mayoclinicproceedings.org/pb/assets/raw/… or
COVID-19 Testing: The Threat of False-Negative Results sciencedirect.com/science/articl… #EBM
@MayoProceedings Also note ja.ma/3ct4UPD from @marcottl @JoshuaLiaoMD
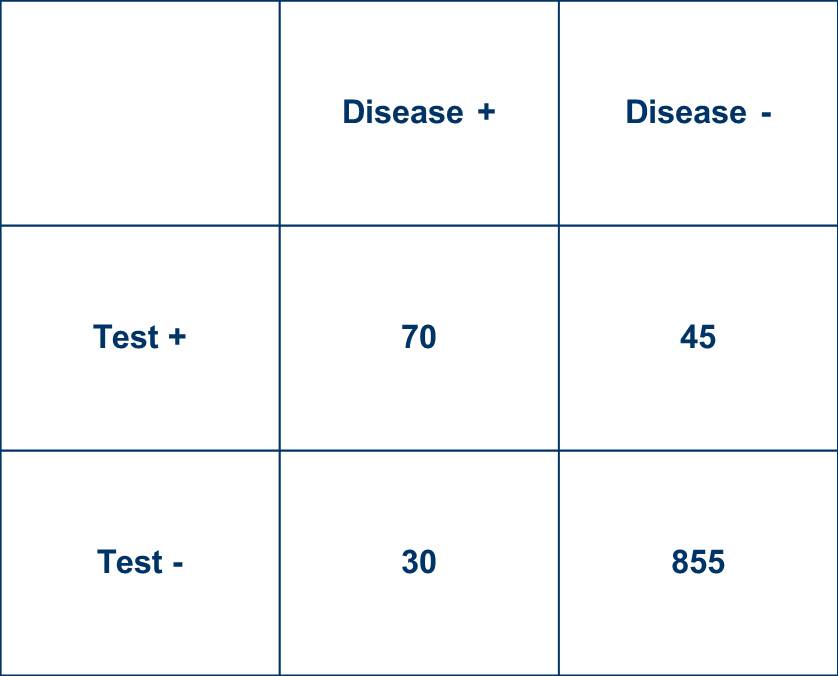
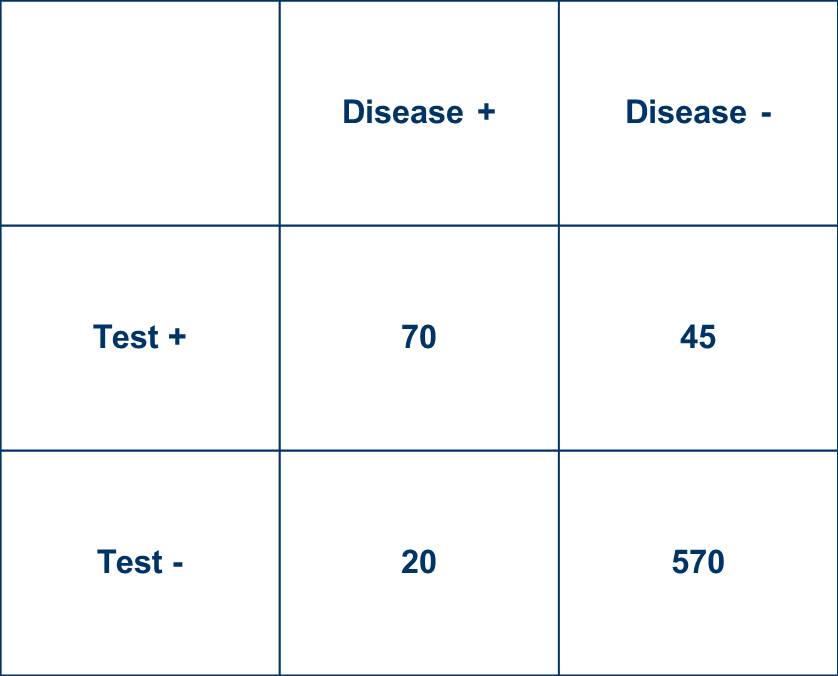
Sensitivity = 70%
Specificity = 95%
LR+ = 14
LR- = 0.32
These are not dissimilar to #COVID19 data floating around, although hardly universally agreed upon.