Today I would like to read and tweet about non-#covid things
Will start a string of pearls and 🔥🌶takes from recent papers #livertwitter #gitwitter #cirrhosis
Will start a string of pearls and 🔥🌶takes from recent papers #livertwitter #gitwitter #cirrhosis
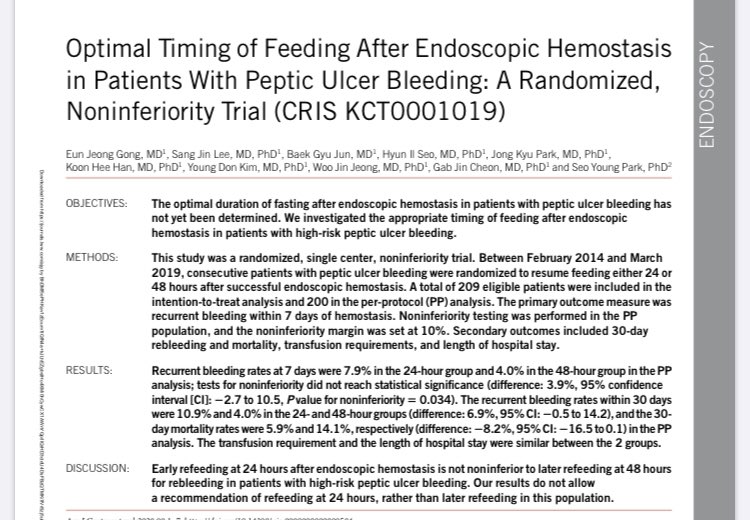
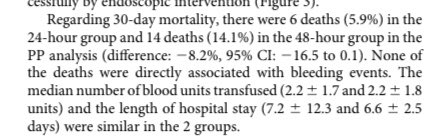
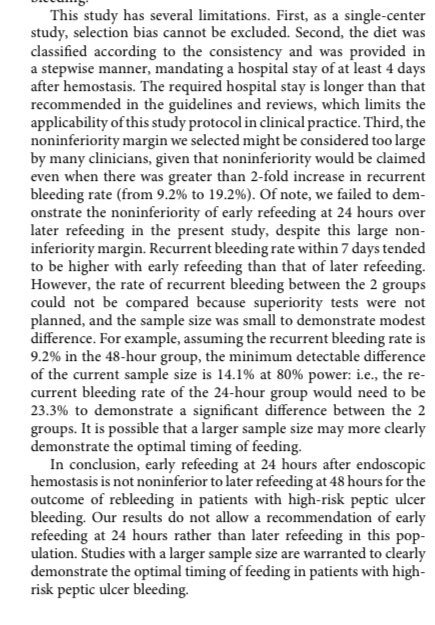
This paper in #amjgastro compared refeeding @ 24 v48 hrs after endoscopic interventions for peptic ulcers. 24 hours was “not noninferior”. multiple limits
1️⃣ ⬆️mortality in 48h
2️⃣diff duration of iv ppi
My 🌶🌶 take: feed your patients when they want!



1️⃣ ⬆️mortality in 48h
2️⃣diff duration of iv ppi
My 🌶🌶 take: feed your patients when they want!

This @LiverInt multinational study shows that noninvasive tests help sort high from low risk for liver-related events and, to a degree, ❤️events in #nafld
🌶take: this is how we need to do #nafld epi from now on

🌶take: this is how we need to do #nafld epi from now on


🛑the madness!
Biofire PCR tests 4 stool “infections” are positive in 14% of healthy controls (!!!) & offer limited to no prognostic information in ppl with #ibd
🌶🌶🌶take: These tests are out of control, riddled with false positives. Check cdiff &manage clinically. @ibddoctor

Biofire PCR tests 4 stool “infections” are positive in 14% of healthy controls (!!!) & offer limited to no prognostic information in ppl with #ibd
🌶🌶🌶take: These tests are out of control, riddled with false positives. Check cdiff &manage clinically. @ibddoctor


PEARL ALERT:
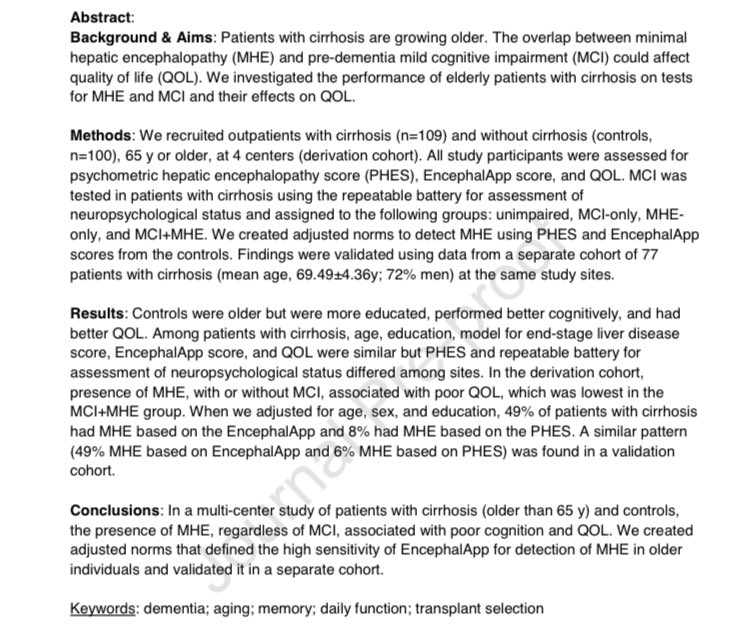
Memory is preserved in Minimal hepatic encephalopathy
WHY THIS @AGA_CGH PAPER MATTERS:
As ppl w/#cirrhosis age, there is overlap between causes of cognitive dysfunction
WHAT @JasmohanBajaj DID
1️⃣mHE matters even when MCI present
2️⃣norms for older persons


Memory is preserved in Minimal hepatic encephalopathy
WHY THIS @AGA_CGH PAPER MATTERS:
As ppl w/#cirrhosis age, there is overlap between causes of cognitive dysfunction
WHAT @JasmohanBajaj DID
1️⃣mHE matters even when MCI present
2️⃣norms for older persons


TPOag ⬆️platelets in #cirrhosis
Do we need them before procedures?
WHY I LIKED THIS @AGA_CGH PAPER
1️⃣mainly before HCC treatment. 🌶: shouldn’t be used before egd
WHAT COULD BE BETTER
1️⃣weird bleeding defn. No diff periop!
2️⃣🌶I wish the comparison was no plts!
PMID:32205226


Do we need them before procedures?
WHY I LIKED THIS @AGA_CGH PAPER
1️⃣mainly before HCC treatment. 🌶: shouldn’t be used before egd
WHAT COULD BE BETTER
1️⃣weird bleeding defn. No diff periop!
2️⃣🌶I wish the comparison was no plts!
PMID:32205226


“Have I told u FIB-4 rocks?” Vol 47
👉200000 people without known liver disease followed for 1.7million person-years in korean health exam database
👉high fib-4 = ⬆️⬆️mortality
Pmid: 32090451


👉200000 people without known liver disease followed for 1.7million person-years in korean health exam database
👉high fib-4 = ⬆️⬆️mortality
Pmid: 32090451



• • •
Missing some Tweet in this thread? You can try to
force a refresh













