1/ Covid (@UCSF) Chronicles, Day 177
Nice to re-start our Covid grand rounds today. Available here: tinyurl.com/yyw5myns. We covered a range of epi issues (the shape of the pandemic, changing mortality rate of Covid) and highlighted a novel new therapeutic approach: AeroNabs.
Nice to re-start our Covid grand rounds today. Available here: tinyurl.com/yyw5myns. We covered a range of epi issues (the shape of the pandemic, changing mortality rate of Covid) and highlighted a novel new therapeutic approach: AeroNabs.
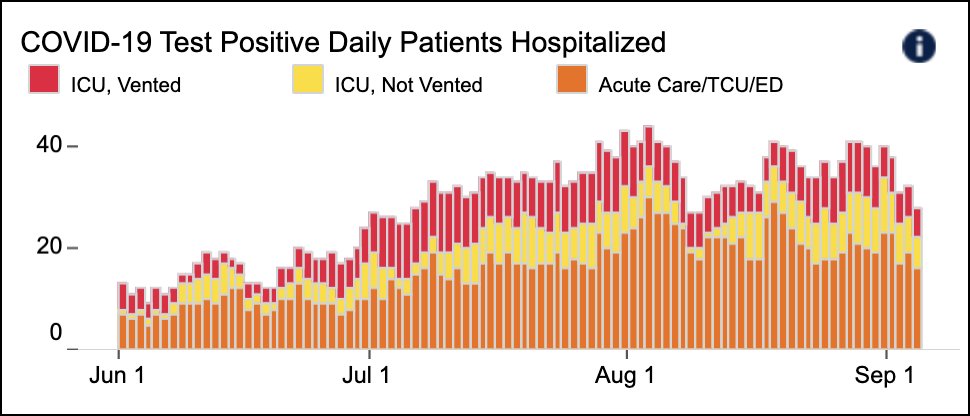
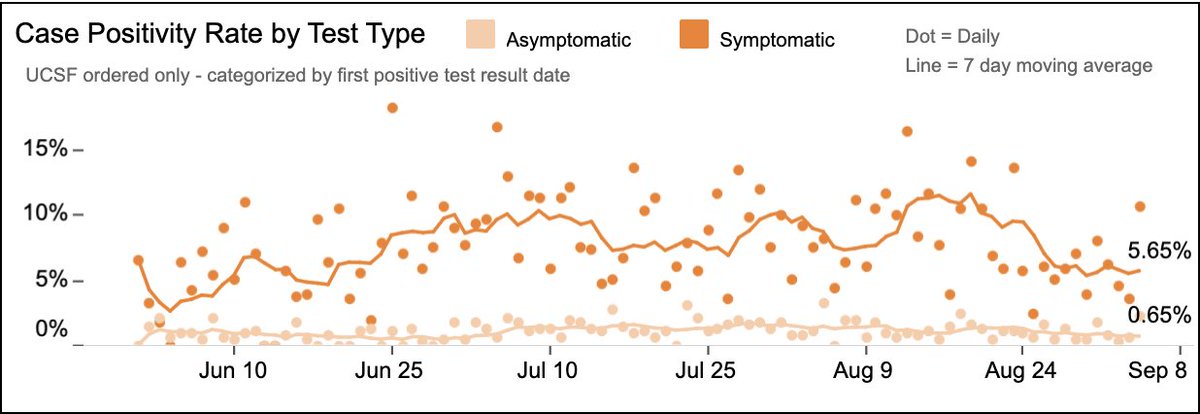
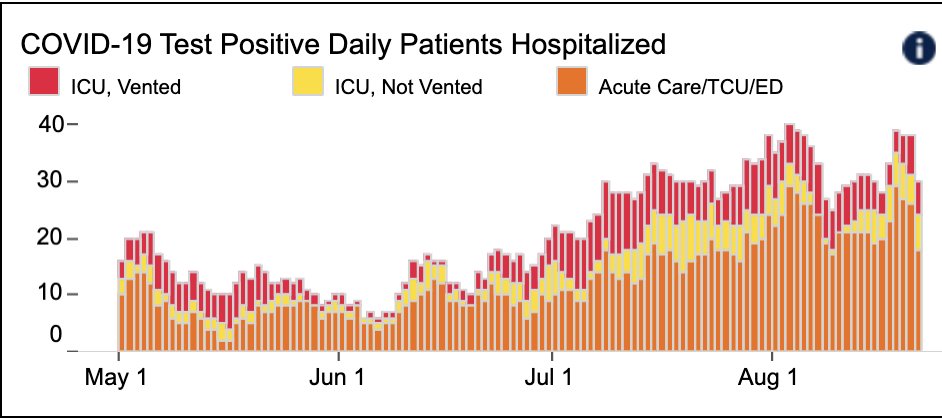
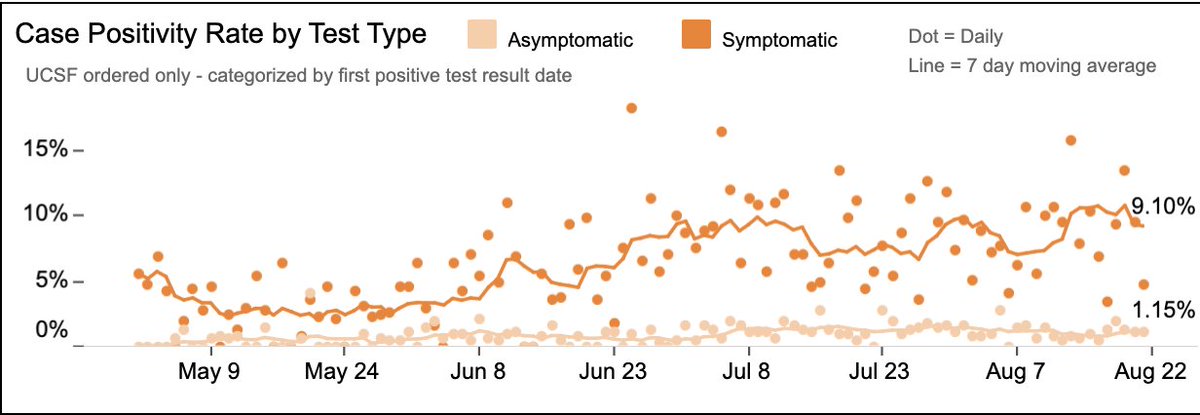
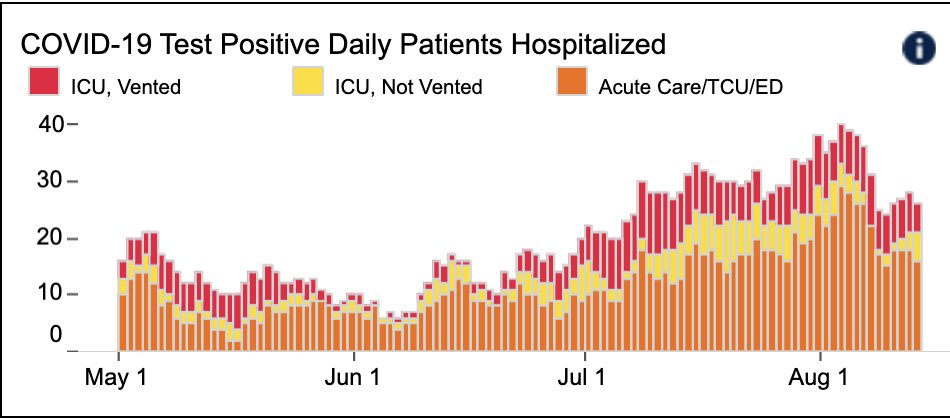
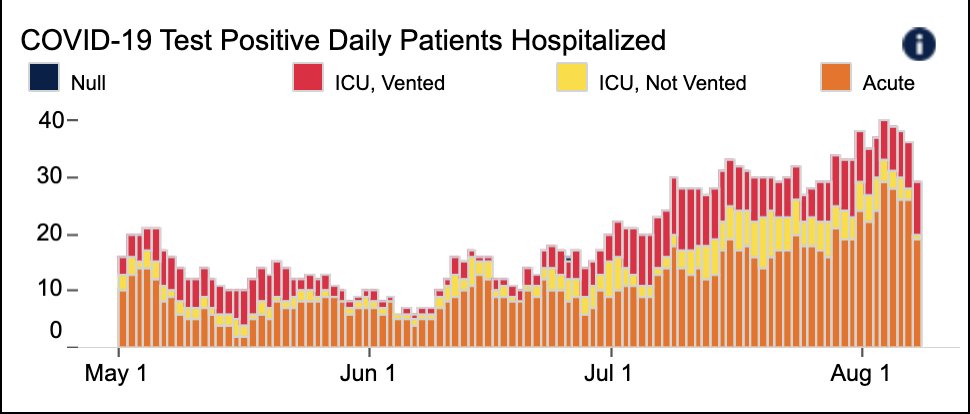
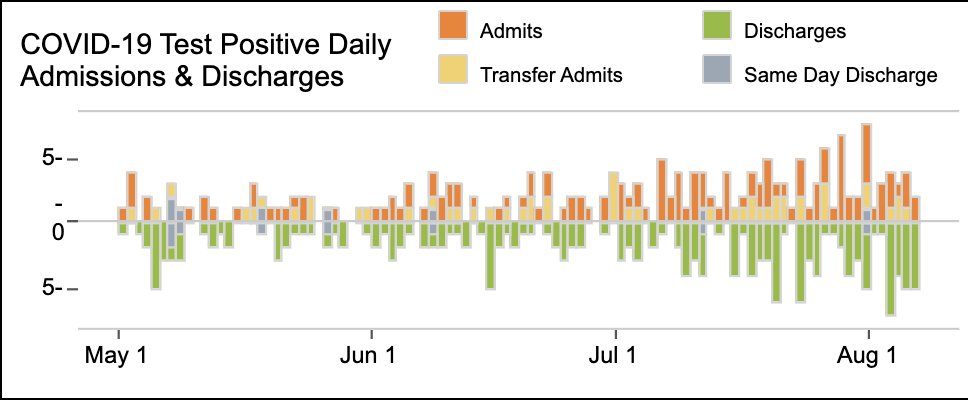
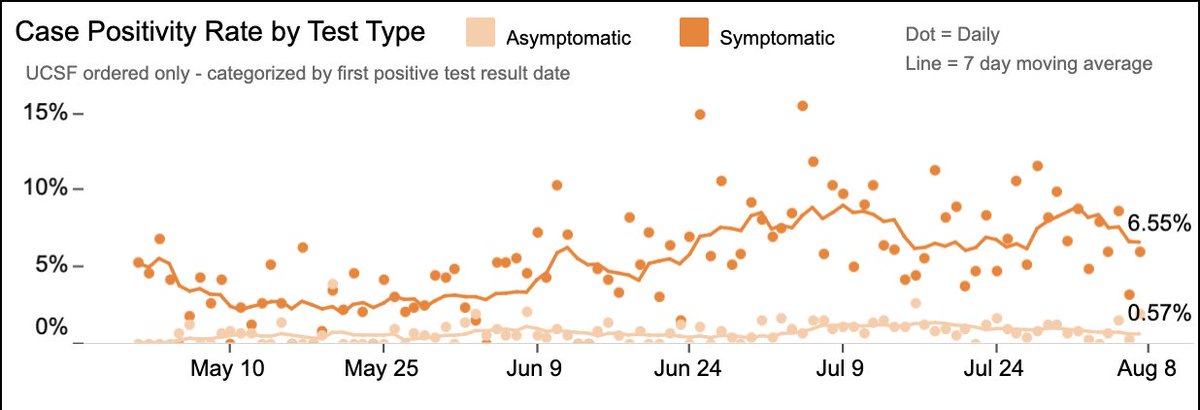
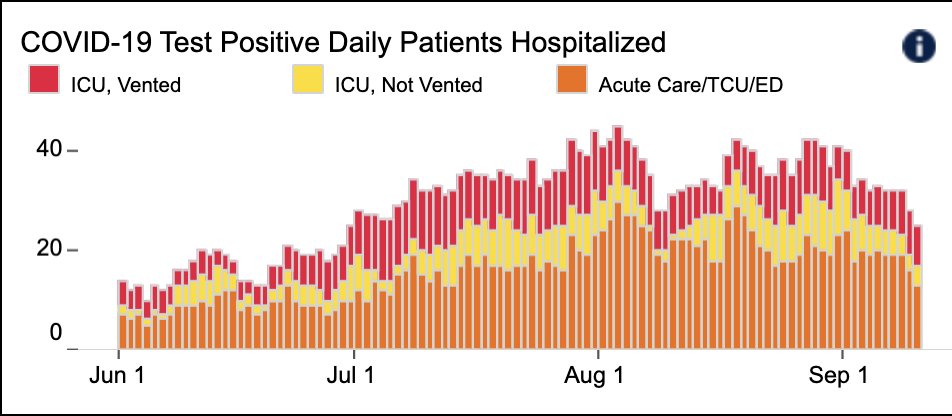
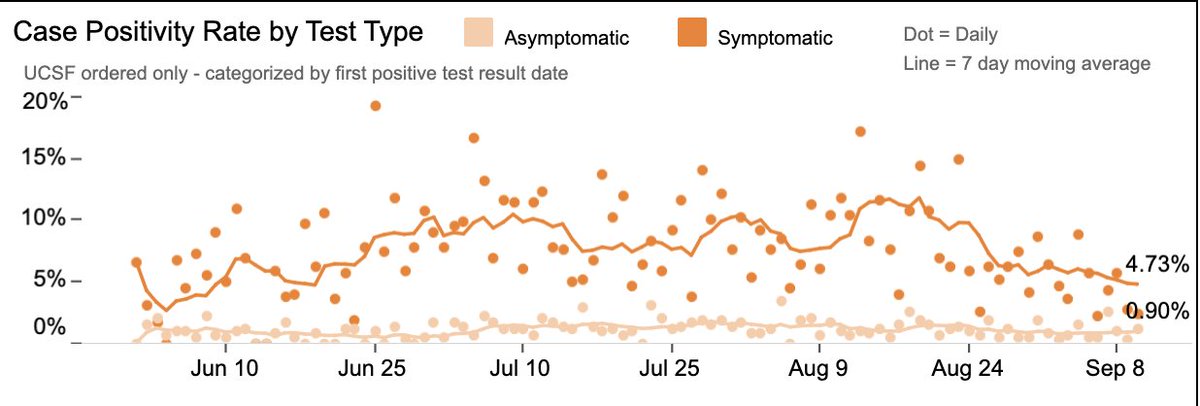
2/ @UCSFHospitals: continued good news, with fewer hospitalized pts (23, w/ 7 on vents), lowest since June (Fig on L). Test positivity 2.7%: 4.7% in pts w/ symptoms (down); 0.9% in pts w/o (a bit up) (Fig R). Sx/Asx ratio usually ~10:1; not sure what 5:1 ratio means. Prob a blip. 

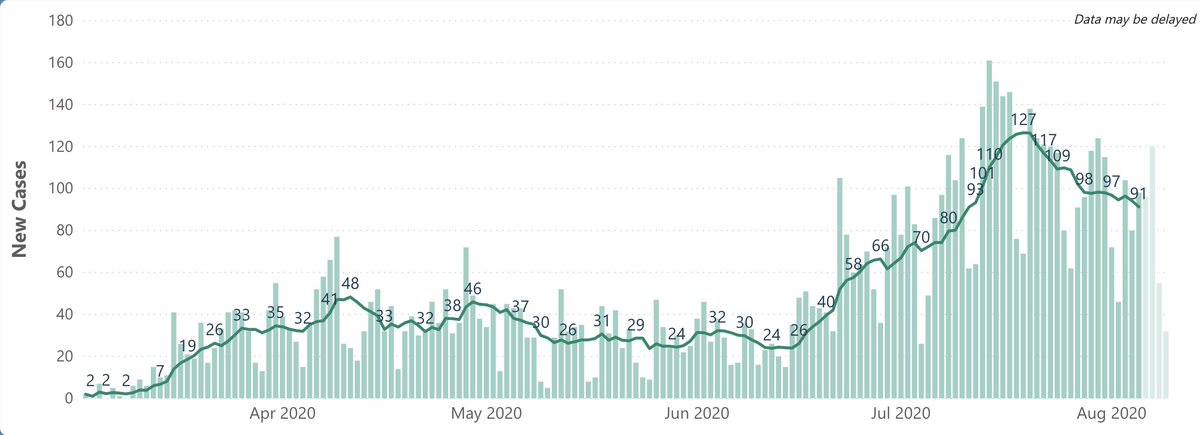
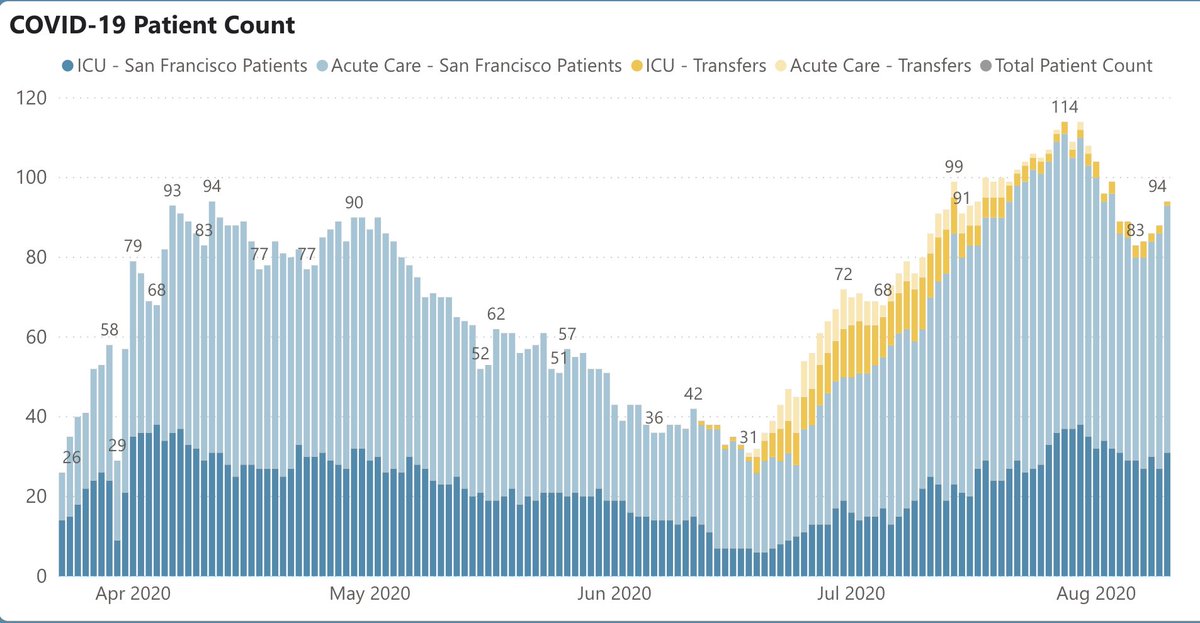
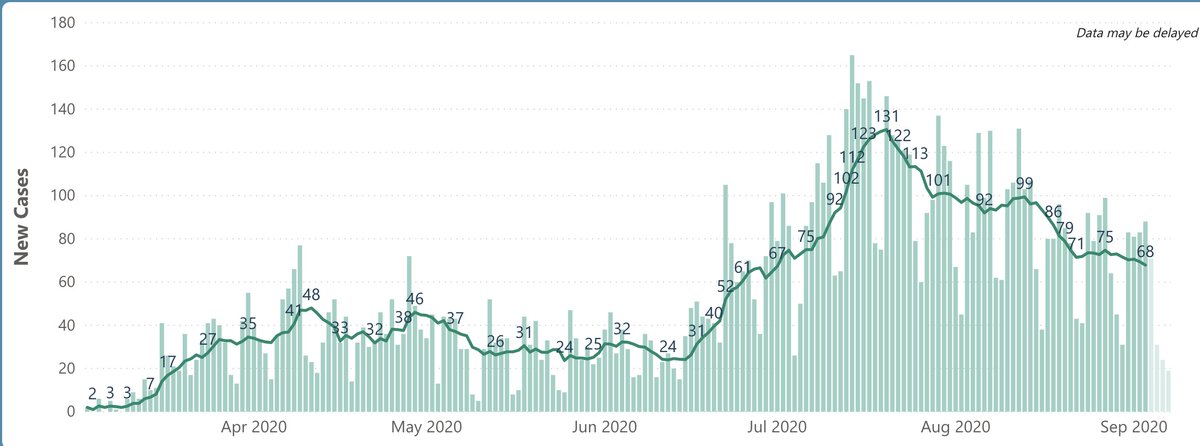
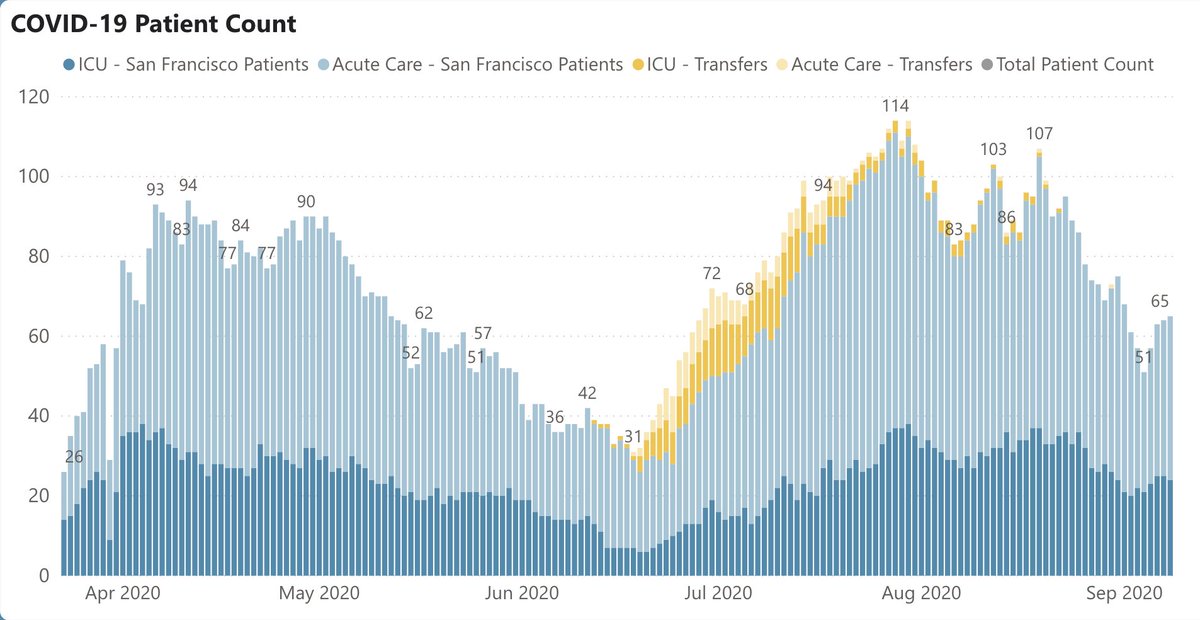
3/ SF: daily case rate down to 68, half of the peak in July (Fig on L). Total of 88 deaths since March; more on this amazing # later. SF case positivity rate 2.1%. SF hospitalizations also going in right direction: 65 total, also ~half of peak in July (Fig R). 

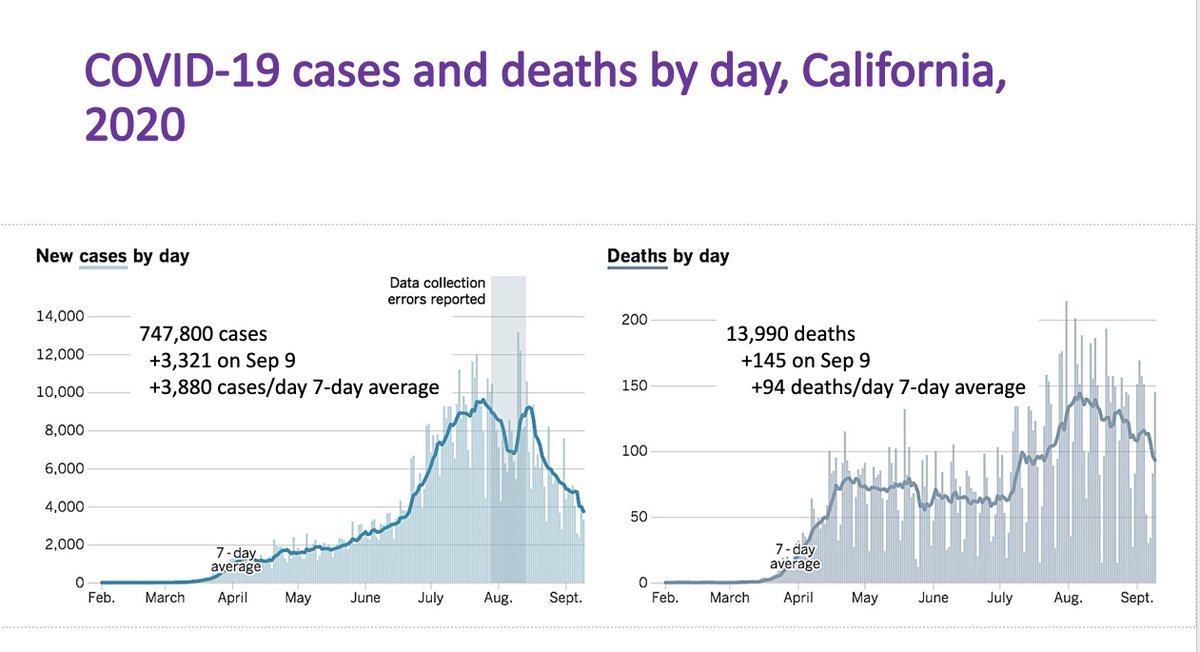
4/ On to Grand Rounds: @ 11:30, CA data (below) by @Rutherford_UCSF: daily cases down to ~4000 (vs peak of 10K). Deaths also down, now <100/day for first time since July. Along w/ southern states (TX, FL, AZ), CA is improving – a big part of reason why U.S. case rate is falling. 
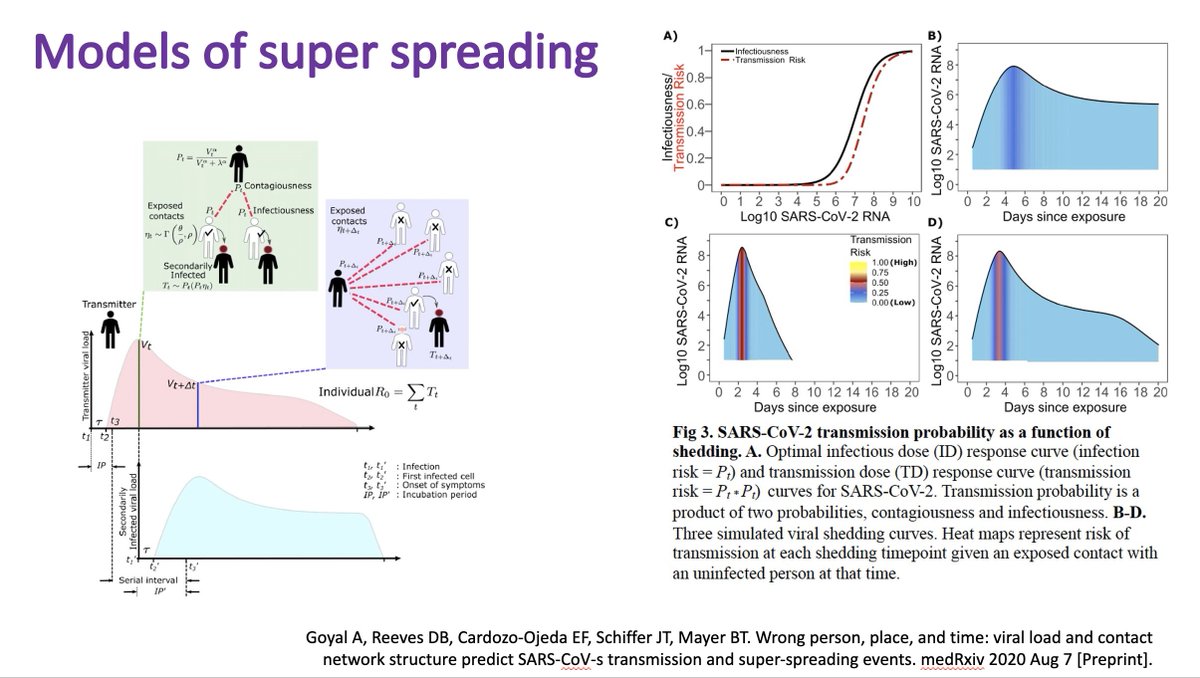
5/ @ 7:00, George reviewed the (somewhat controversial) study that found that Sturgis Motorcycle Rally was the nation’s biggest superspreader event ever. Early on, we had no idea of how superspreading happened: was it about viral load, or anatomy, ventilation, or something else? 

6/ @ 8:50, George reviews current thinking on how superspreading happens. Seems to be a combo of very infectious person happening to come in close contact with a crowd. “It’s just a matter of luck and timing." (Timing: days 4-6 after exposure is highest risk for spreading). 
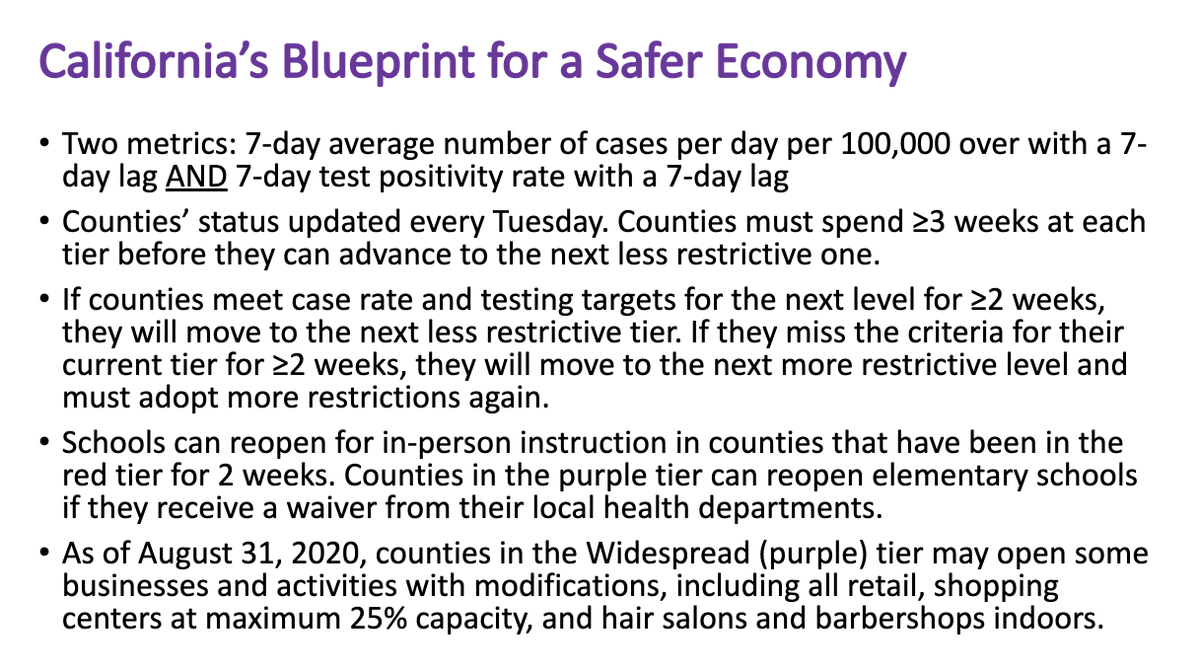
7/ @ 18:50, George reviewed CA’s new “Blueprint for a Safer Economy,” a more conservative plan for opening up the state. Summary below – key change is that the bar for counties to move toward more openness is higher, w/ need for 2 weeks of good performance before changing tiers. 
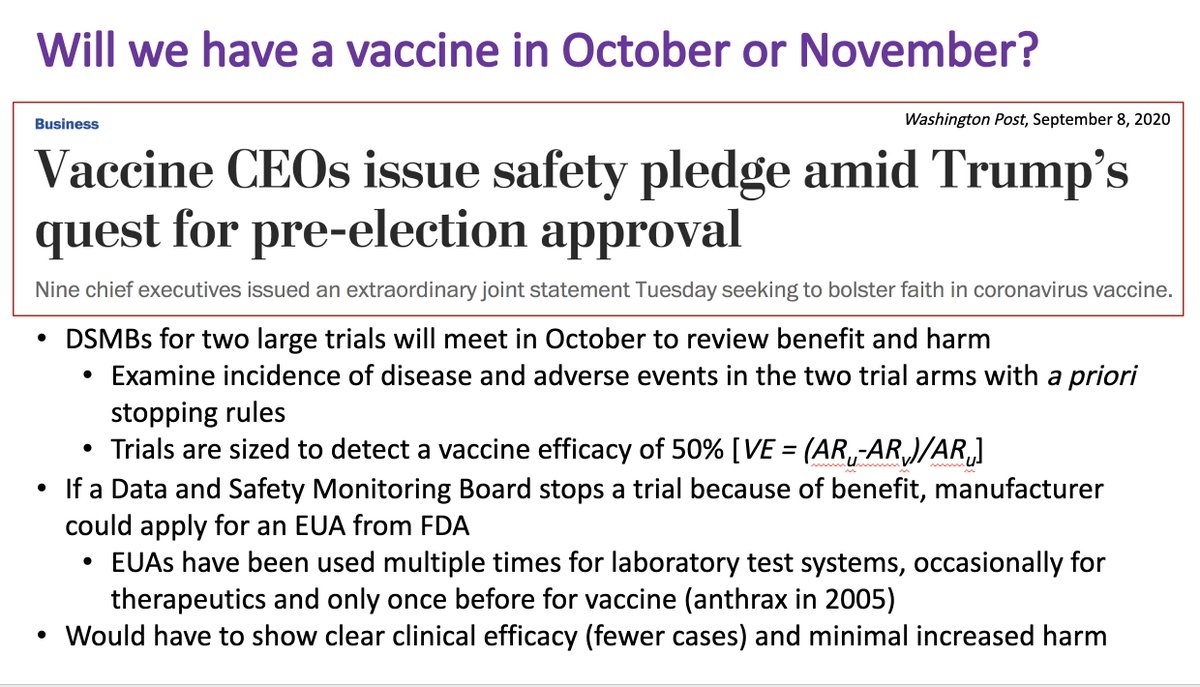
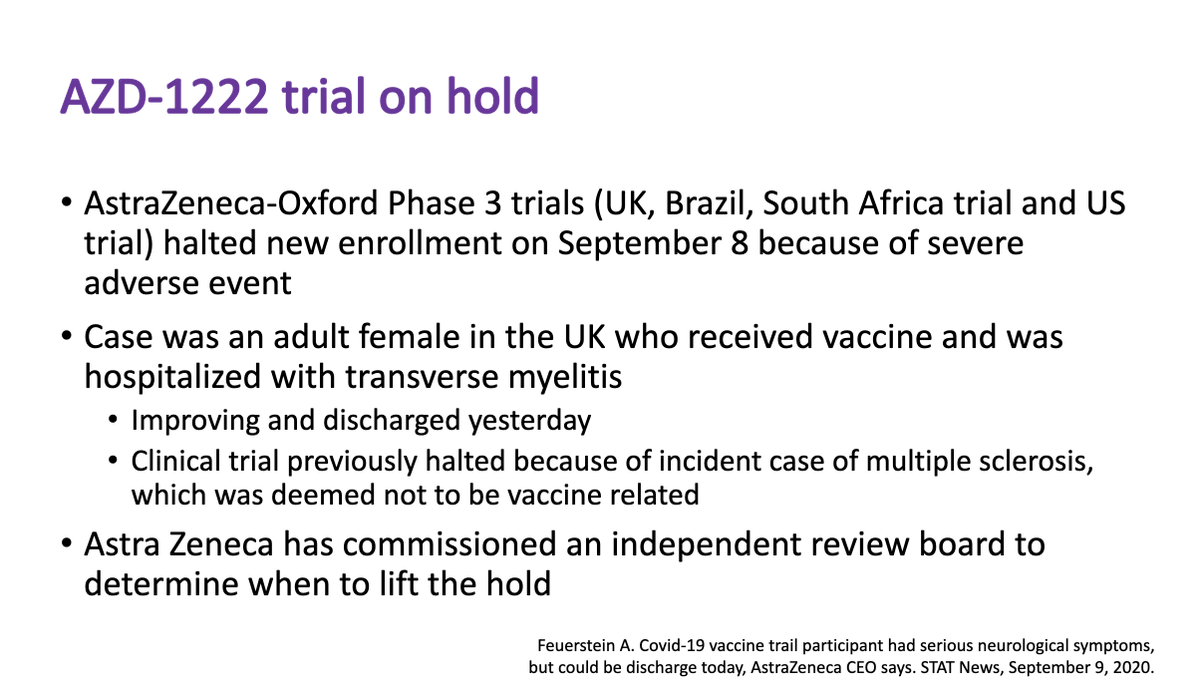
8/ As prelude to next week’s Grand Rounds (on vaccines), @ 22:00 George reviews the 3 major vaccine candidates; @AstraZeneca vaccine on hold due to pt w/ prob. transverse myelitis. Interesting fact: only 1 vaccine (for inhalational anthrax) has ever received EUA from @US_FDA. 

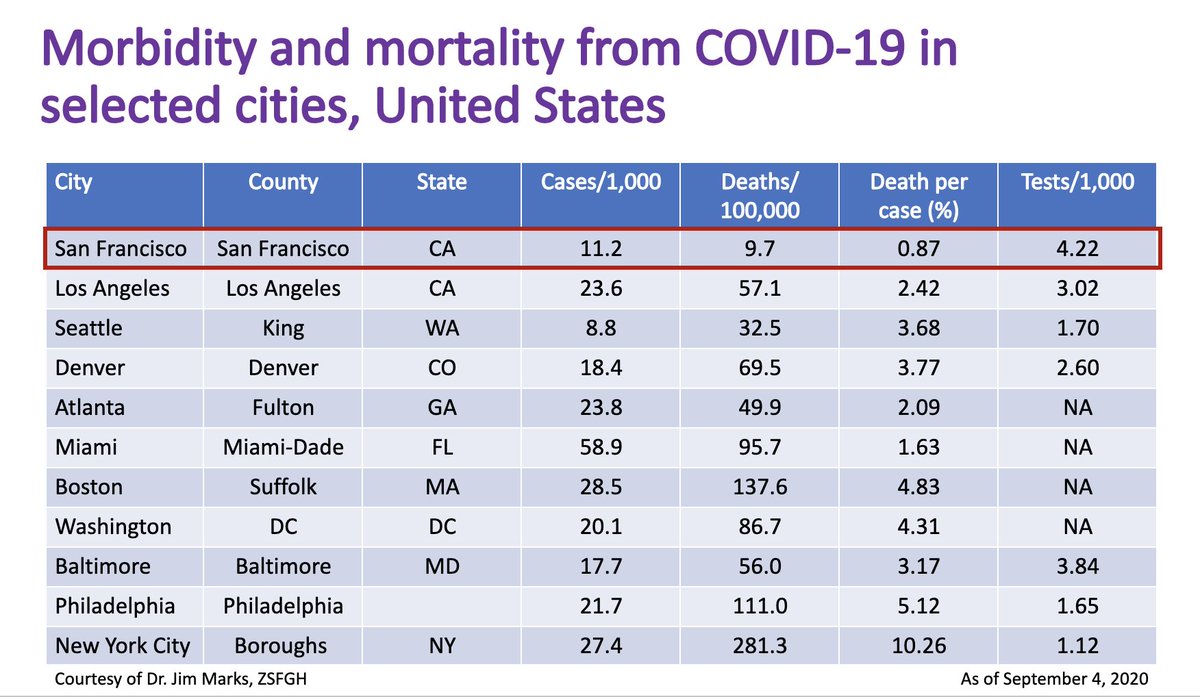
9/ Finally, moving toward @MonicaGandhi9’s talk on Covid's falling mortality rate, George (@ 18:00) showed fig below, which shows that SF not only has low case rate (though not as low as Seattle’s) but has had, by far, lowest rate of deaths/case (0.87%) of major U.S. cities. 
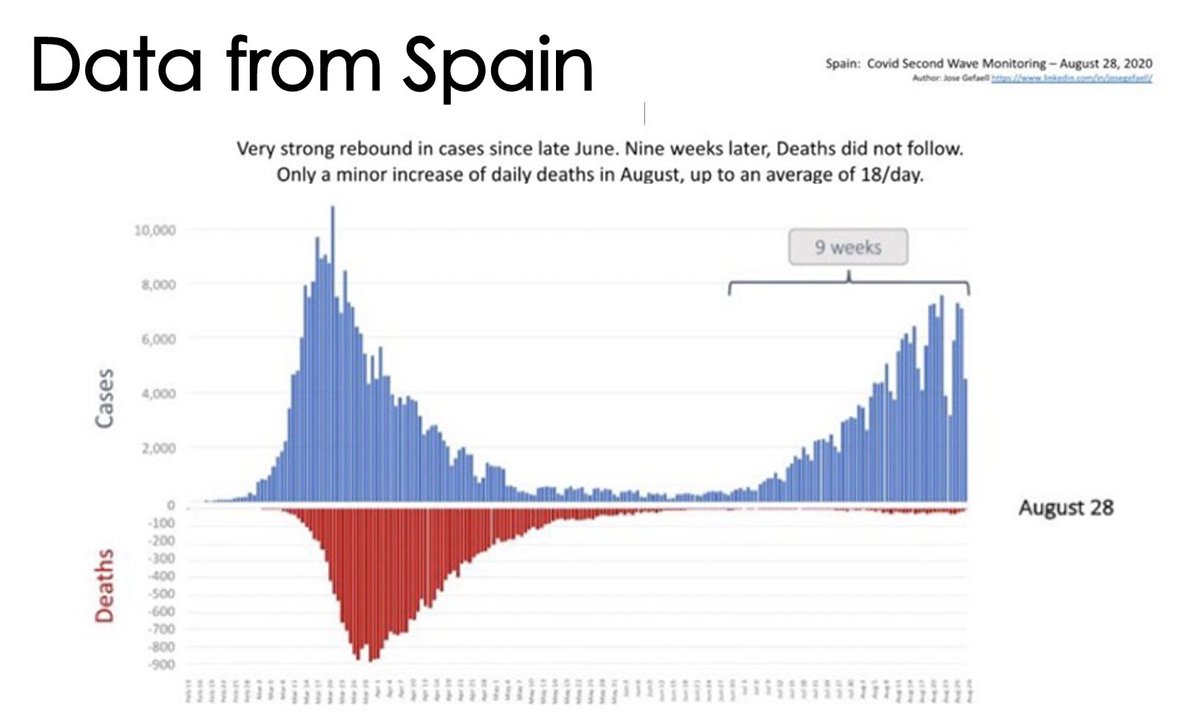
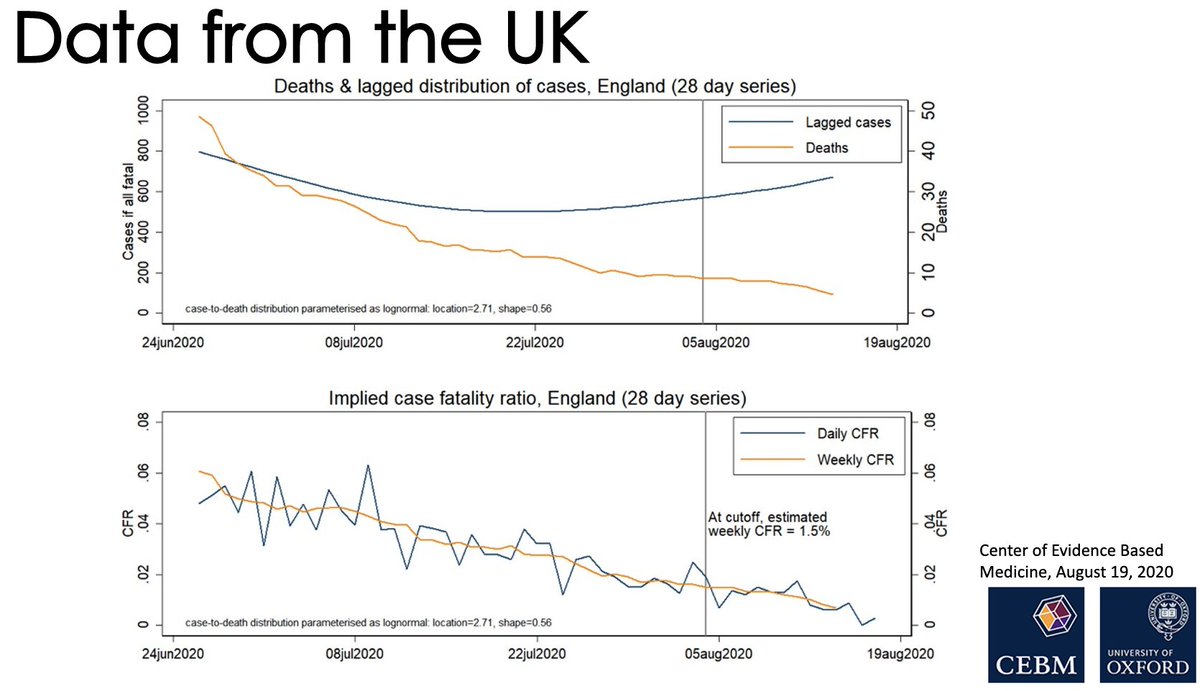
10/ Monica’s talk focused on the changing mortality rate in Covid. @ 35:00, here are amazing data from Spain (left) and UK (right) highlighting the striking fall in case-fatality rate. What’s going on? Younger age? Mask wearing? Immunity? Better treatments and approaches? 

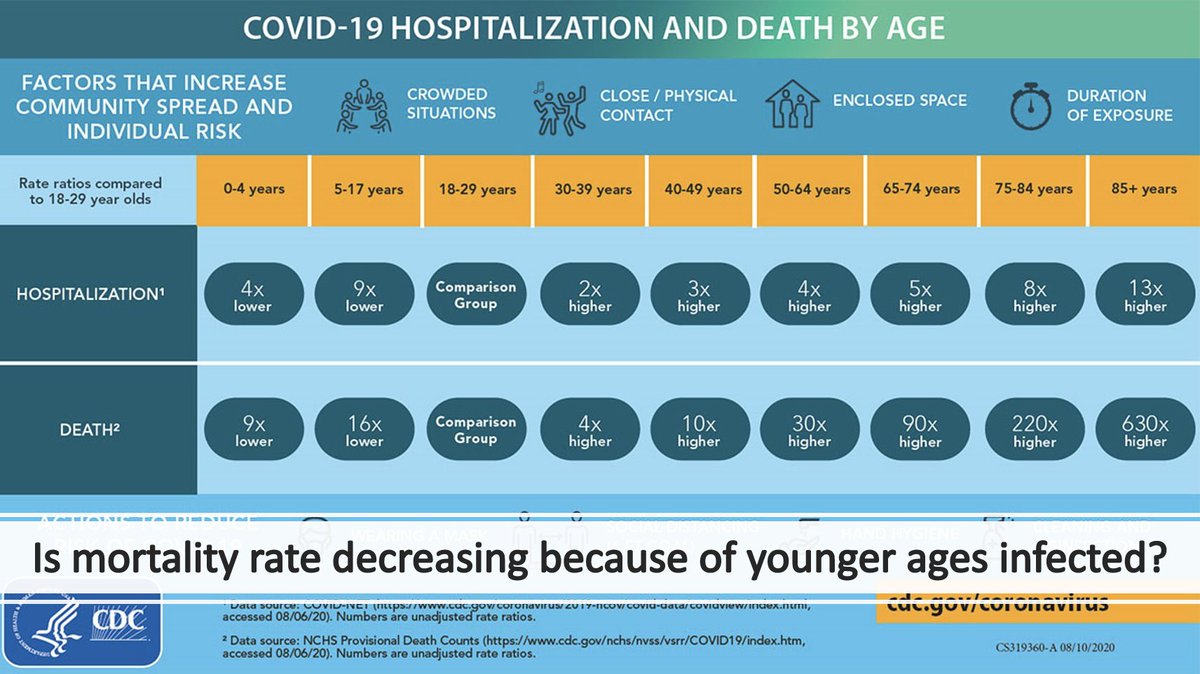
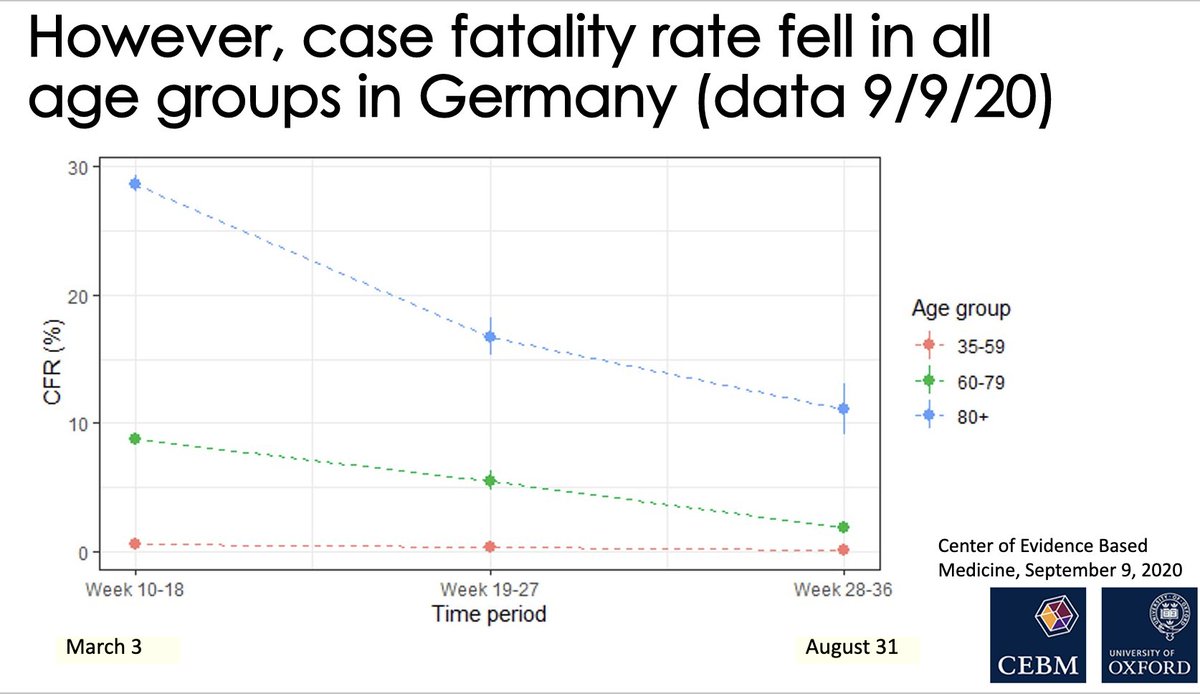
11/ Clearly (@ 37:00) Covid has shifted to younger people, & mortality is tightly linked to age, as per CDC diagram (on L). But these data from Germany (Fig R, @ 38:50) show falling mortality rate in each age group. Doesn’t look like age completely explains falling mortality. 

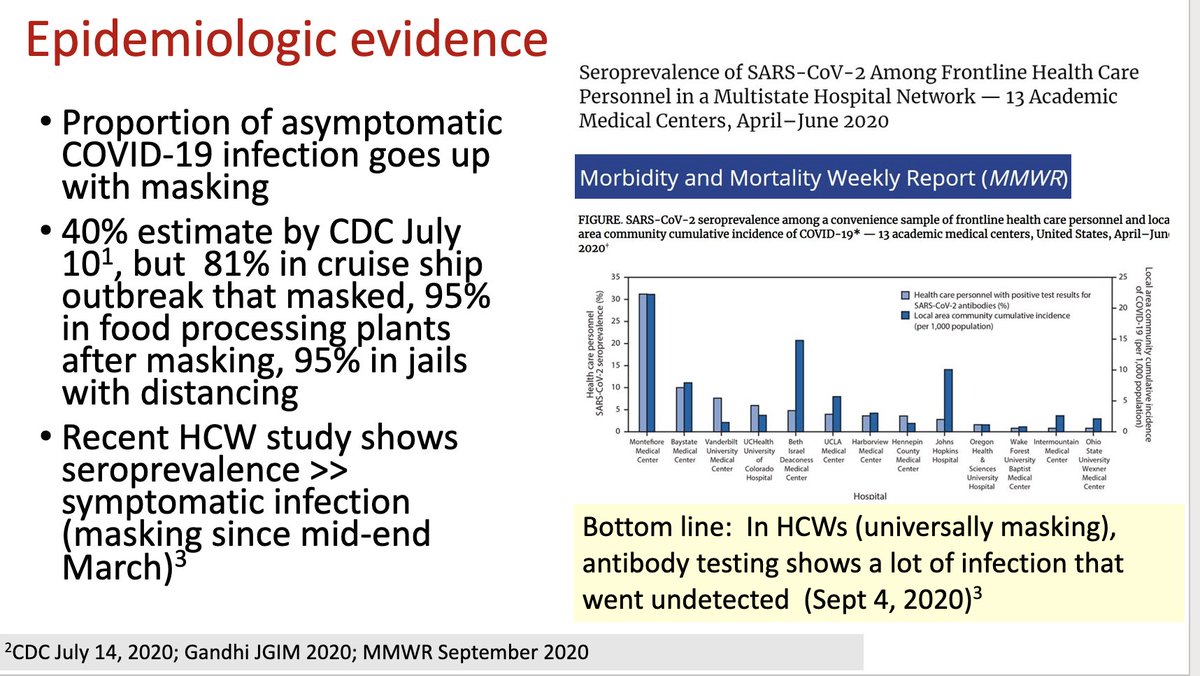
12/ So, is it masking? @ 39:40, Monica reviews her hypothesis that masks lead to lower viral inocula, which then leads to milder disease. She presented virologic evidence (@ 41:00) & epi evidence (below). Also, cities that have more masking (such as SF) have lower mortality rate. 
13/ Next, is immunity involved? Answer (@ 49:30) is also probably yes – per Monica and George’s interesting article in today’s @NEJM (tinyurl.com/y4bf9c8l), masking probably leads to the development of immunity in some people via low-grade viral exposure.
14/ Of course, therapies have made a difference – not just steroids & remdesivir but also less overwhelmed hospitals. Whereas NYC hospitals were crushed in March, few hospitals were overwhelmed in June/July (@ 56:00). This too is likely part of the explanation.
15/ @ 52:00, far-ranging Q&A w/ Monica and George. Monica clarifies that, even with falling mortality, a) Covid is still worse than flu; b) no evidence that viral mutations have made it milder; and c) improvements would evaporate if people stopped wearing masks and distancing. 

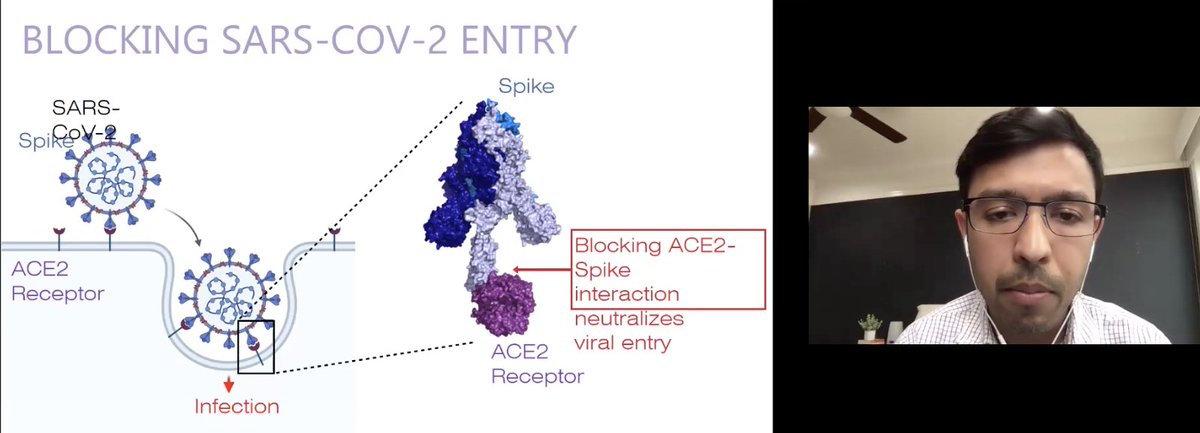
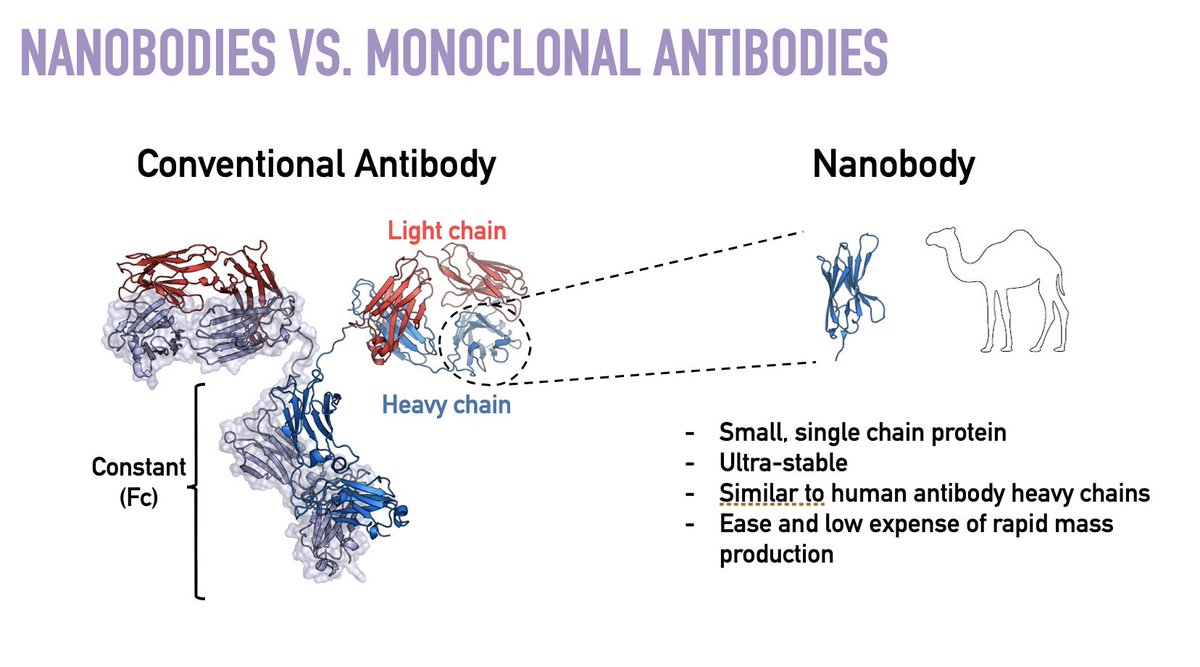
16/ Next @ 1:01:50: @AashishManglik on an innovative approach to Covid prevention. It’s a great story of scientific discovery: in a few months, dozens of @UCSF scientists & students discovered a novel way to block the virus’s ability to gain purchase to our respiratory tract… 
17/ …then, inspired by the llama’s immune system, they tested billions of nanobodies to find the one best able to bind the SARS-CoV-2 spike protein; found a way to build a molecule that would be stable in aerosol form & have high affinity for spike protein; and then tested it. 
18/ While this video is a bit simplistic, it is a nice depiction of the concept and its potential tinyurl.com/yydrxu72. At this point, the @UCSF investigators are working with industry in an effort to commercialize their discovery. The approach seems promising.
19/ @ 1:15:20, I asked Aashish re: clinical use. While I would have guessed that its main use would be in prevention (perhaps after high-risk exposures or in people at very high risk for Covid & bad outcomes), he also discussed its possible use early in the course of infection….
20/ ...since the virus’s spike protein (target of the nanobody) needs to bind to ACE-2 receptors to multiply and do its damage. Of course, finding people on the first day of their infection is a non-trivial problem – it requires a testing infrastructure that we currently lack.
21/ @ 1:24:00, I asked about whether the prospect of vaccines might make AeroNabs less commercially viable. I agree with his answer: even if we have a credible (non-politically determined) approval of a vaccine that is >50% effective sometime in the next 3 months …
22/ ... we’re still looking at a year before we will have widespread distribution of the vaccine. And we may have a vaccine uptake of only 40-60%. So, if AeroNabs pan out, they could easily find a major role in 2021, notwithstanding good (and hoped for!) progress on vaccines.
23/ Another great session, again here: tinyurl.com/yyw5myns. Next week, all-thing-vaccines w/ @PeterHotez.
Moving my weekly long tweet thread to Mondays; this Monday I'll focus on changing nature–& growing challenge–of risk assessment as we try to live our lives. Stay safe.
Moving my weekly long tweet thread to Mondays; this Monday I'll focus on changing nature–& growing challenge–of risk assessment as we try to live our lives. Stay safe.
• • •
Missing some Tweet in this thread? You can try to
force a refresh