1/
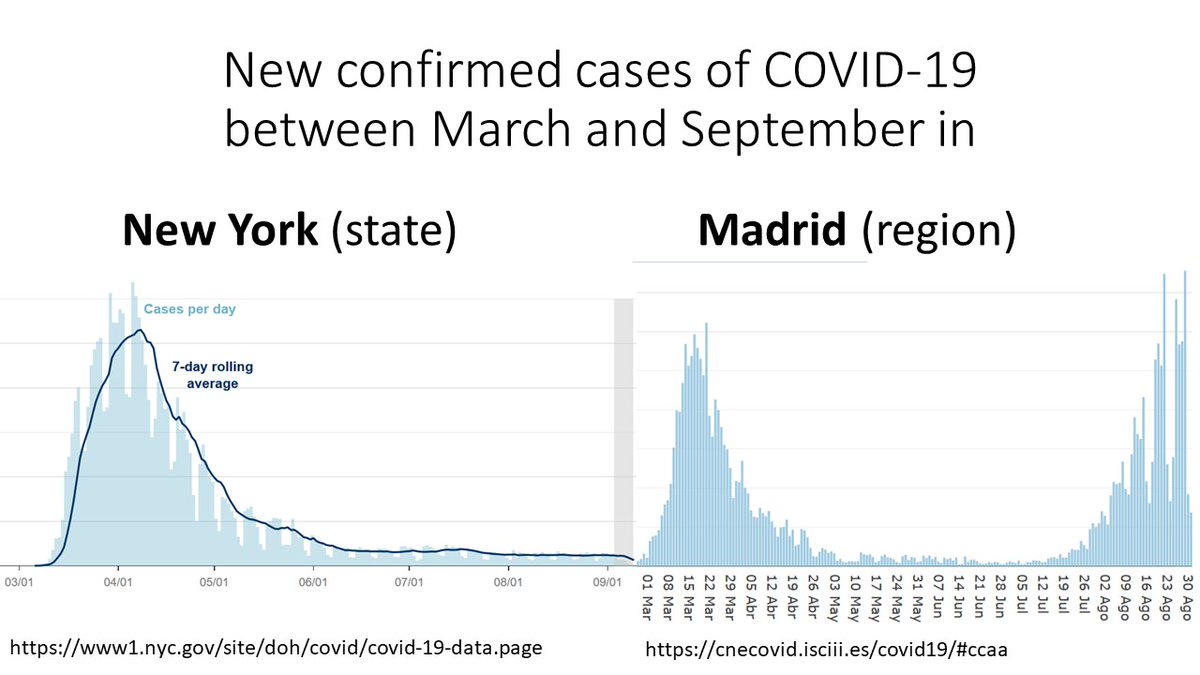
Look at the shape of these curves.
New York and Madrid had similar epidemics until they spectacularly diverged.
In March, both cities were caught by surprise and shut down because of #COVID19.
In September, the situation is under control in NY and alarming in Madrid.
Why?
Look at the shape of these curves.
New York and Madrid had similar epidemics until they spectacularly diverged.
In March, both cities were caught by surprise and shut down because of #COVID19.
In September, the situation is under control in NY and alarming in Madrid.
Why?
2/
Let’s start with the similarities: two big, dense cities with a large network of public transit and lots of visitors.
An explosive outbreak of #SARSCOV2 overwhelmed their contact tracing system and their hospitals. A lockdown was required to reduce the public health disaster.
Let’s start with the similarities: two big, dense cities with a large network of public transit and lots of visitors.
An explosive outbreak of #SARSCOV2 overwhelmed their contact tracing system and their hospitals. A lockdown was required to reduce the public health disaster.
3/
By June, both places had succeeded in bringing down the number of new cases. That's precisely what lockdowns do.
In July, new cases started to increase in Madrid until reaching one of the highest incidences in Europe.
New York has not seen any increase in new cases yet.
By June, both places had succeeded in bringing down the number of new cases. That's precisely what lockdowns do.
In July, new cases started to increase in Madrid until reaching one of the highest incidences in Europe.
New York has not seen any increase in new cases yet.
4/
We could argue that number of new #COVID19 cases isn't the best metric for the severity of the #SARSCOV2 epidemic. Perhaps most cases are asymptomatic or mildly symptomatic?
Let's then look at hospital occupation. No problem in New York. Serious trouble brewing in Madrid.
👇
We could argue that number of new #COVID19 cases isn't the best metric for the severity of the #SARSCOV2 epidemic. Perhaps most cases are asymptomatic or mildly symptomatic?
Let's then look at hospital occupation. No problem in New York. Serious trouble brewing in Madrid.
👇

5/
So what happened?
#NewYork and #Madrid had significantly different responses in terms of contact tracing, number of tests, and speed of reopening.
Let’s review each of these elements.
This comparison is a case study on epidemic management in hub cities around the world.
So what happened?
#NewYork and #Madrid had significantly different responses in terms of contact tracing, number of tests, and speed of reopening.
Let’s review each of these elements.
This comparison is a case study on epidemic management in hub cities around the world.
6/
CONTACT TRACING
New York state aimed at 30 contact tracers per 100,000 people before reopening. Minimum.
That translates into 6000 contract tracers in New York and 2000 in Madrid.
Madrid had about 200 contact tracers in July (maybe 700 now). An order of magnitude difference.
CONTACT TRACING
New York state aimed at 30 contact tracers per 100,000 people before reopening. Minimum.
That translates into 6000 contract tracers in New York and 2000 in Madrid.
Madrid had about 200 contact tracers in July (maybe 700 now). An order of magnitude difference.
7/
TESTING
In April, >70% of PCRs were positive in both New York and Madrid.
New York aimed at achieving <5% positivity before reopening. It is now 1-2%.
www1.nyc.gov/site/doh/covid…
Positivity in Madrid is ~20% and increasing since July. That is, not nearly enough tests are done.
TESTING
In April, >70% of PCRs were positive in both New York and Madrid.
New York aimed at achieving <5% positivity before reopening. It is now 1-2%.
www1.nyc.gov/site/doh/covid…
Positivity in Madrid is ~20% and increasing since July. That is, not nearly enough tests are done.
8/
SPEED OF REOPENING
Let's focus on indoor dining, a vital economic activity in both #NewYork and #Madrid, and arguably one of the main sources of transmission of the #coronavirus.
SPEED OF REOPENING
Let's focus on indoor dining, a vital economic activity in both #NewYork and #Madrid, and arguably one of the main sources of transmission of the #coronavirus.
9/
Indoor dining in New York is CLOSED.
It'll open on September 30 at 25% capacity (50% on November 1) with
- NO bar service.
- Strict protocols
- Phone number to report violations
- Deployment of hundreds of enforcement personnel to ensure compliance
forward.ny.gov/nyc-indoor-din…
Indoor dining in New York is CLOSED.
It'll open on September 30 at 25% capacity (50% on November 1) with
- NO bar service.
- Strict protocols
- Phone number to report violations
- Deployment of hundreds of enforcement personnel to ensure compliance
forward.ny.gov/nyc-indoor-din…
10/
Indoor dining in Madrid was OPEN at 60% capacity in June.
Bar service opened too.
Protocols weren't aggressively enforced.
Since June it has been easy to find crowded bars and tables. The contrast with NY was striking as anyone spending time in both places can tell you.
Indoor dining in Madrid was OPEN at 60% capacity in June.
Bar service opened too.
Protocols weren't aggressively enforced.
Since June it has been easy to find crowded bars and tables. The contrast with NY was striking as anyone spending time in both places can tell you.
11/
Contact tracing, testing, and speed of reopening differed dramatically between #NewYork and #Madrid.
New York opened the economy without overwhelming the hospitals and confirmed its credentials as a serious place to do business.
By simply doing what experts say since March.
Contact tracing, testing, and speed of reopening differed dramatically between #NewYork and #Madrid.
New York opened the economy without overwhelming the hospitals and confirmed its credentials as a serious place to do business.
By simply doing what experts say since March.
12/
A colleague asked whether New York may have reached "herd immunity" whereas Madrid has not. That'd explain the low number of cases in NY.
Unlikely. Based on the available seroprevalence studies, both places had a similar % of population who developed antibodies to #SARSCOV2.
A colleague asked whether New York may have reached "herd immunity" whereas Madrid has not. That'd explain the low number of cases in NY.
Unlikely. Based on the available seroprevalence studies, both places had a similar % of population who developed antibodies to #SARSCOV2.
13/
Of course, bad luck can never be ruled out in epidemics.
A spark at the right time may ignite a wildfire in one place but not another.
But bad luck seems a poor explanation for the NY-Madrid differences after comparing their testing, contact tracing, and reopening policies.
Of course, bad luck can never be ruled out in epidemics.
A spark at the right time may ignite a wildfire in one place but not another.
But bad luck seems a poor explanation for the NY-Madrid differences after comparing their testing, contact tracing, and reopening policies.
14/
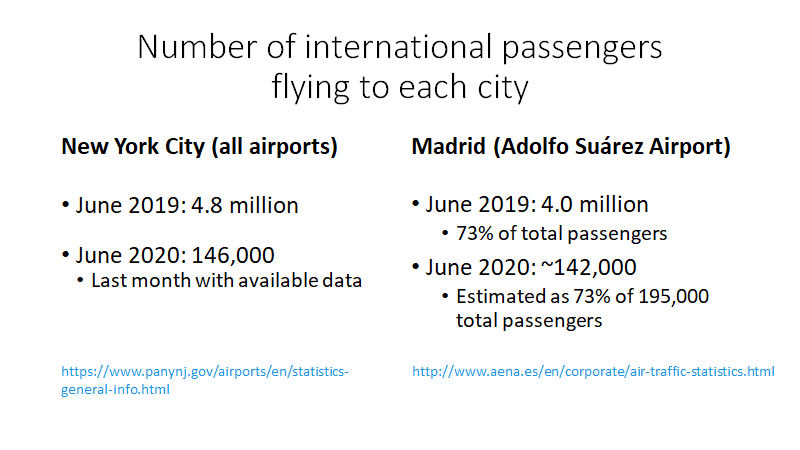
Finally, some people have asked whether differences in number of international passengers may explain the different epidemic Summer in #NYC and #Madrid.
Unlikely.
NYC and Madrid had a very similar influx of international passengers, both before and after the lockdown.
Finally, some people have asked whether differences in number of international passengers may explain the different epidemic Summer in #NYC and #Madrid.
Unlikely.
NYC and Madrid had a very similar influx of international passengers, both before and after the lockdown.
15/
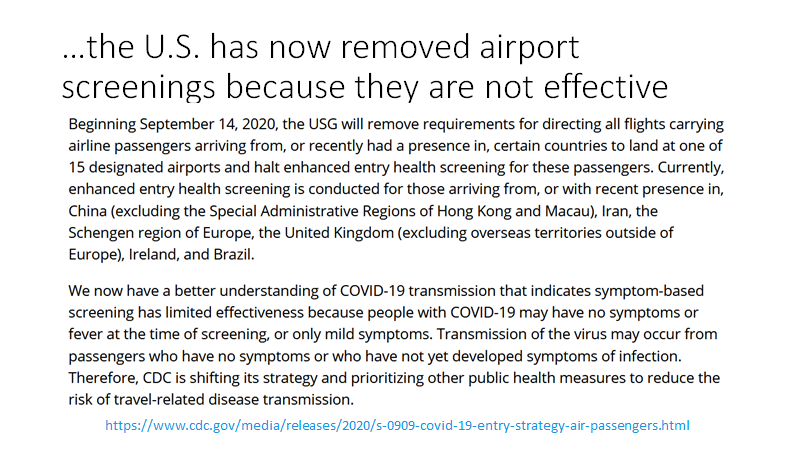
Maybe passenger screening was stricter in the U.S.?
Of 675,000 passengers screened in *all* U.S. airports, 15 were identified with #COVID19.
If Spain had implemented the U.S. screening procedures, Madrid would have found too few cases to explain the difference.
In fact...
Maybe passenger screening was stricter in the U.S.?
Of 675,000 passengers screened in *all* U.S. airports, 15 were identified with #COVID19.
If Spain had implemented the U.S. screening procedures, Madrid would have found too few cases to explain the difference.
In fact...
• • •
Missing some Tweet in this thread? You can try to
force a refresh