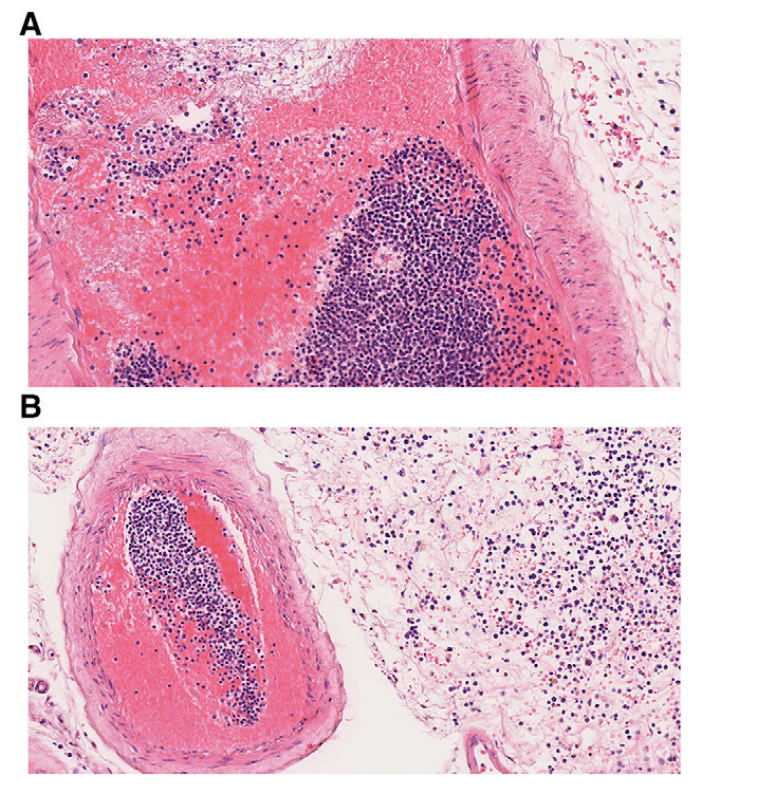
- Risk of leukostasis is higher in AML compared to ALL due to higher MCV and expression of adhesion molecules
-A dx of leukostasis requires hyperleukocytosis + clinical findings
- Initial management includes IV fluids and cytoreduction. Leukapheresis is controversial