A case for hepatic vein Doppler lovers:
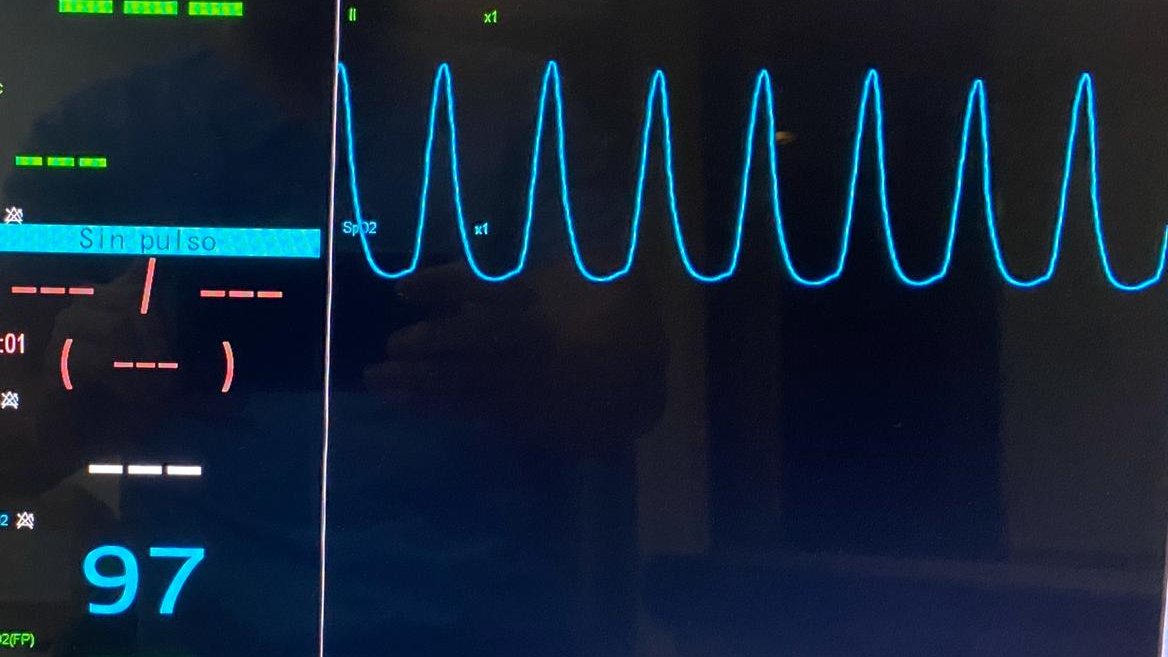
ECG tracing not abvailable on the ultrasound machine (I tried, I swear)
Can we still interpret this HV waveform without ECG?
I speculate we can!
I'll try to do it step by step: 1/7
ECG tracing not abvailable on the ultrasound machine (I tried, I swear)
Can we still interpret this HV waveform without ECG?
I speculate we can!
I'll try to do it step by step: 1/7

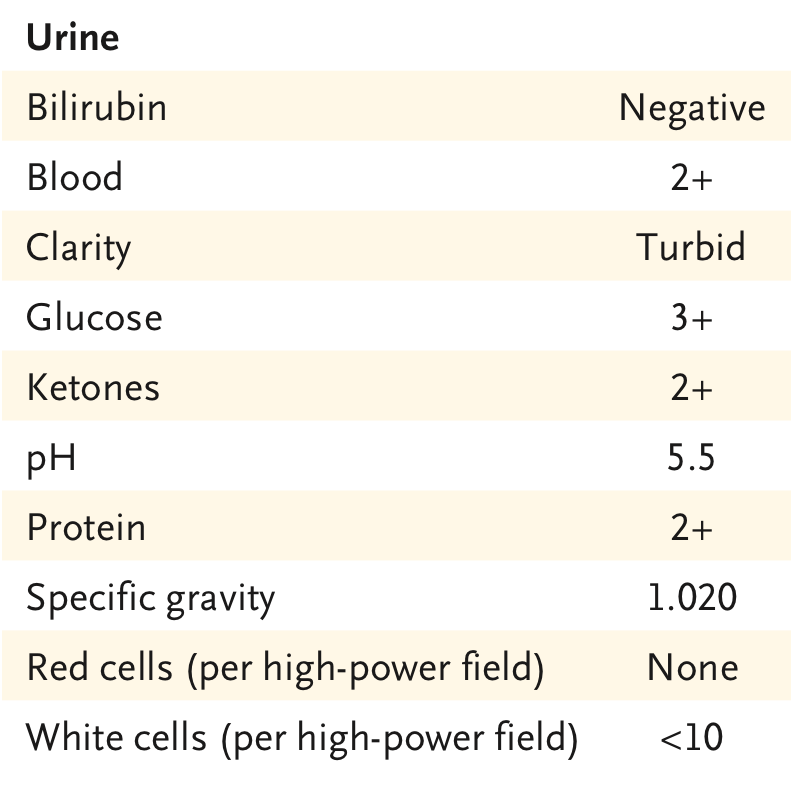
What can we tell?
For one, there are 2 retrograde waves and 1 antegrade wave.
Given the patient was in sinus rhythm, then one of the retrograde waves MUST be an A wave! 2/7

For one, there are 2 retrograde waves and 1 antegrade wave.
Given the patient was in sinus rhythm, then one of the retrograde waves MUST be an A wave! 2/7
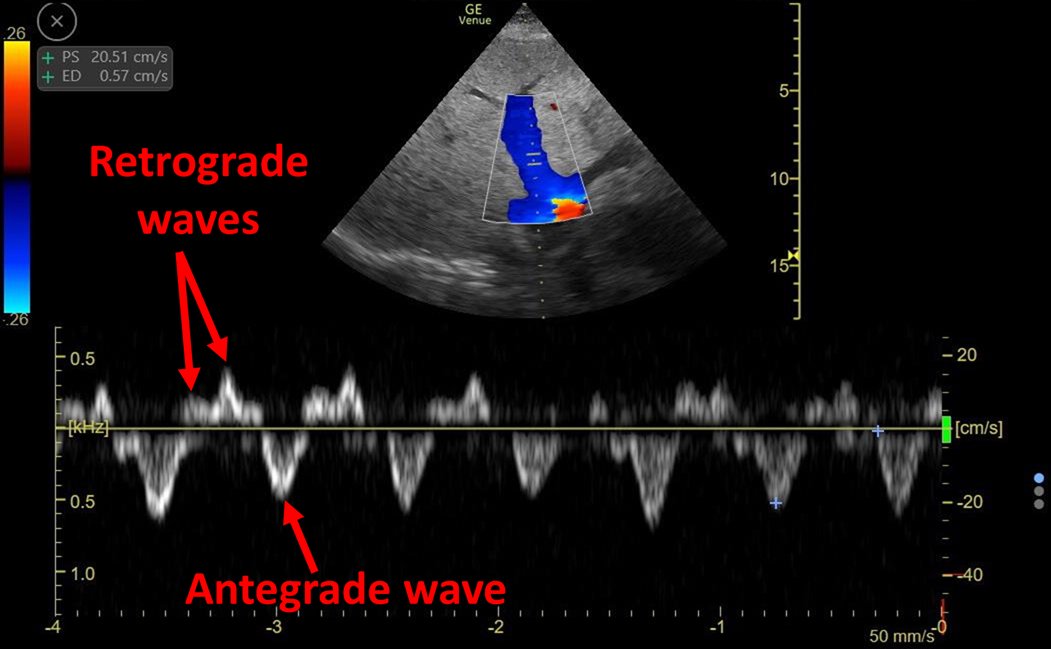

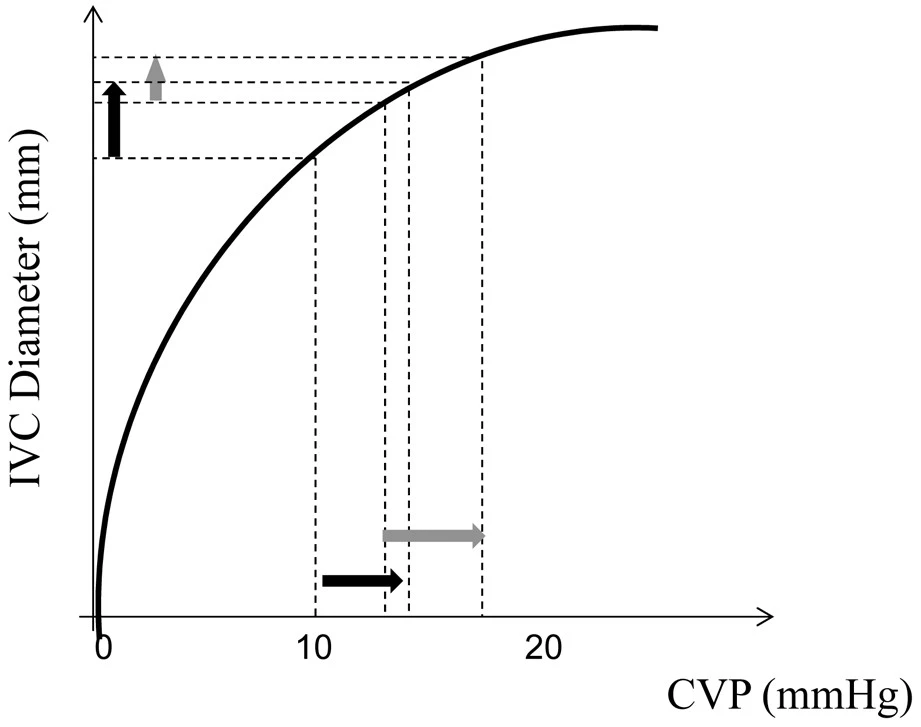
Given HV waveform sequence should always be A-S-D, AND A wave is always retrograde:
Then this leaves only 2 possibilities: There could either be S wave reversal or D wave reversal 3/7

Then this leaves only 2 possibilities: There could either be S wave reversal or D wave reversal 3/7


**this may be a stretch but...If we look closer and asume the antegrade wave is systolic there might even be an S1 and an S2 wave (The notch between S1 and S2 representing tricuspid valve closure or "c" wave on CVP). Here are several tracings I obtained: 4/7 





Without ECG, Is it impossible to know if the antegrade wave = S wave? I don't think so! This antegrade wave should be visible on intra-renal venous doppler which has a simultaneous arterial waveform. Looking at this, it seems the antegrade venous wave happens in systole! 5/7 


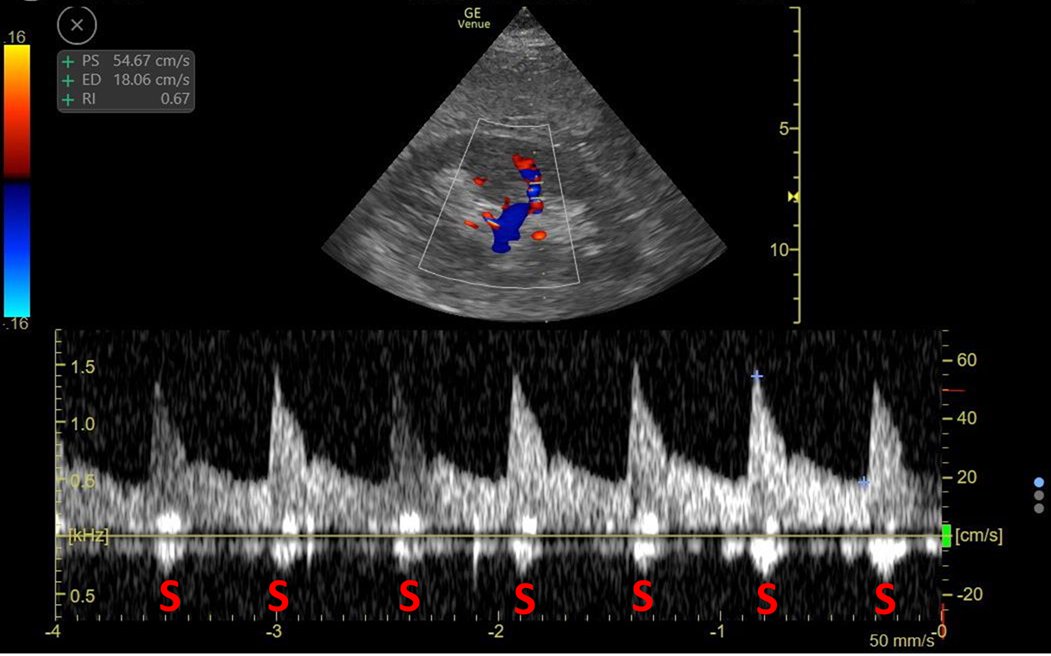


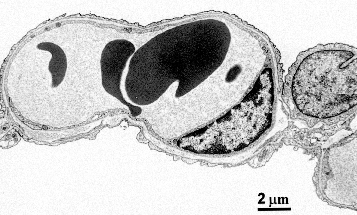
Lastly, if this analysis is wrong, then there is S wave reversal and we would expect severe TR to be the underlying pathology. Here is the heart! Patient had all the signs of tamponade physiology (Trans-Mitral variation, RV collapse) and no significant TR. 6/7
Classically expiratory D wave reversal has been well described in tamponade. Oddly in this patient it occured all throughout the respiratory cycle. However I think everything points to D wave reversal. But hey this whole thread is pure speculation! 7/7
ping Doppler Nerds 🤓 @Thind888 @ThinkingCC @khaycock2 @NephroP @msenussiMD @iceman_ex
I'd appreciate some of your insigts!
I'd appreciate some of your insigts!
• • •
Missing some Tweet in this thread? You can try to
force a refresh