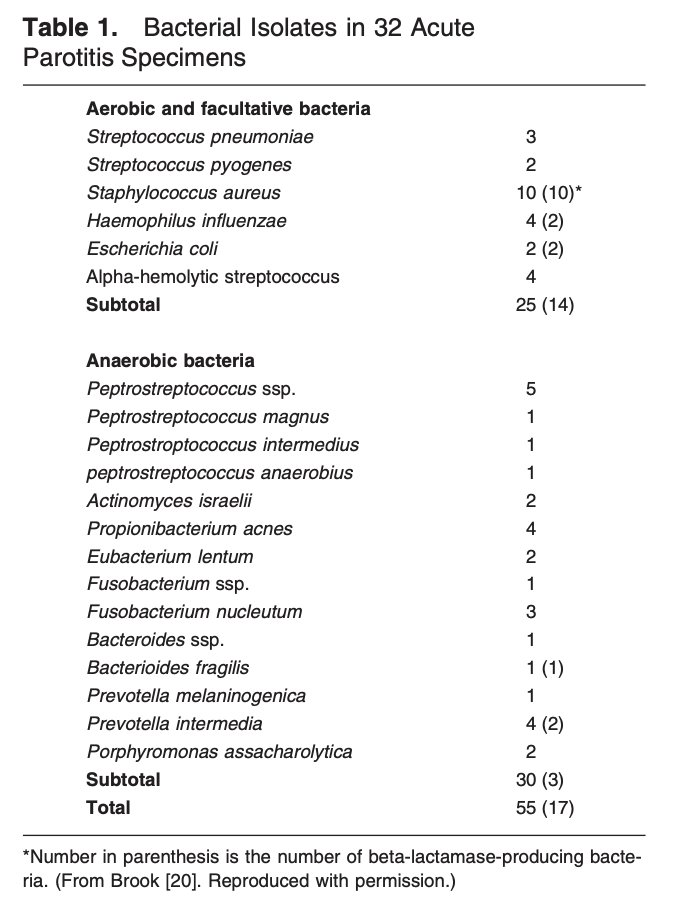
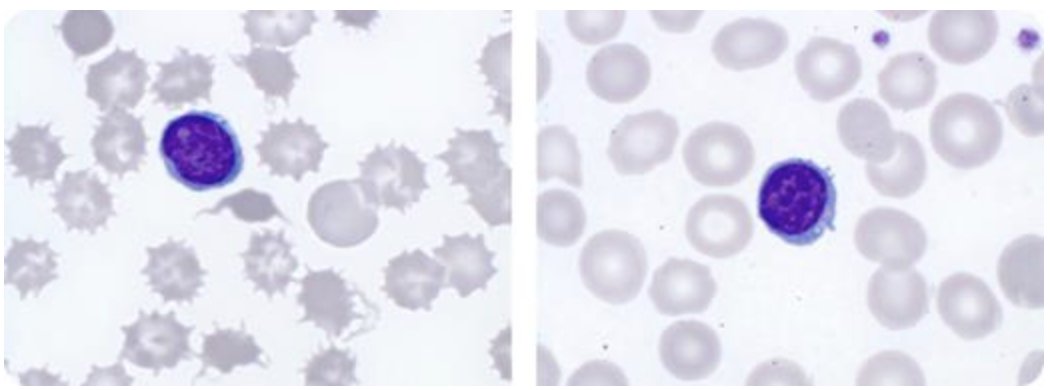
Initial labs typically include CBC w/ diff, peripheral smear, and CMP. Urinalysis can be considered if history, exam, and labs are concerning for a possible renal etiology. Erythropoietin (EPO) level should be sent off. Below is an image re the presentation of PV (Spivak 2019) 

If EPO is low-low/normal, JAK2 V617F mutational testing should be sent. If JAK2 V617F is negative but suspicion for an MPN is high, testing for other JAK2 mutations, CALR mutations, MPL mutations, & BCR-ABL is considered. Below are the WHO diagnostic criteria for PV 

One important point to make is that JAK2 mutations can be seen quite frequently in MPNs other than PV. Both primary myelofibrosis and essential thrombocytosis have JAK2-mutation frequencies of >50%. Bone marrow biopsy may be necessary to differentiate PV from other MPNs
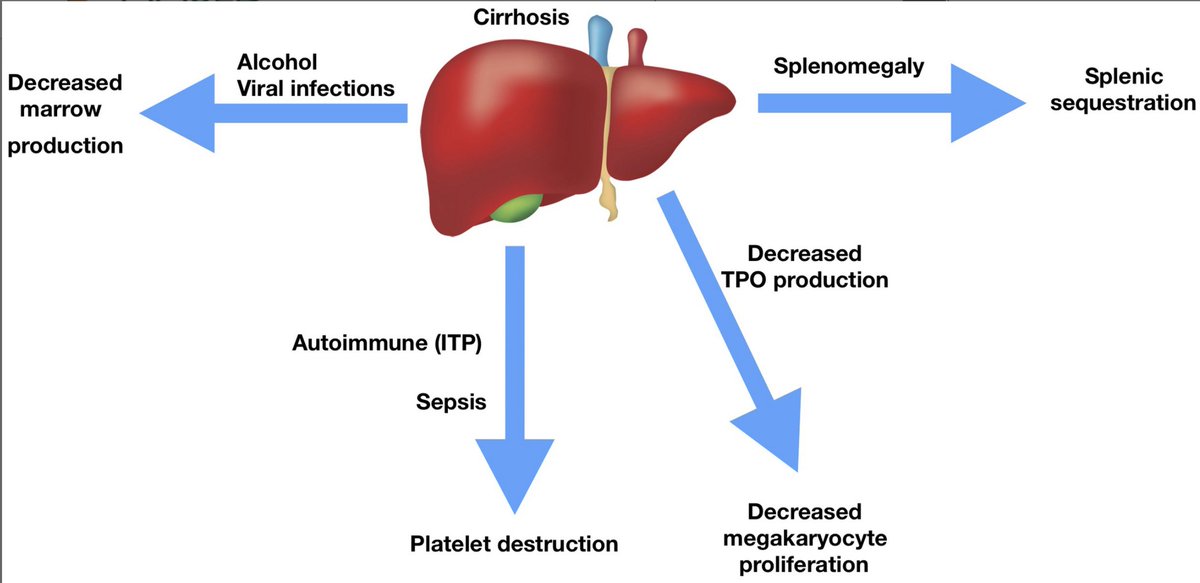
If EPO is high-normal/high then secondary polycythemia is likely! Directed workup based on the underlying driver should be pursued such as underlying cardiopulmonary disease, carbon monoxide exposure, renal disease, exogenous EPO, or EPO-secreting tumor.
Hopefully this has been helpful! Any feedback or additional thoughts from #medtwitter is welcome! @CPSolvers @Vikas_Gupta_1
@CPSolvers @Vikas_Gupta_1 This diagnostic approach can be put to use on an @hdx case from this week!
• • •
Missing some Tweet in this thread? You can try to
force a refresh