Question to all #VExUS experts: "Do you ever diurese VExUS 0 ?" Thread below.
I admit not being a #VExUS user, but learned much from your tweets and have been practicing many #DiuresisJedi concepts.
@ArgaizR @msiuba @ThinkingCC @NephroP @load_dependent @khaycock2 @Thind888
I admit not being a #VExUS user, but learned much from your tweets and have been practicing many #DiuresisJedi concepts.
@ArgaizR @msiuba @ThinkingCC @NephroP @load_dependent @khaycock2 @Thind888
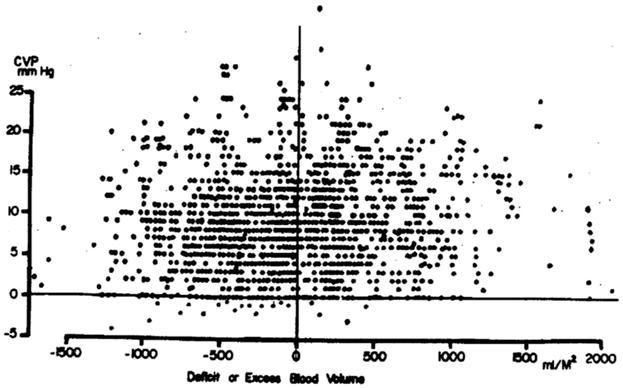
Ever since I read this great paper, tend to consider volume status and cardiac filling pressures as 2 separate and equally important concepts that both deserve optimisation in #ICU and #HeartFailure.
Basically, V-p correlation is all over the place! (1/6)
journal.chestnet.org/article/S0012-…
Basically, V-p correlation is all over the place! (1/6)
journal.chestnet.org/article/S0012-…
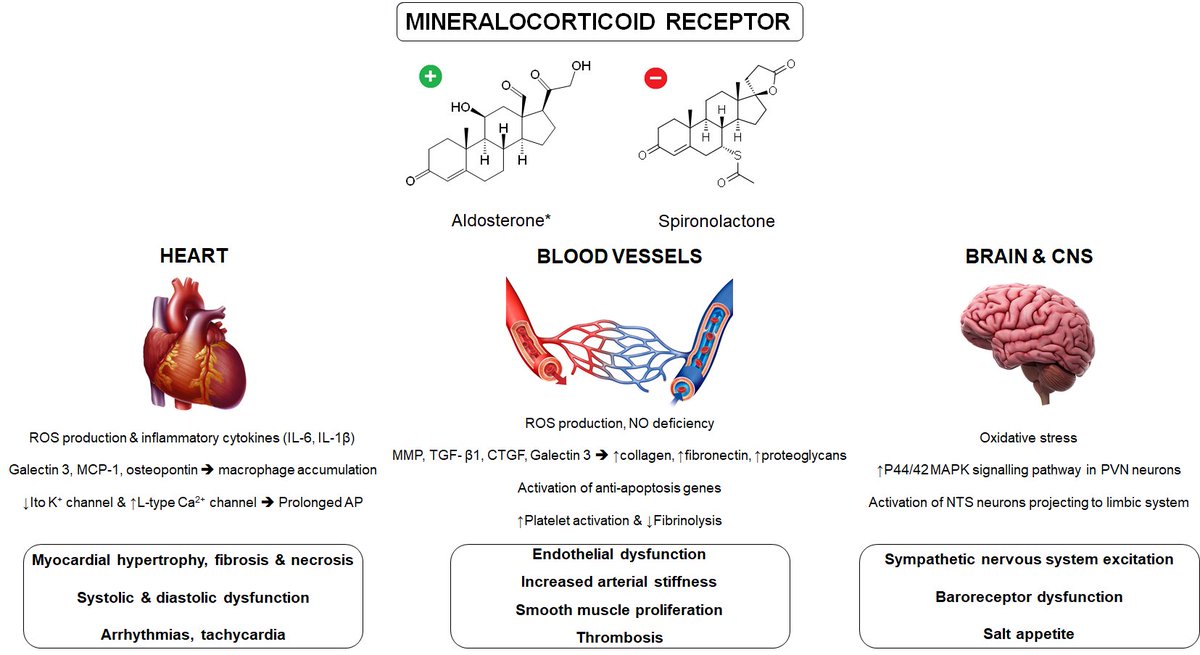
What I learned from you all is that #VExUS & especially portal vein flow is a great tool to assess the impact of ⬆️(right-sided) pressure on organ function. This gives you more confidence to diurese patients, even when hypotensive or still hemodynamic unstable. (2/6)
My approach has always been to try and operate at "the lowest comfortable volume or better NaCl status" in ICU (and HF) patients. Therefore, I tend to diurese from the moment I achieve hemodynamic stability. Urine Na concentration helps me to decide how far I can go. (3/6) 

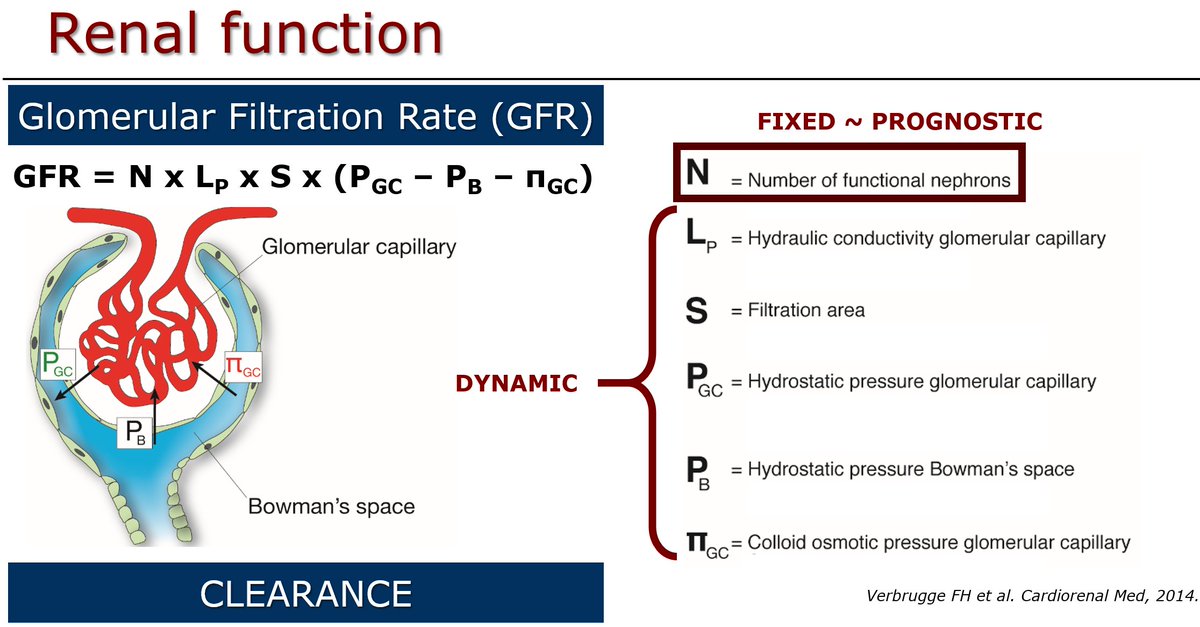
My diuretic cocktail is usually bolus acetazolamide+bumetanide (dose~GFR) for balanced diuresis & thiazides in case of diuretic resistance. I only stop to diurese after urine Na <85 mmol/L, which is often AFTER cardiac filling pressures normalize. (4/6)
link.springer.com/article/10.100…
link.springer.com/article/10.100…
Why? Cumulative NaCl overload very common in #ICU from crystalloid administration & intermittent loop diuretics producing hypotonic urine. NaCl determines ECV, is buffered in interstitium & harms the glycocalyx, so NaCl depletion makes sense! (5/6)
sciencedirect.com/science/articl…
sciencedirect.com/science/articl…

So this is what I do (below), which means I would consider (slow) diuresis even in patients with normal cardiac filling pressures (but high urinary Na response) that have presumably low #VExUS grade. Get rid of Na overload! Has served me well... Curious about your thoughts! (6/6) 

• • •
Missing some Tweet in this thread? You can try to
force a refresh