Saw a patient in clinic w/ (likely) refractory ITP and luckily there was an excellent @BloodJournal article by Miltiadous and colleagues published earlier this month! I want to highlight some of the main learning points I took away #medtwitter #hemetwitter ashpublications.org/blood/article/…
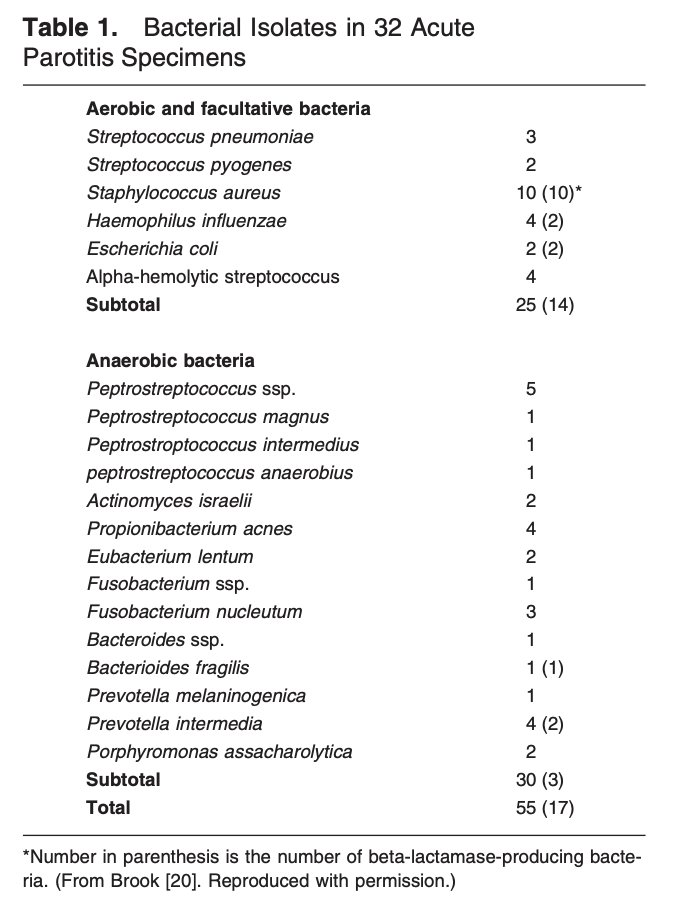
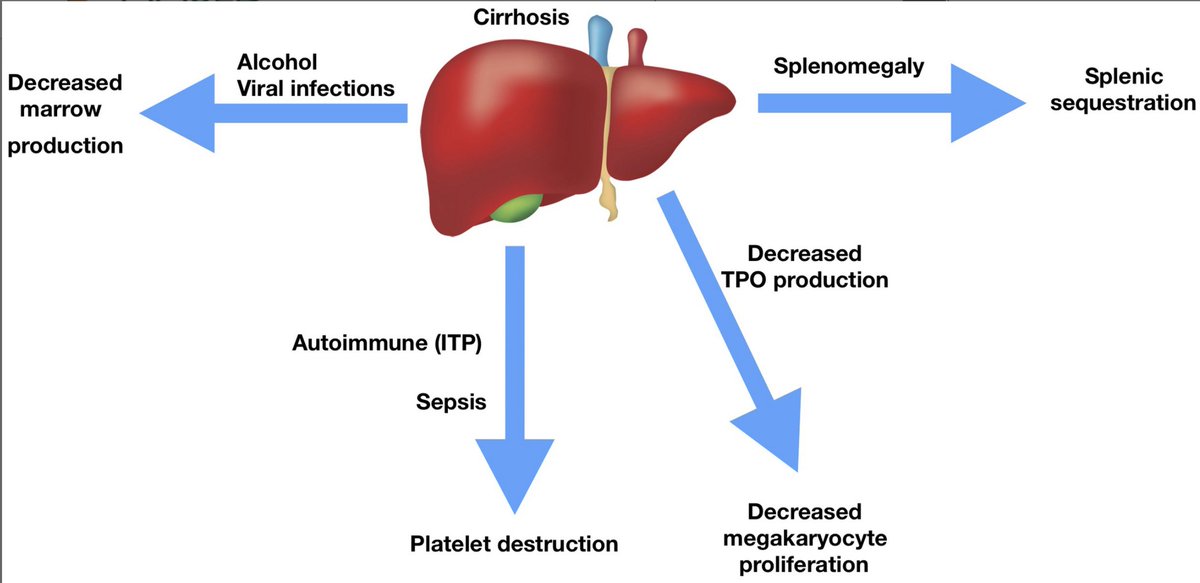
# 1: Make sure that the patient truly has primary, refractory ITP! If a patient is not responding as expected with primary ITP-directed therapies, it bears consideration to do a more extensive workup looking for alternative diagnoses 



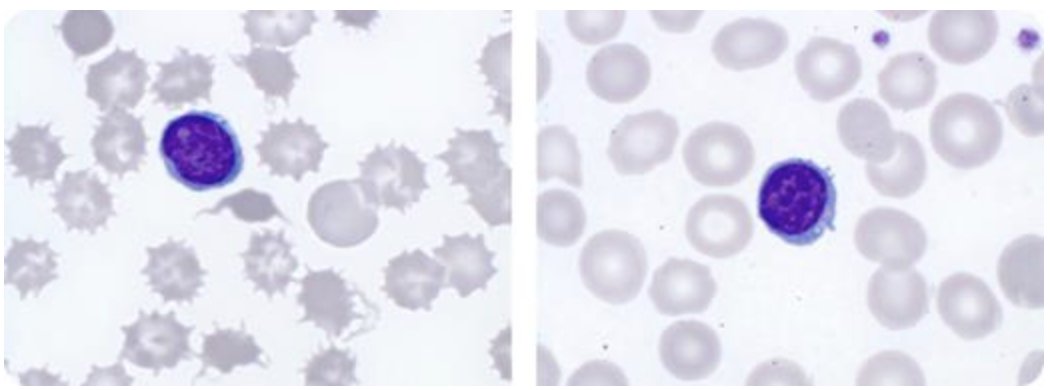
#2: If a patient is not responding as expected to treatment for ITP, have a low threshold to pursue a bone marrow biopsy. A number of bone marrow failure states can present with isolated thrombocytopenia 

#3: If a patient truly has refractory, primary ITP then combination therapies should be considered. The flowchart nicely outlines workup and treatments, the evidence behind different combinations is covered in the article itself 
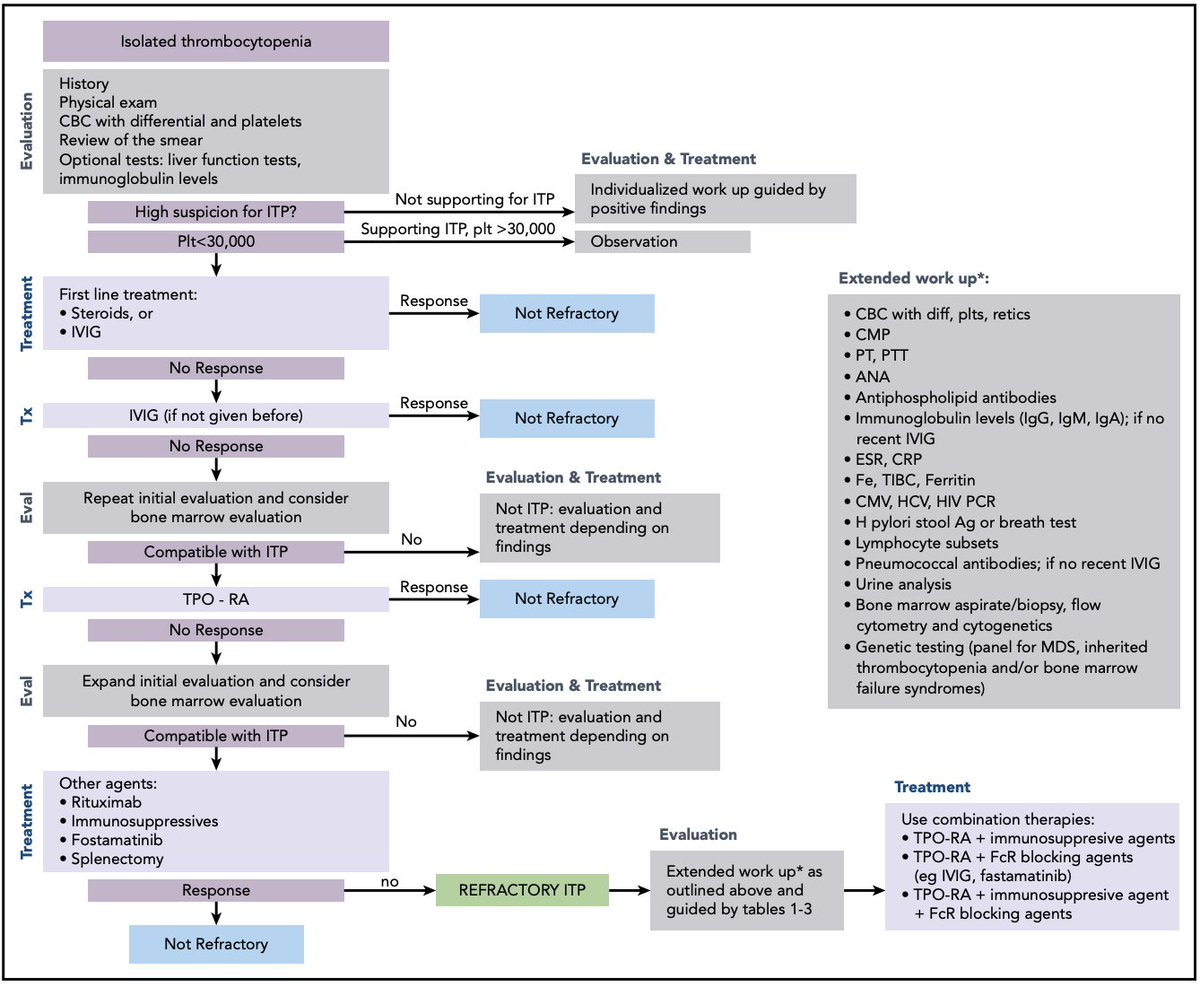
In summary, the more ITP I see the more I realize how many patients may not have it. Therefore I have a low threshold to pursue additional workup and re-examine the original dx if patients aren't responding as expected. Would love to get additional pearls from #medtwitter
• • •
Missing some Tweet in this thread? You can try to
force a refresh