@GallodeMoraesMD will be live tweeting the #PICS talk @accp #CHESTCritCare
@crit_caring_MD @GioraNetzer @itsradu @ICU_Recovery are talking about #PICS now!
@crit_caring_MD @GioraNetzer @itsradu @ICU_Recovery are talking about #PICS now!
At 12 months only 44% of ICU survivors are PICS-free, being cognitive a significative part of the post-ICU impairment. With more ICU survivors, we will likely be seeing more PICS. #CHEST2020 #CHESTCritCare
The lack of visitors in the COVID-19 era, will likely contribute to higher number of survivors with PICS #CHEST2020 #CHESTCritCare
@GioraNetzer reminds us that who is family is determined by the patients. Family engagement is part of the ABCDEF bundle of ICU liberation. 57% of ICU survivors require care by a caregiver after ICU discharge. Patients with good social support do better.
sciencedirect.com/science/articl…
sciencedirect.com/science/articl…
Sequela of critical illness are seen well passed ICU discharge, both in patients and their families. One year after ICU discharge, many caregivers have PTSD, depression and anxiety.
journals.lww.com/ccmjournal/Abs…
journals.lww.com/ccmjournal/Abs…
Majority of ICU survivors will have a family member who will have a major change in life-style: loss income, change in jobs/schedules to be able to care for the survivor.
#CHEST2020 #CHESTCritCare @accpchest
#CHEST2020 #CHESTCritCare @accpchest
The caregivers will need support as well: they will need counseling, psychoeducational interventions, support group and respite. The caregiver should be taken into consideration when a PICS clinic is being planned. #PICS #CHEST2020
Keeping family members engaged is helpful to prevent PICS in survivors and helps with PTSD and anxiety in family members. It is our obligation to provide a tablet or video-conferencing capability to family members in order to decrease social injustices during COVID-19 era.
@itsradu reminds us of the most frequent readmission diagnoses after sepsis survival are new/recurrent infections, CHF exacerbation, AKI, COPD exacerbation, aspiration pneumonia
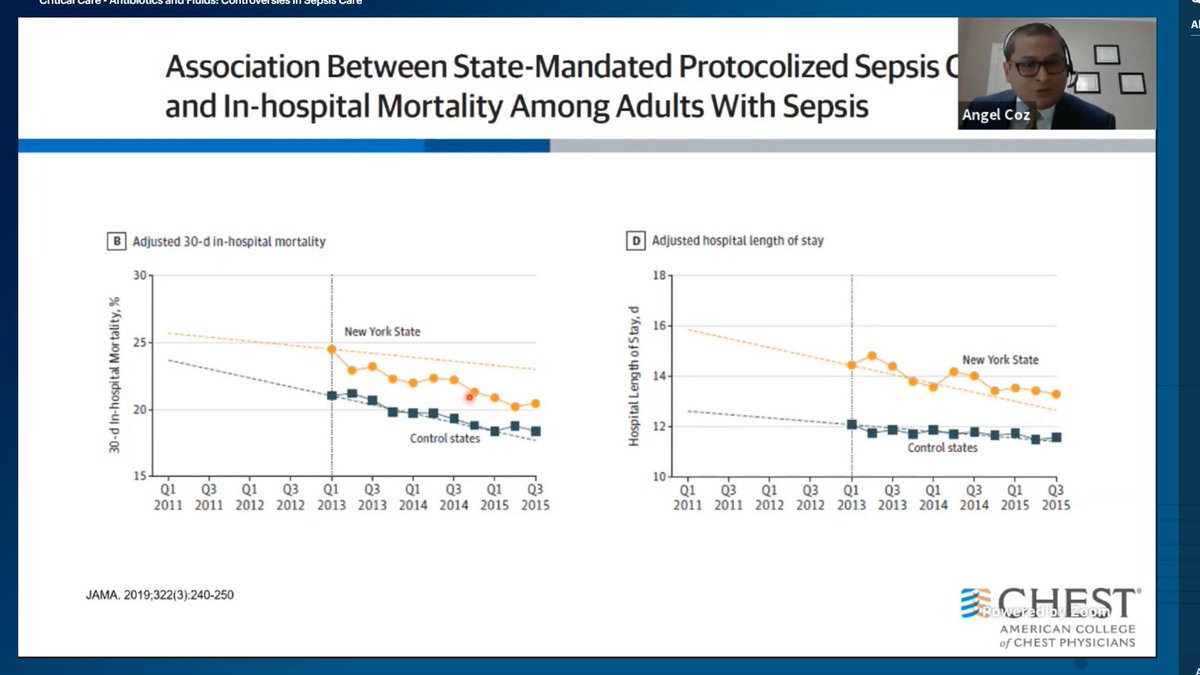
jamanetwork.com/journals/jama/…
jamanetwork.com/journals/jama/…
Pre-existing cognitive dysfunction/mental health is a risk factor for the development of #PICS, these patients would benefit from more aggressive implementation of the ABCDEF bundle. #CHEST2020 #CHESTCritCare
Proactive contact by case-managers with telephone calls soon after discharge prevents readmissions, increases survival and is also cost-saving. #CHESTCritCare #CHEST2020
• • •
Missing some Tweet in this thread? You can try to
force a refresh