Back on COVID-19 service this month
Went to see this patient with "increased respiratory drive despite high dose sedation and NMB". This is the vent: 1/4
Went to see this patient with "increased respiratory drive despite high dose sedation and NMB". This is the vent: 1/4
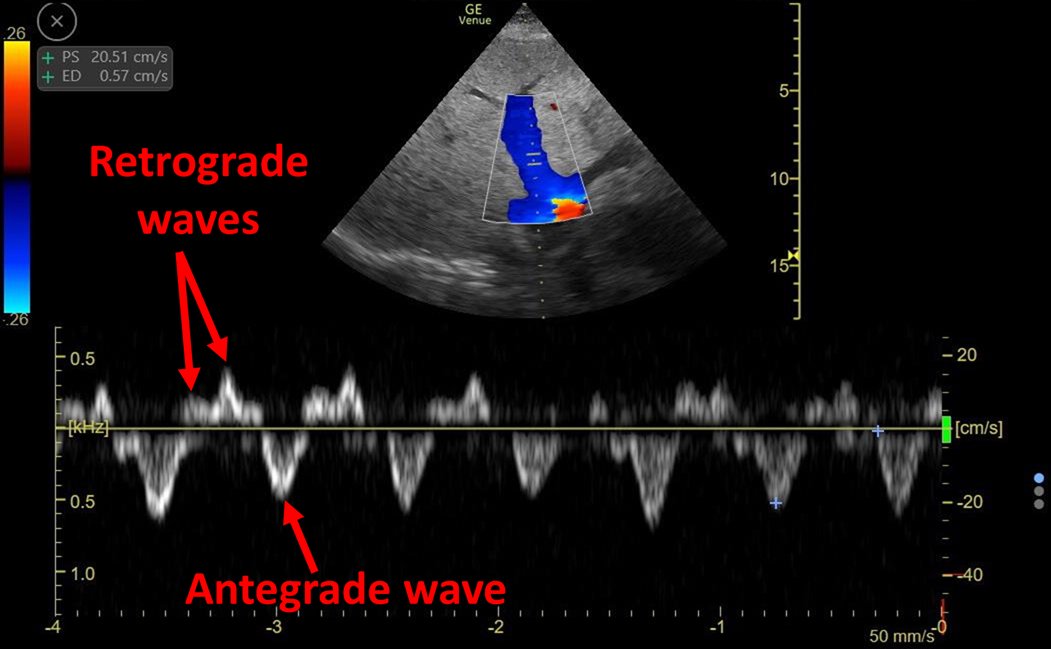
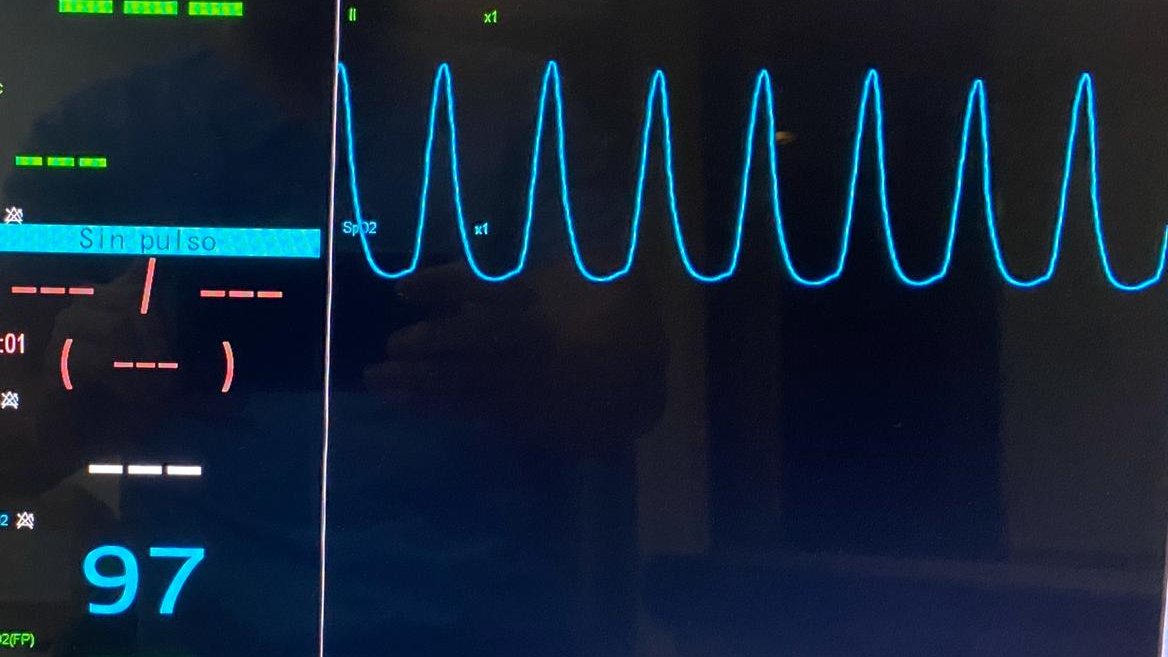
Looking at the patient's monitor, the respiratory curve seems oddly coincident with heart rate: 2/4
Inspiratory pause reveals NO respiratory drive and several cardiogenic oscillations! 3/4
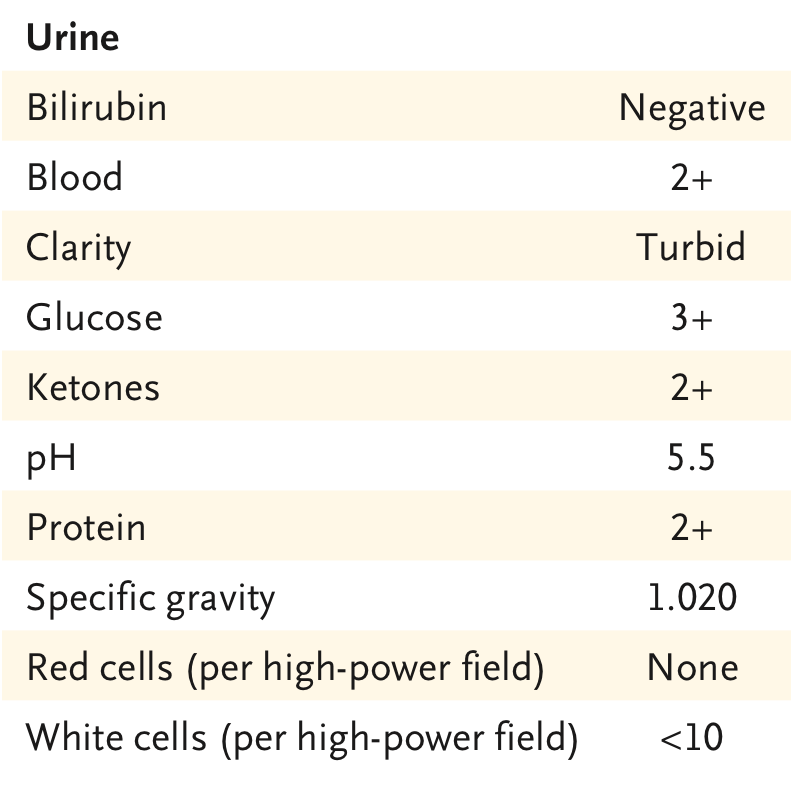
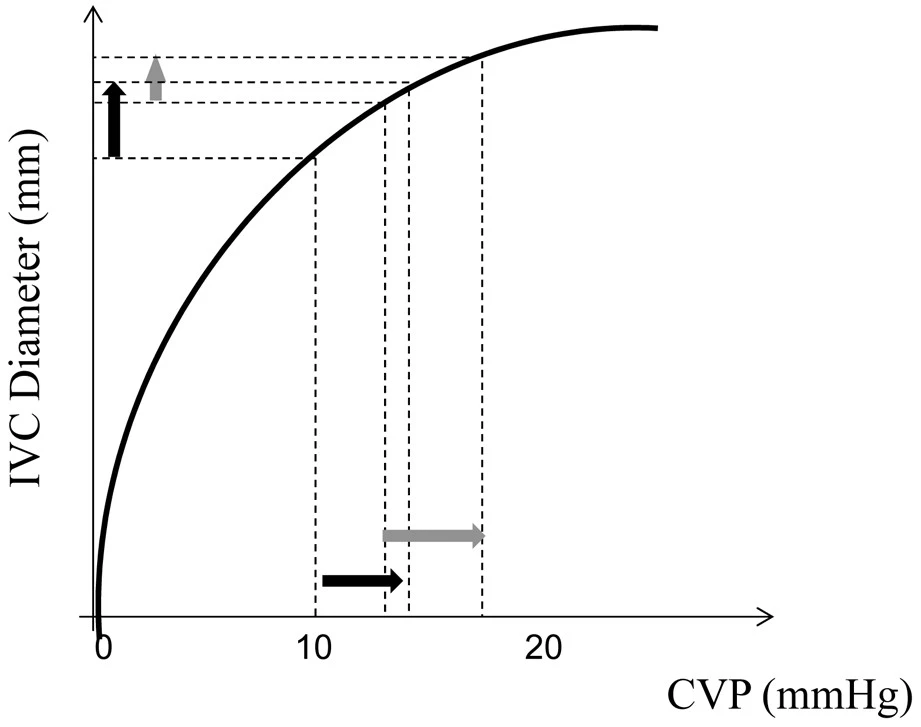
Trigger was 3.0 l/min so I increased it to 6 l/min. Afterwards I was able to stop NMB and lower sedation.
Diagnosis: Auto Triggering (triggering secondary to cardiogenic oscillations) 4/4
Diagnosis: Auto Triggering (triggering secondary to cardiogenic oscillations) 4/4
• • •
Missing some Tweet in this thread? You can try to
force a refresh