Get your popcorn ready because this is going to be quite the learning contest. #CHEST2020
The webinar is LIVE in T - 5mins, speakers are checking their 🎤🎤
We are only a tiny bit biased towards our co-chair @GallodeMoraesMD!
The webinar is LIVE in T - 5mins, speakers are checking their 🎤🎤
We are only a tiny bit biased towards our co-chair @GallodeMoraesMD!
https://twitter.com/virenkaul/status/1318992846582652929
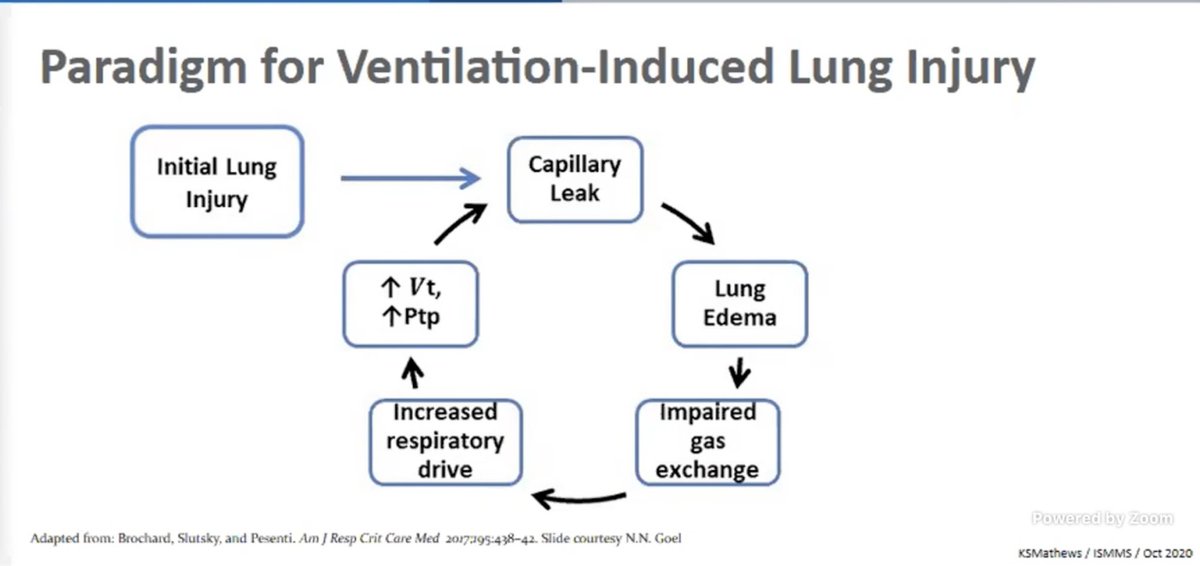
Dr. Mathews: Starts with sharing what drives ventilation-induced lung injury. This is "leak" is likely more pronounced in #COVID19
#CHEST2020
#CHEST2020
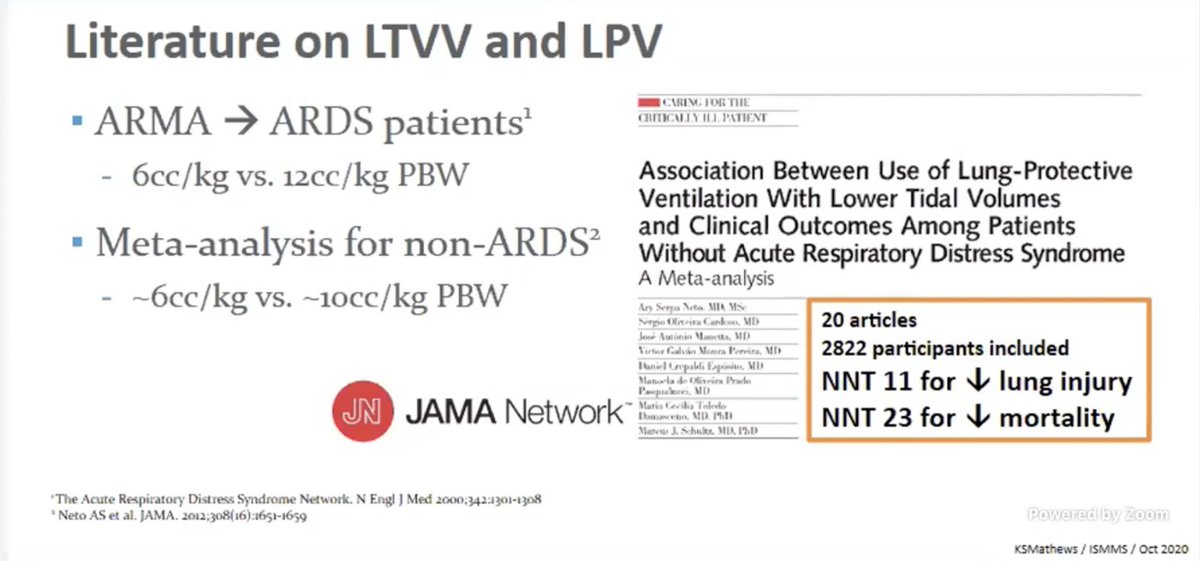
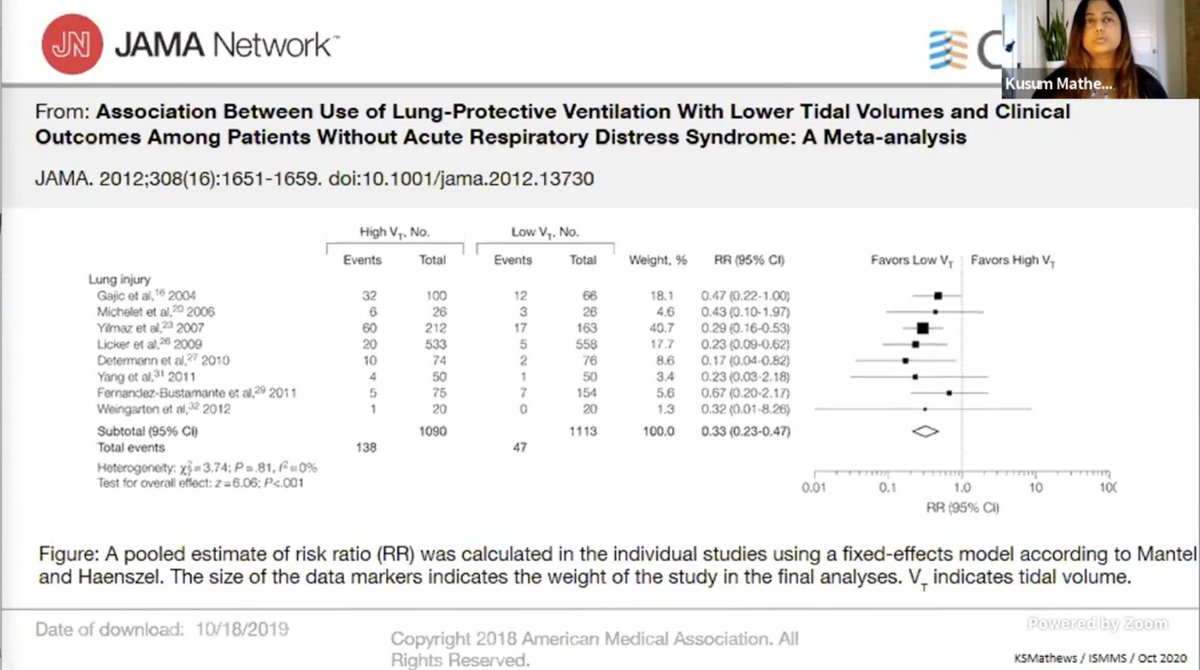
Dr. Mathews: ARMA supported LTVV in ARDS with significantly improved mortality. LTVV has been since found to be beneficial in non ARDS situations. #CHEST2020 


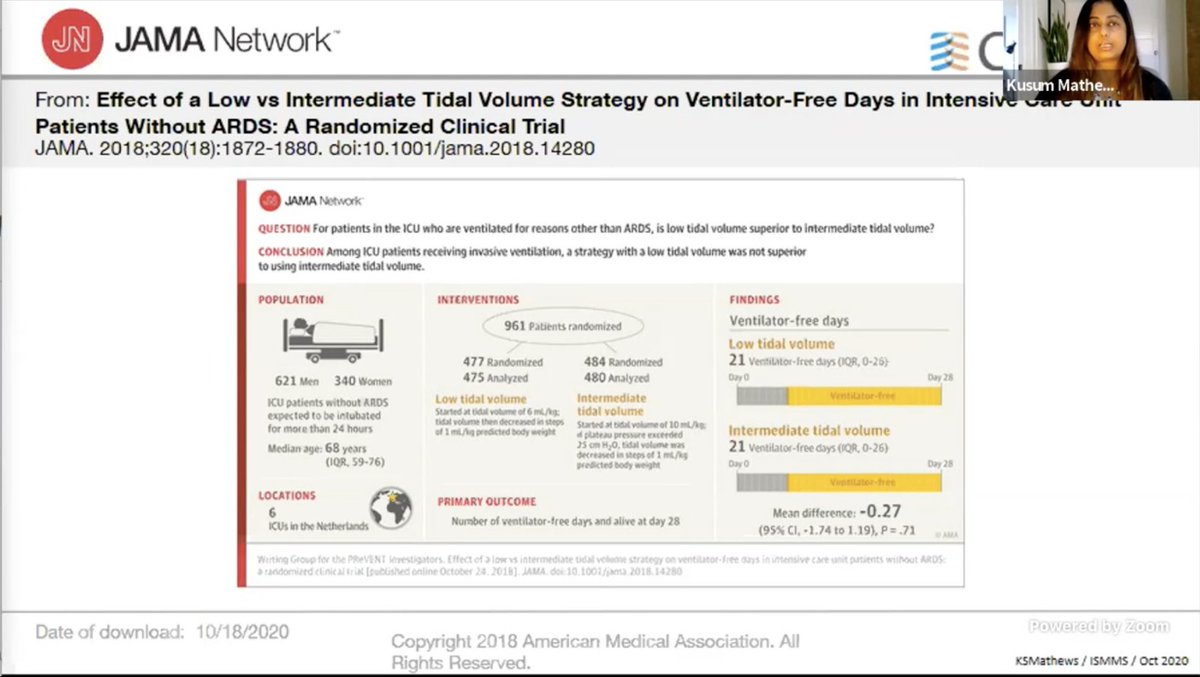
PReVENT trial: Low vs intermediate TV strategy in patients with non ARDS. No diff in vent free days.
However, limitations:
- No diff in sedation use
- Poor separation in terms of TV b/w groups
- Low enrollment
#CHEST2020
However, limitations:
- No diff in sedation use
- Poor separation in terms of TV b/w groups
- Low enrollment
#CHEST2020
LUNG-SAFE: We are bad at recognizing #ARDS and then implementing LTVV.
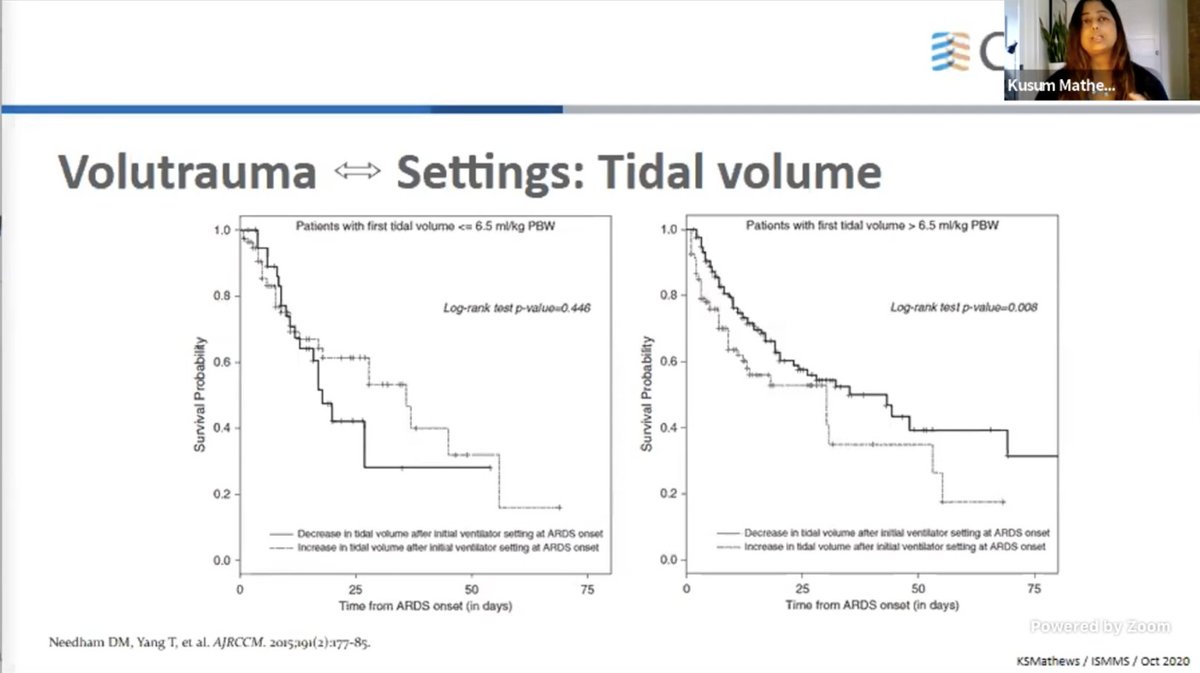
Needham et al showed the initial TV being low matters too.
That's why Dr. M makes a point to use LTV early and across the spectrum.
#CHEST2020


Needham et al showed the initial TV being low matters too.
That's why Dr. M makes a point to use LTV early and across the spectrum.
#CHEST2020


Also, despite nudges, 1/3rd patients did not get LTVV.
Hence changing the "default" management i.e. early ARDS recognition and implementation of LTVV is important, Dr. M advocates!
#CHEST2020

Hence changing the "default" management i.e. early ARDS recognition and implementation of LTVV is important, Dr. M advocates!
#CHEST2020


Dr. M: Remember other factors affecting the vent settings:
- Place of intubation
- Who's implementing settings
- Work load
- Cognitive load
Hence standardized implementation of LTVV is important.
Dr. M reminds everyone to implement LTVV for #COVID19 as well.
#CHEST2020
- Place of intubation
- Who's implementing settings
- Work load
- Cognitive load
Hence standardized implementation of LTVV is important.
Dr. M reminds everyone to implement LTVV for #COVID19 as well.
#CHEST2020
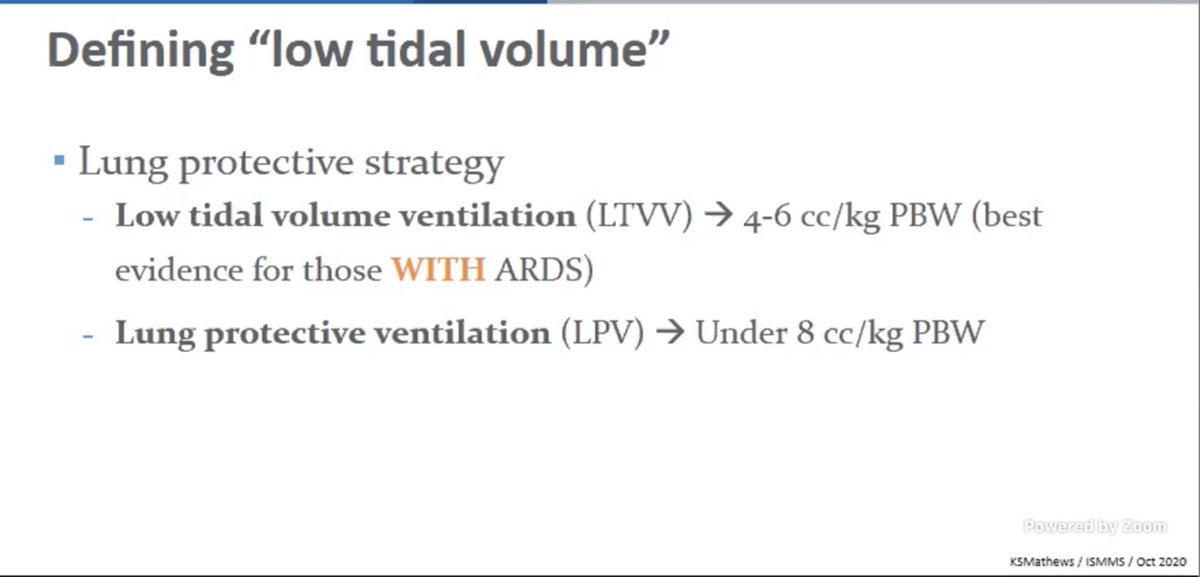
I should clarify. She's advocating for Lung Protective Settings (<= 66 cc/kg) across the board and LTVV (<= 6 cc/kg) for critically ill esp with ARDS!
#CHEST2020 #CHESTCritCare
#CHEST2020 #CHESTCritCare
And now @roeckler will argue that "One size does not fit all" when it comes to lung-protective ventilation across the board.
#CHEST2020
"Are we still talking about Vt in 2020?"
#CHEST2020
"Are we still talking about Vt in 2020?"
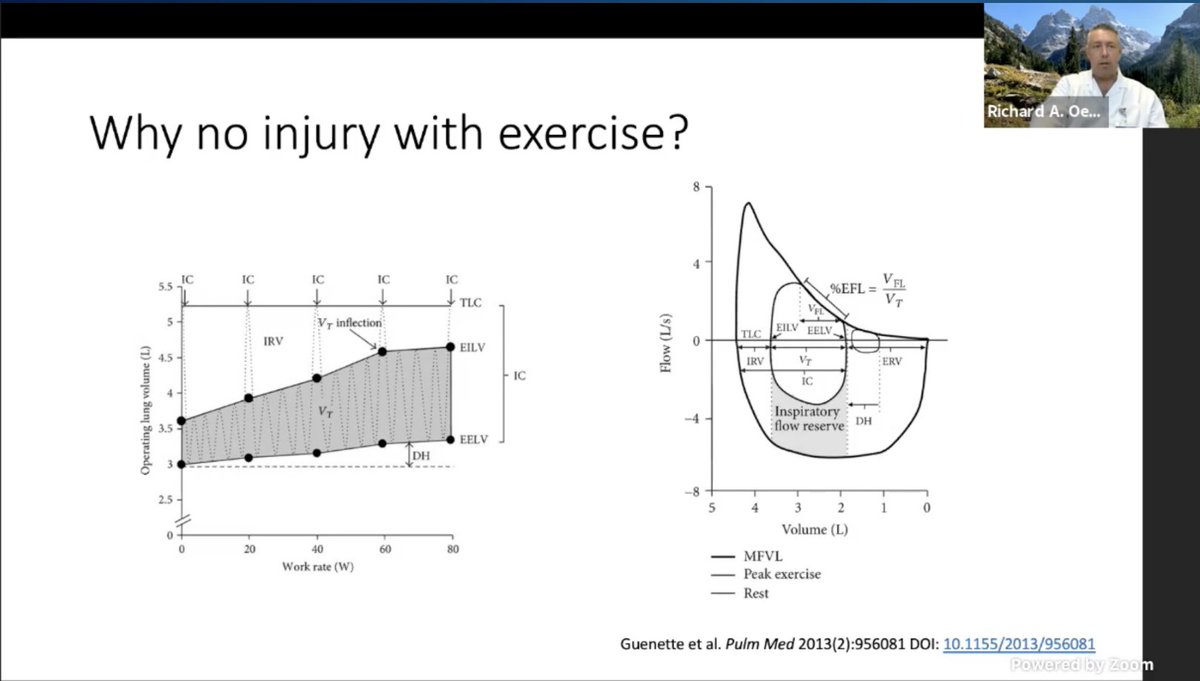
.@roeckler: Is low Vt just the normal Vt. Not sure why LUNG-SAFE and other studies are even looking at the "high" Vt.
Remind us: Atheletes don't get injured with taking huge volumes so clearly it's the local milieu contributing to the injury.

Remind us: Atheletes don't get injured with taking huge volumes so clearly it's the local milieu contributing to the injury.
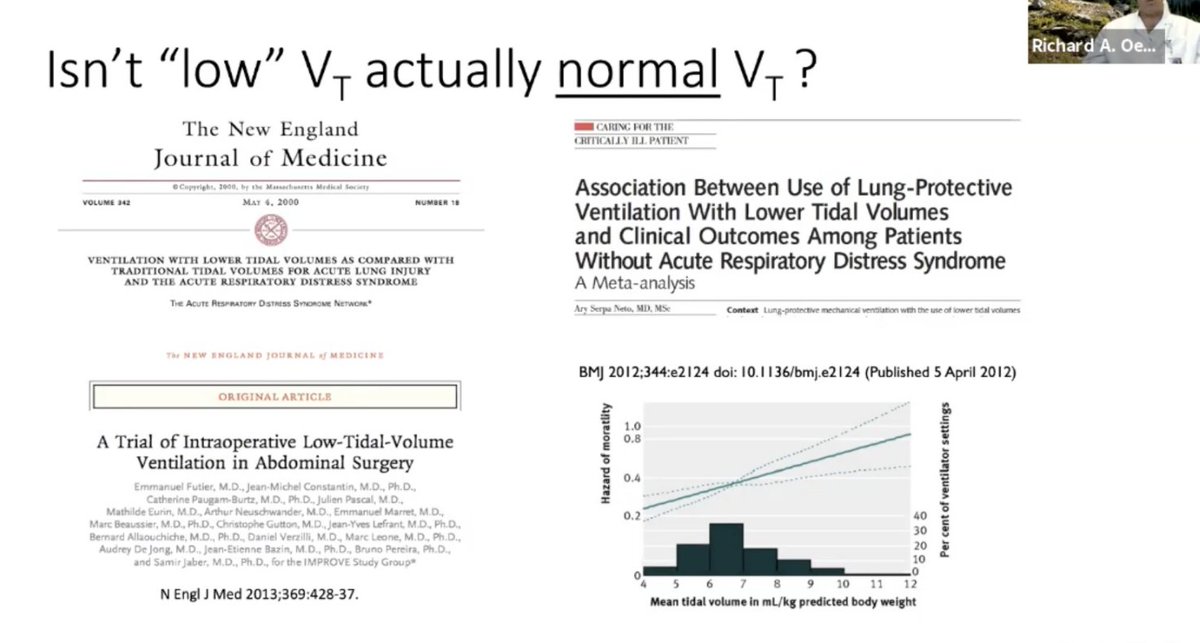
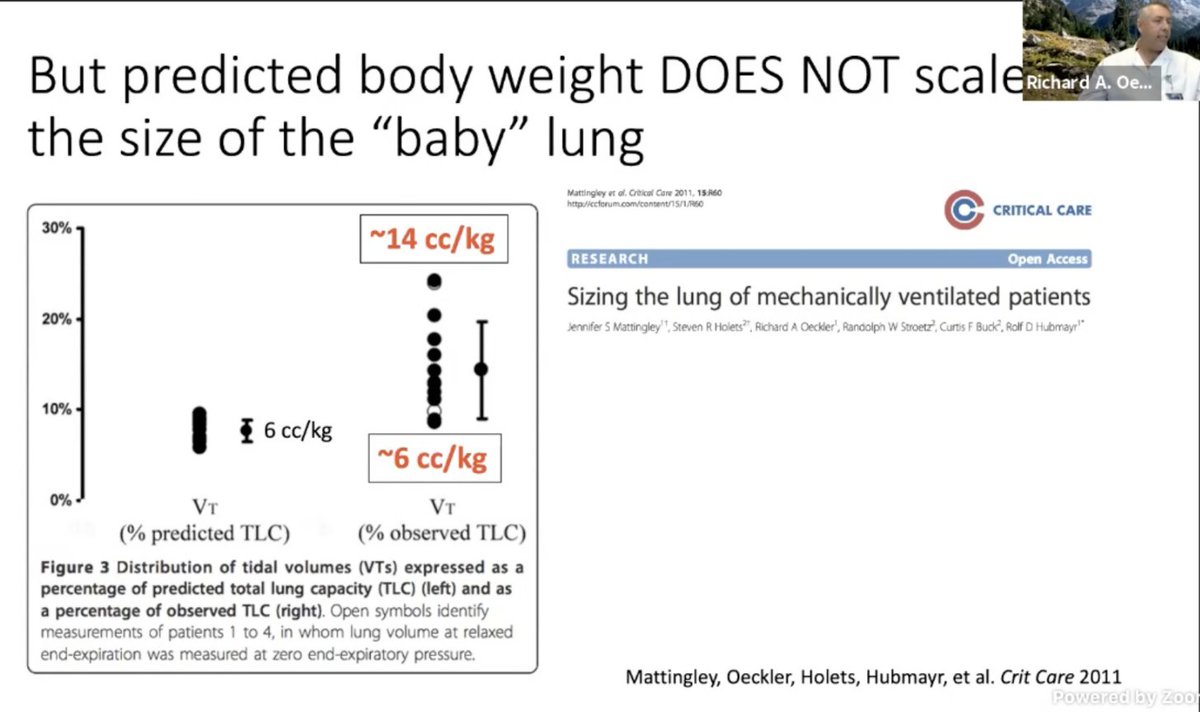
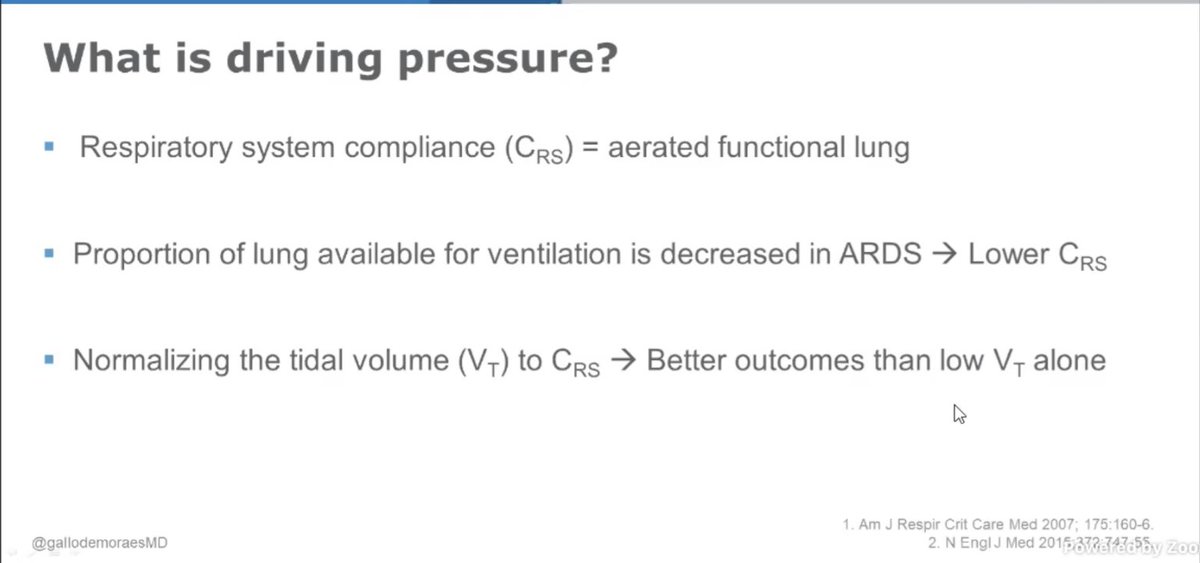
.@roeckler: PBW does not scale to the size of the baby lung in their study. So the Vt does not help across various individuals.
He is advocating for scaling the Vt to the lung compliance of the baby lung instead, not the PBW/IBW.
#CHEST2020

He is advocating for scaling the Vt to the lung compliance of the baby lung instead, not the PBW/IBW.
#CHEST2020
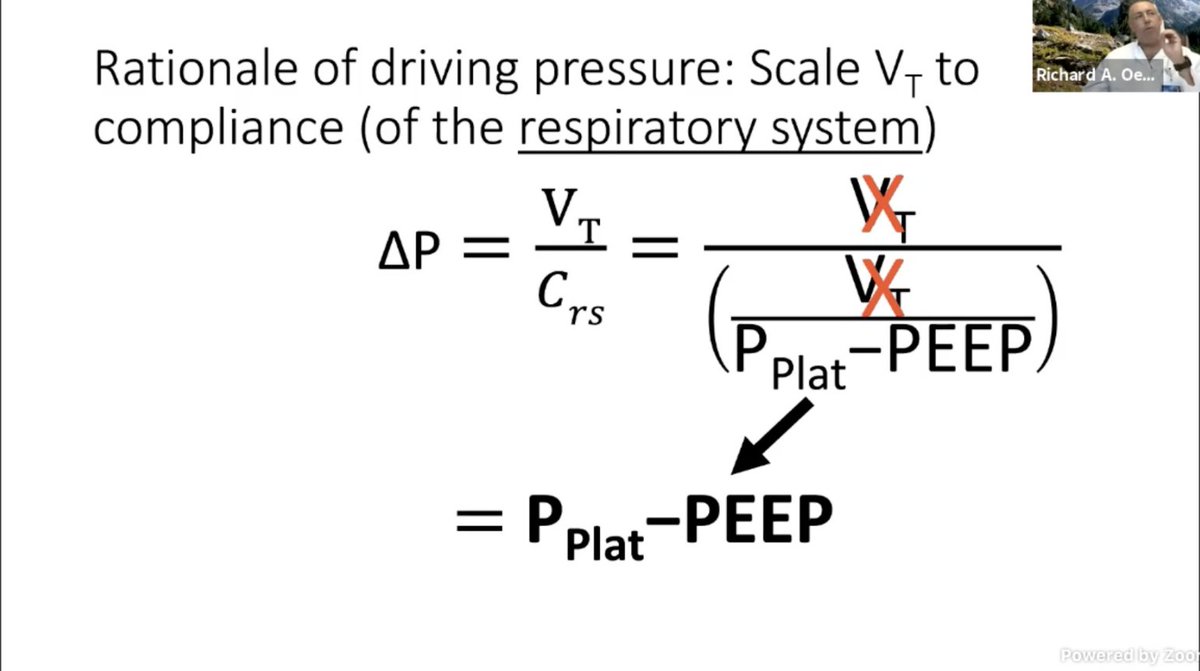
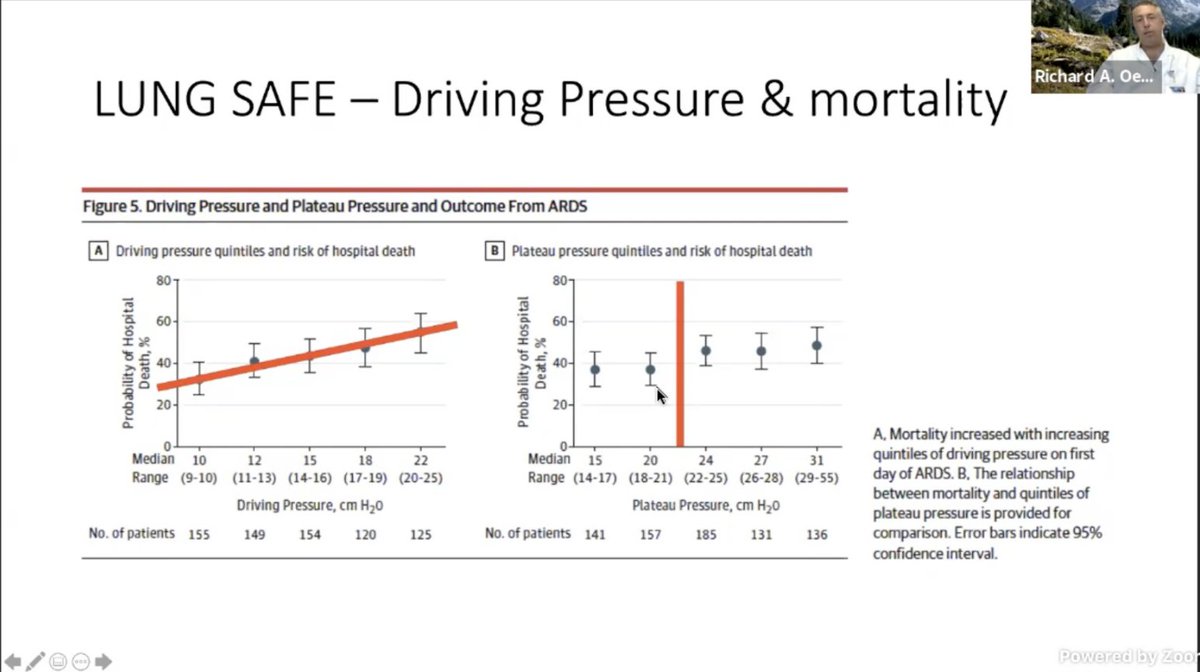
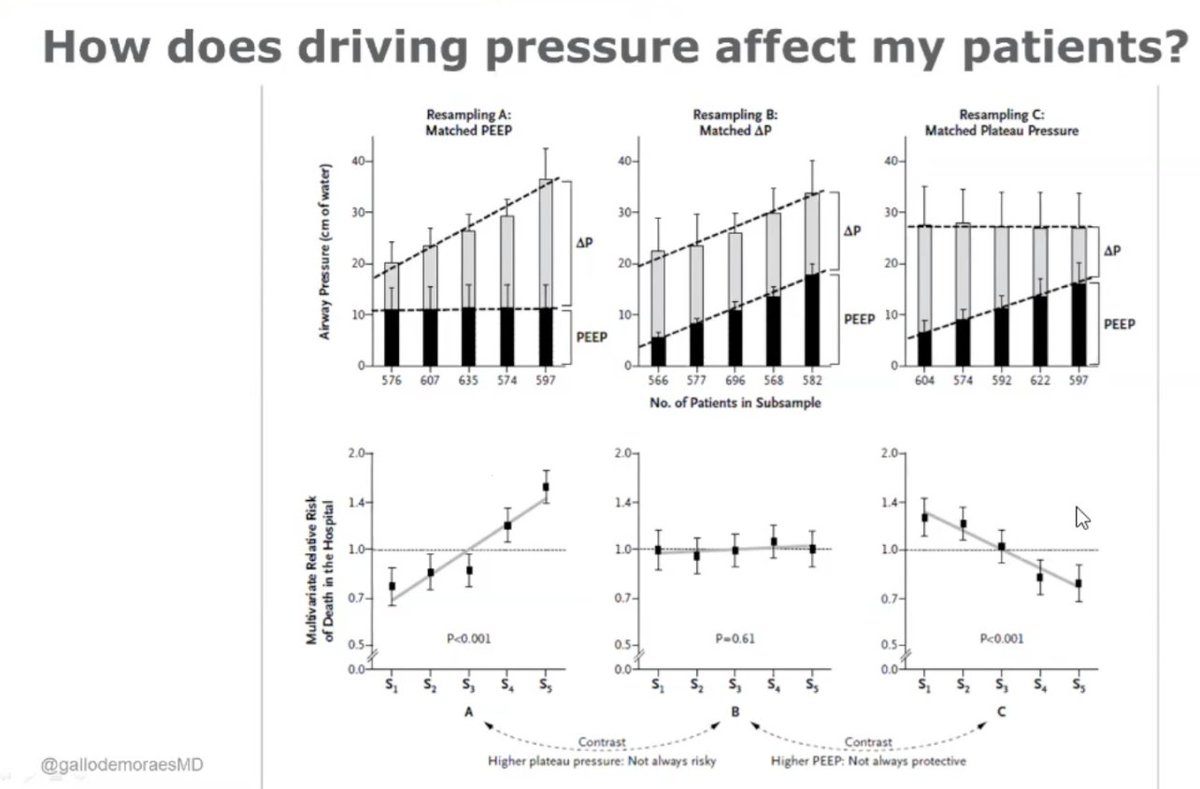
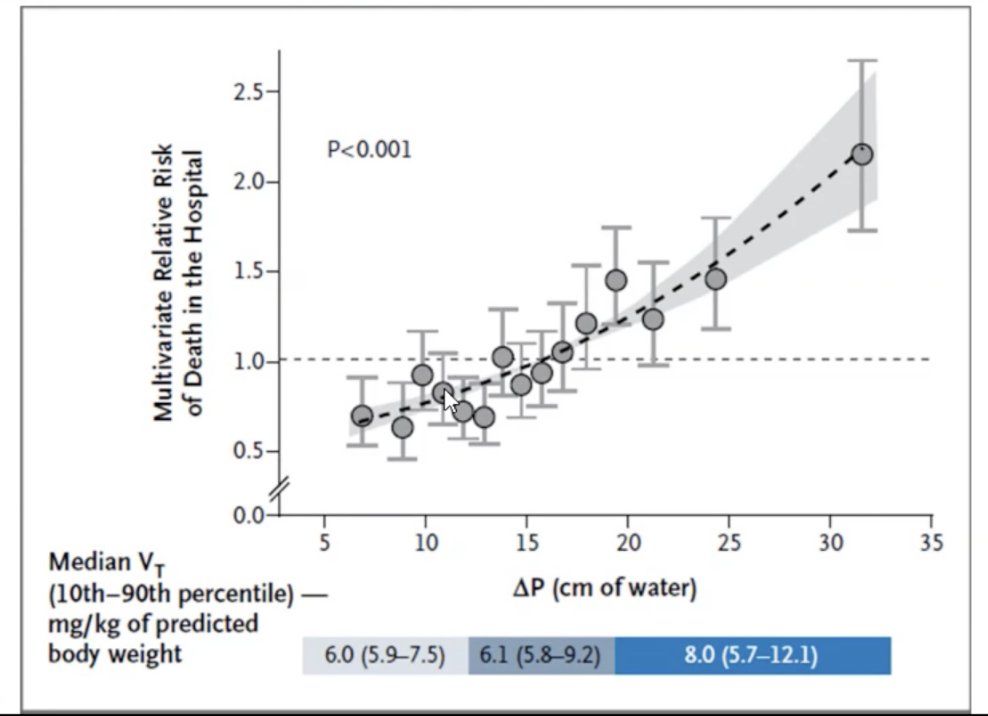
.@roeckler:
Quotes supplement of the Amato paper.
No improvement in mortality with decreasing Vt but look at that improvement with optimizing DP.
#CHEST2020
Quotes supplement of the Amato paper.
No improvement in mortality with decreasing Vt but look at that improvement with optimizing DP.
#CHEST2020
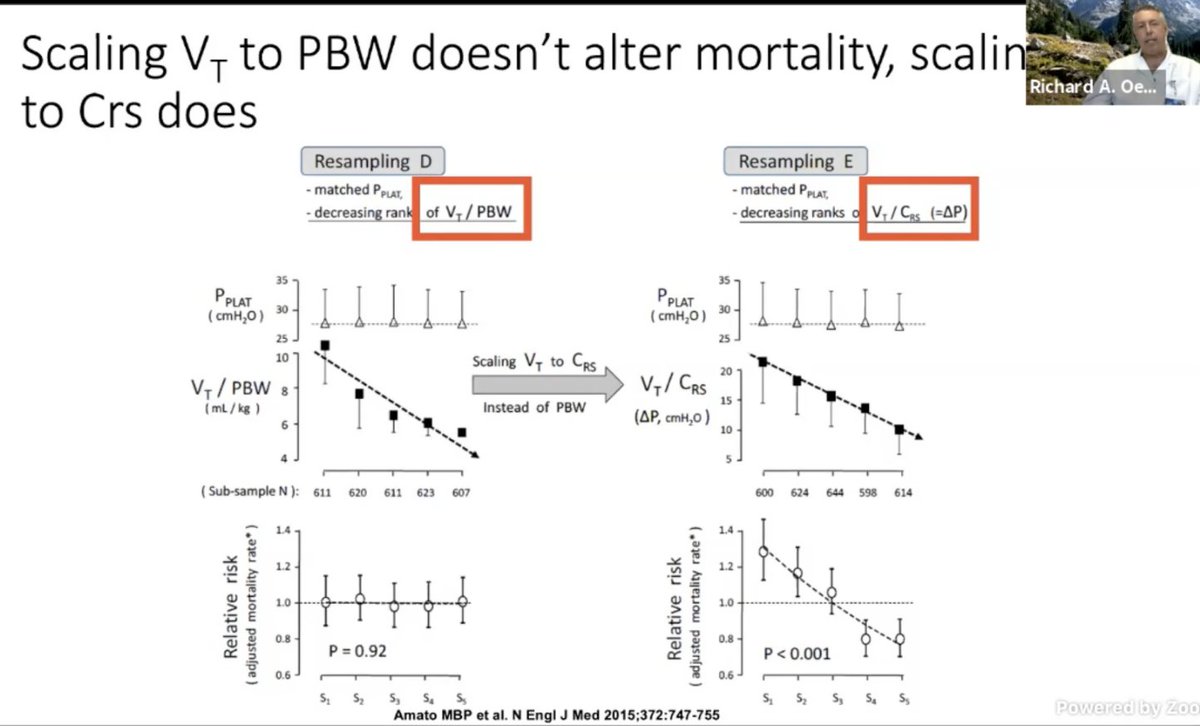
In LUNG-SAFE: Looks like driving DP and Pplat down is where the answer is. However, at some point, oxygenation and ventilation becomes mutually exclusive in resp failure esp with that increased dead space. (esp in #COVID19)
So need to find balance between LTV and DP.
#CHEST2020
So need to find balance between LTV and DP.
#CHEST2020
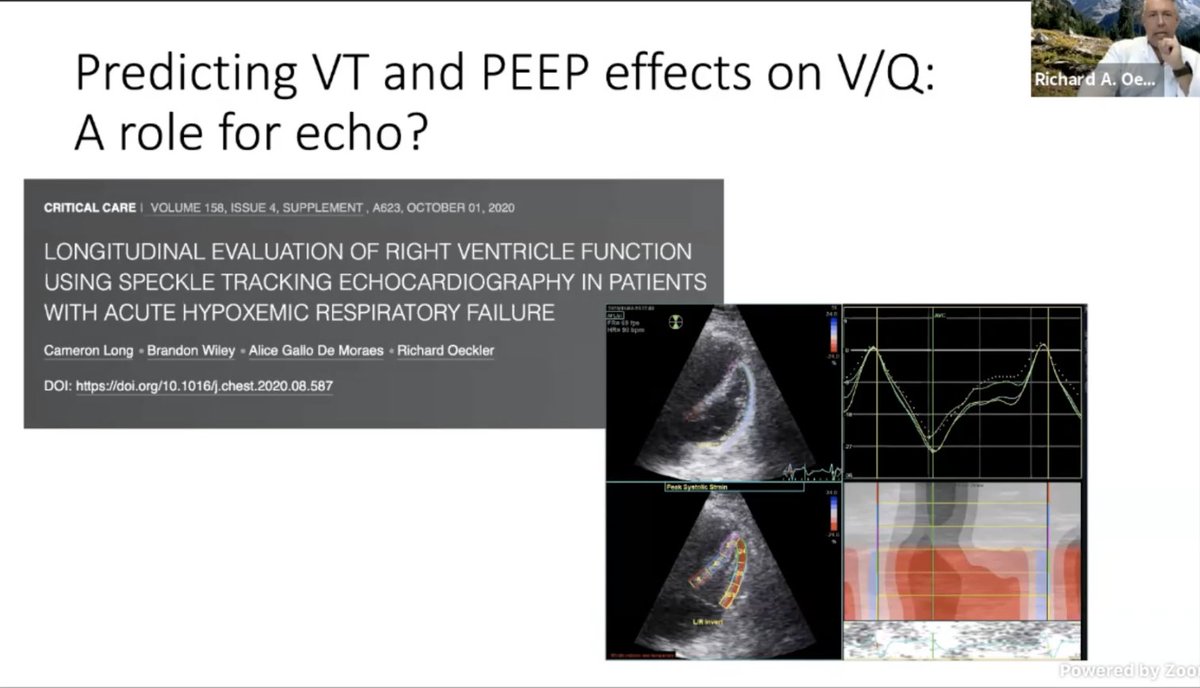
.@roeckler @GallodeMoraesMD and their trainees presented at #CHEST2020: The relationship of lung volume to pulm vascular resistance. This could explain why there are PEEP "responders" and "non responders". We don't have a great way to assessing PVR continuously
#CHEST2020

#CHEST2020
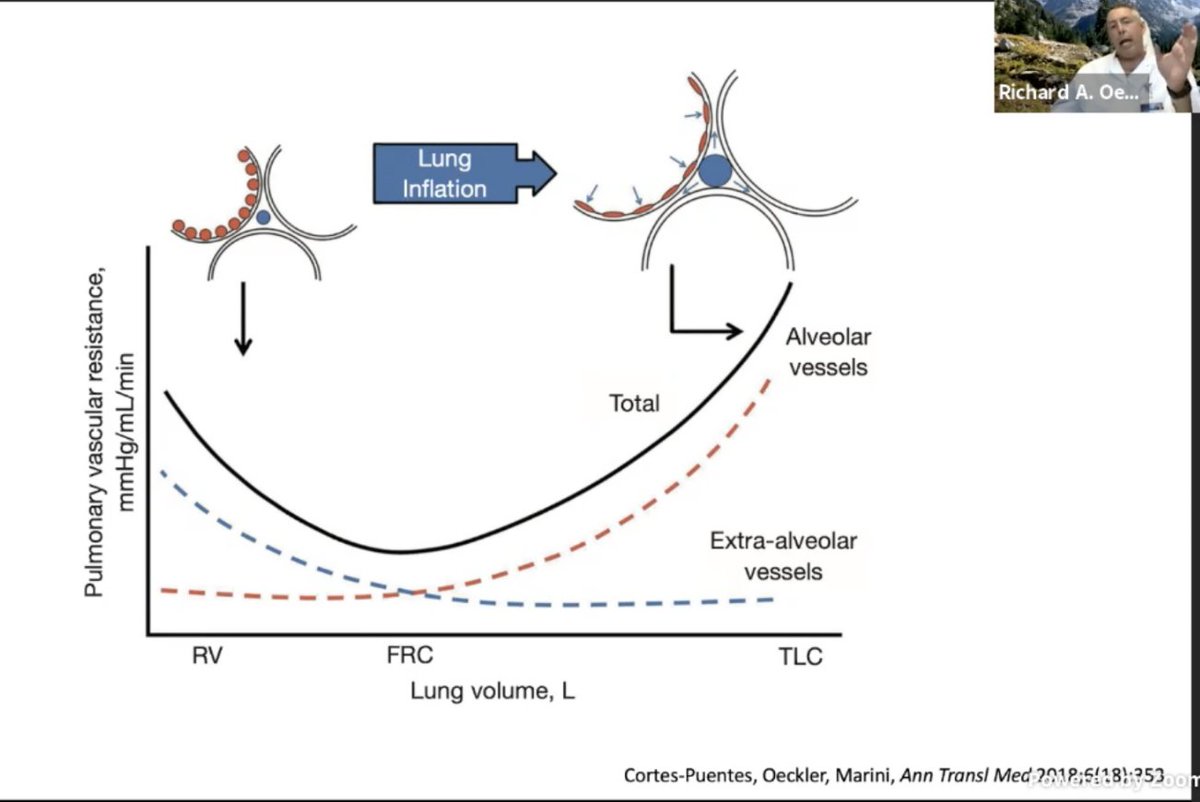

Their poster right here is available to review where they are using speckled tracking and RV #POCUS to get a sense of the PVR at bedside. This might be the missing piece in ARDS care!
.@roeckler out. #CHEST2020
.@roeckler out. #CHEST2020
.@GallodeMoraesMD: Is up next defending LOW DP!
Lung injury is not homogenous.
So even "lung protective injury" can aggravate lung injury.
#CHEST2020
Lung injury is not homogenous.
So even "lung protective injury" can aggravate lung injury.
#CHEST2020
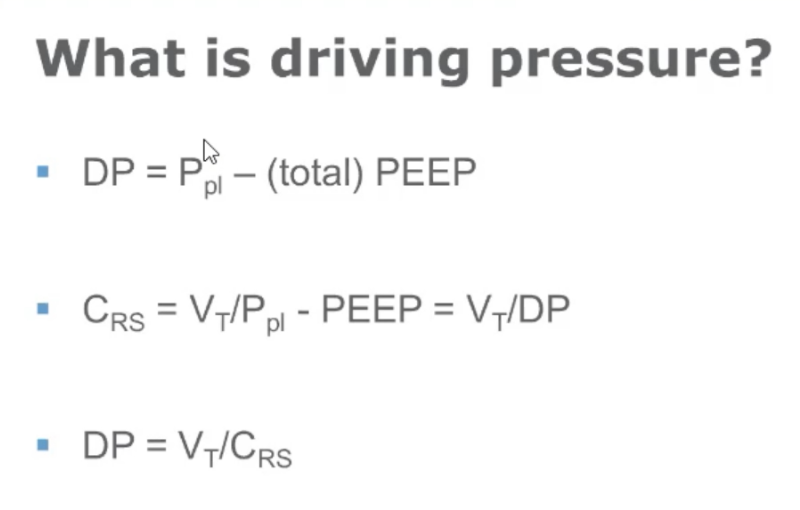
.@GallodeMoraesMD
Amato et al advicated of adapting Vt to compliance for better outcomes.
Question: What is DP.
Tip: Ensure passive patient without auto-PEEP.
#CHEST2020

Amato et al advicated of adapting Vt to compliance for better outcomes.
Question: What is DP.
Tip: Ensure passive patient without auto-PEEP.
#CHEST2020
.@GallodeMoraesMD: Amato's study:
Higher PEEP not always protective
Higher Pplat not always injurious
As long as DP is low.
DP < 15 preferred, < 13 is better!
#CHEST2020

Higher PEEP not always protective
Higher Pplat not always injurious
As long as DP is low.
DP < 15 preferred, < 13 is better!
#CHEST2020
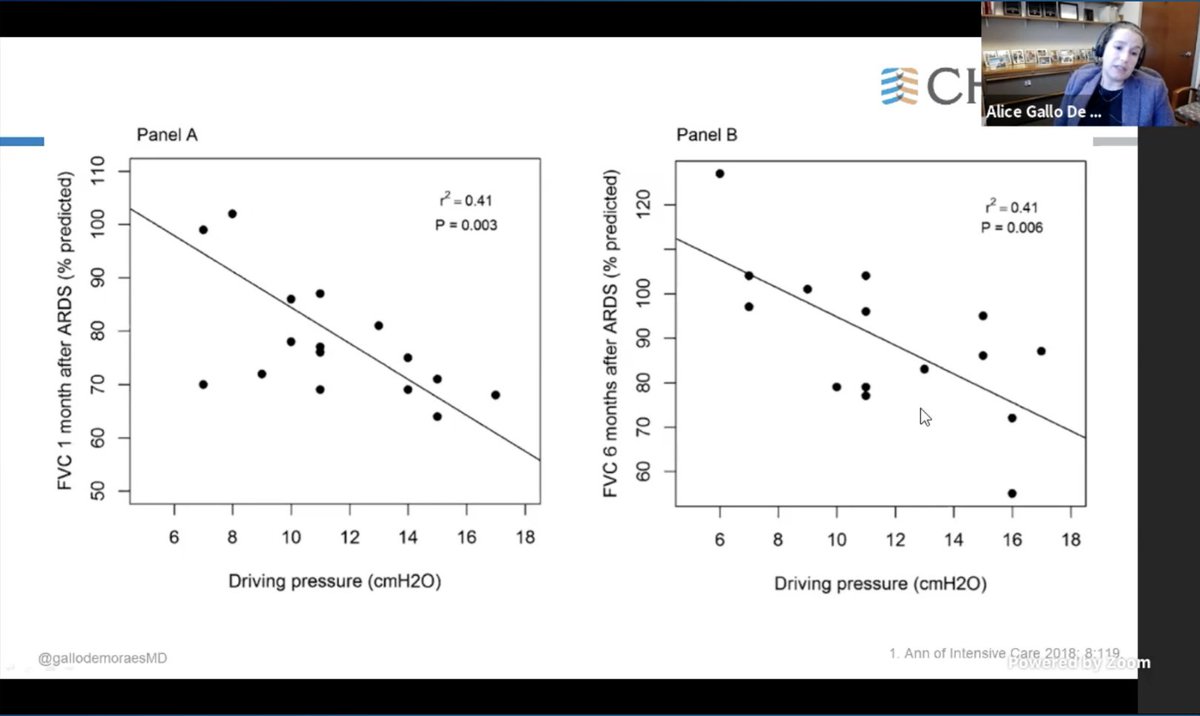
.@GallodeMoraesMD
In pts that survived ARDS
Patients with LOW DP, at 1 month post D/C, had more lung function recovery as well as of density on imaging compared to those where DP were high.
annndddd mic drop Dr. Gallo.
#CHEST2020

In pts that survived ARDS
Patients with LOW DP, at 1 month post D/C, had more lung function recovery as well as of density on imaging compared to those where DP were high.
annndddd mic drop Dr. Gallo.
#CHEST2020

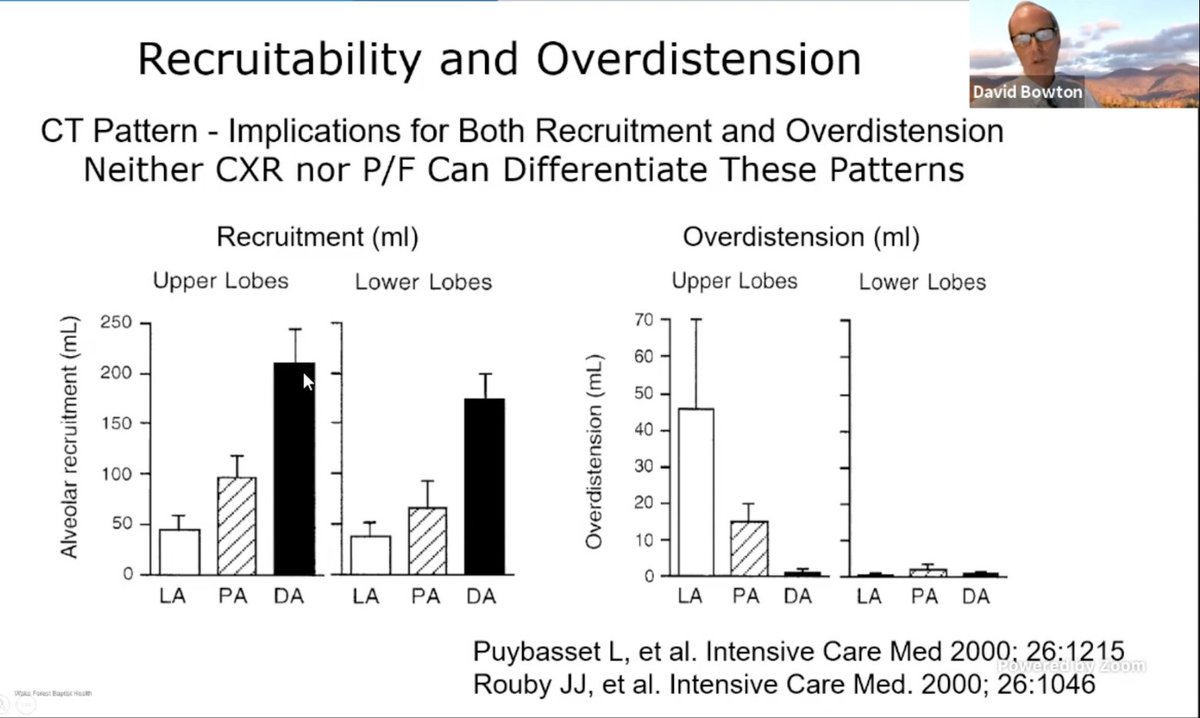
.@DavidBowton will now rebut the idea of LOW DP pressures being beneficial.
CXR and P/F can't distinguish involvement of lungs in #ARDS. So balancing recruitment and overinflation HARD to do without CT scans. Though EIT could change this at bedside.
#CHEST2020
CXR and P/F can't distinguish involvement of lungs in #ARDS. So balancing recruitment and overinflation HARD to do without CT scans. Though EIT could change this at bedside.
#CHEST2020
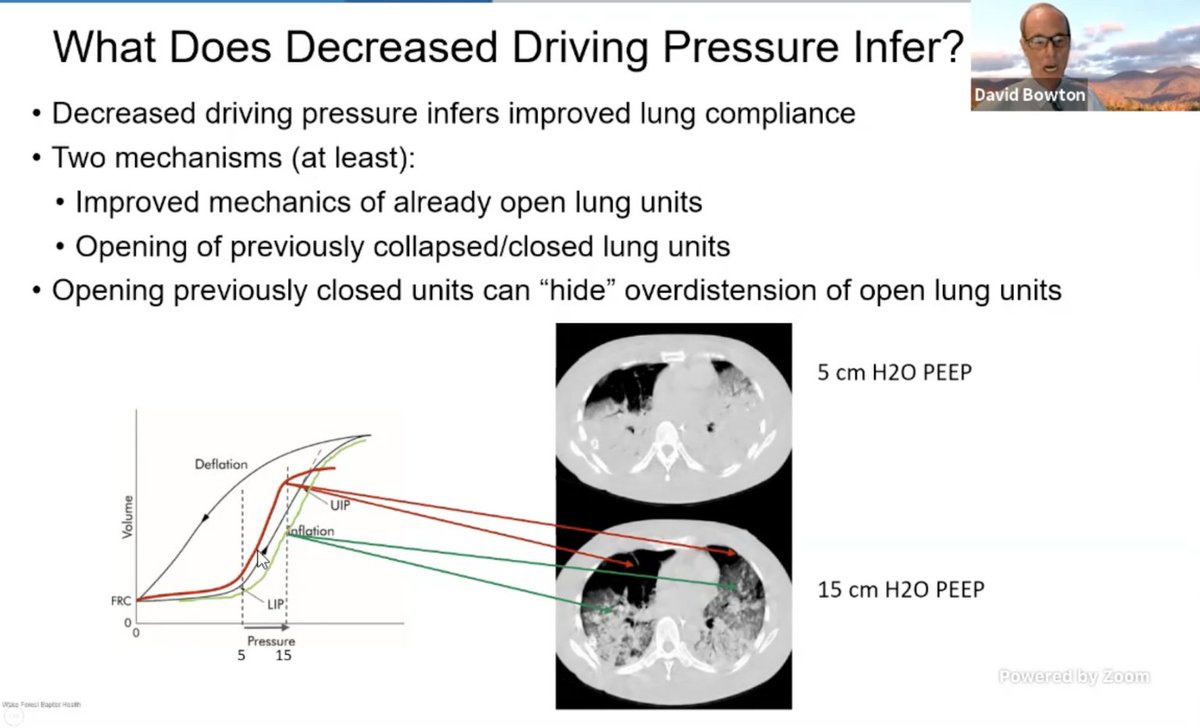
.@DavidBowton: opening up new lung units can hide overdistention of open lung units. However, per studies quoted by Dr. Gallo, DP IS good. But what's the "right" DP?
Dr. Bowton shares that there are no good prospective trials to find the "cutoffs" for benefit.
#CHEST2020

Dr. Bowton shares that there are no good prospective trials to find the "cutoffs" for benefit.
#CHEST2020
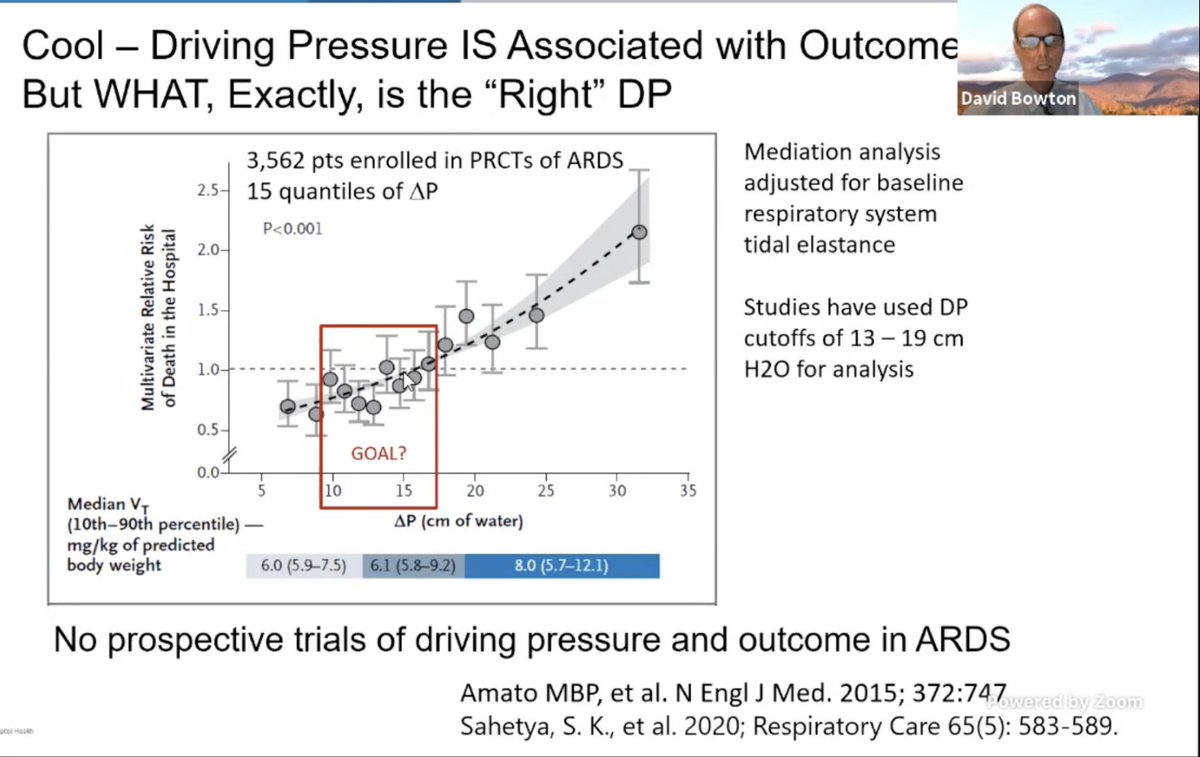
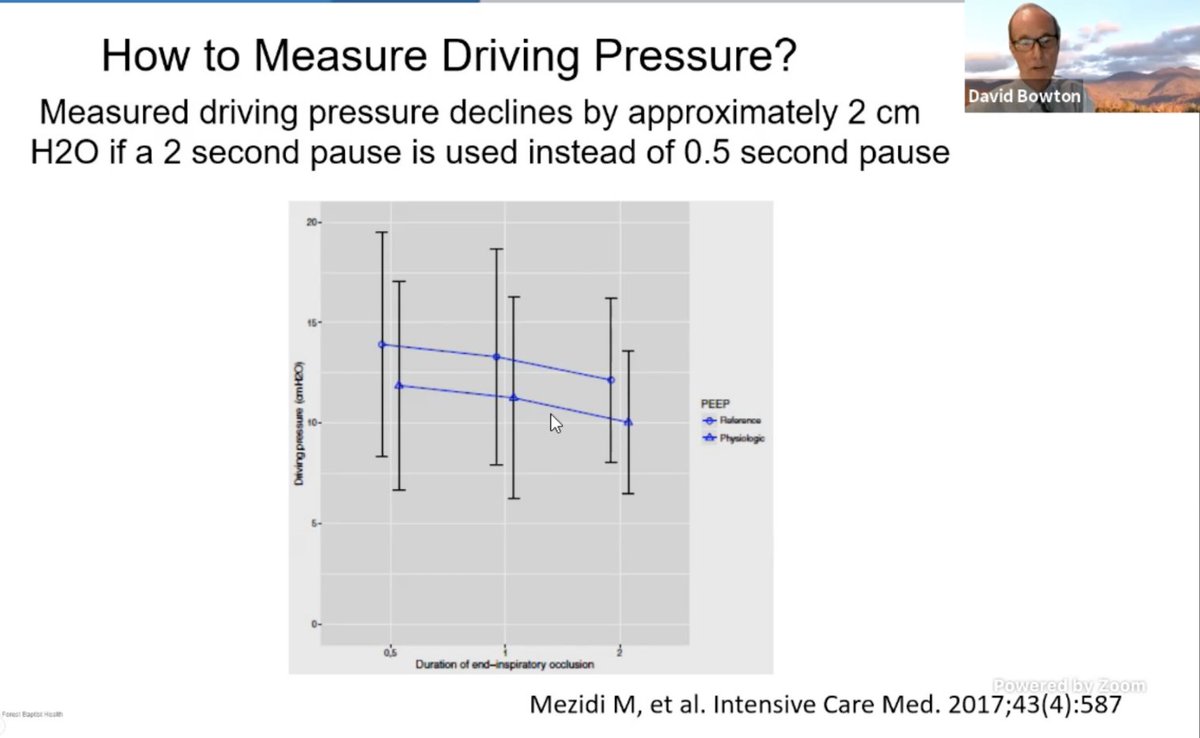
.@DavidBowton:
How we measure DP also needs to be standardized. Changing insp pause from 0.5 to 2 sec could change DP by 2 - 3 CMW and that is a big deal when making clinical changes to vent.
#CHEST2020
How we measure DP also needs to be standardized. Changing insp pause from 0.5 to 2 sec could change DP by 2 - 3 CMW and that is a big deal when making clinical changes to vent.
#CHEST2020
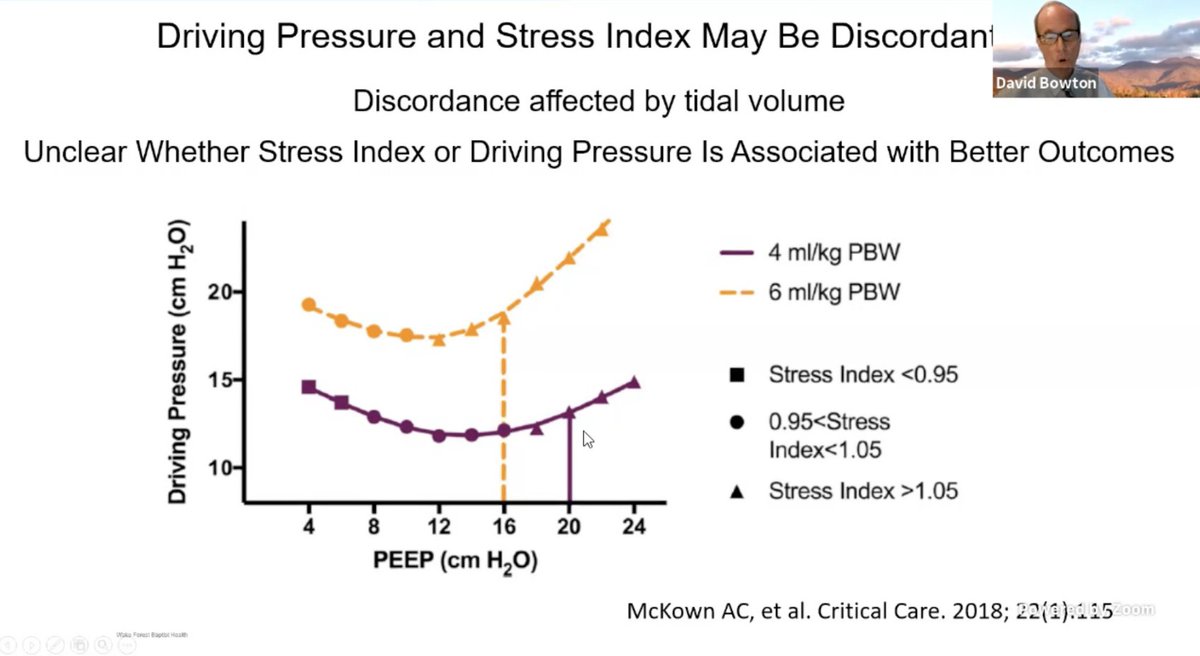
.@DavidBowton Stress Index and DP can diverge at different Tidal Volumes. And how do we reconcile these differences.
Dr. B also reminds us there are other factors that impact TPP and that changes DP, then hard to interpret.
#CHEST2020

Dr. B also reminds us there are other factors that impact TPP and that changes DP, then hard to interpret.
#CHEST2020
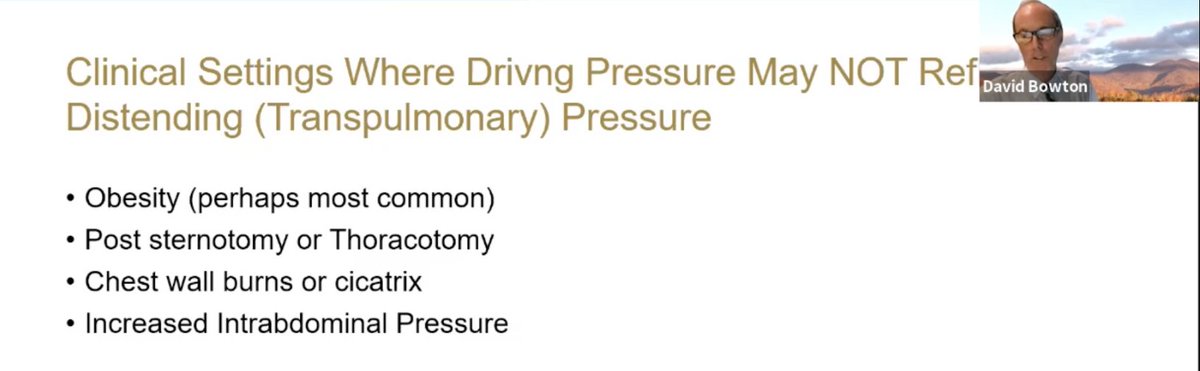
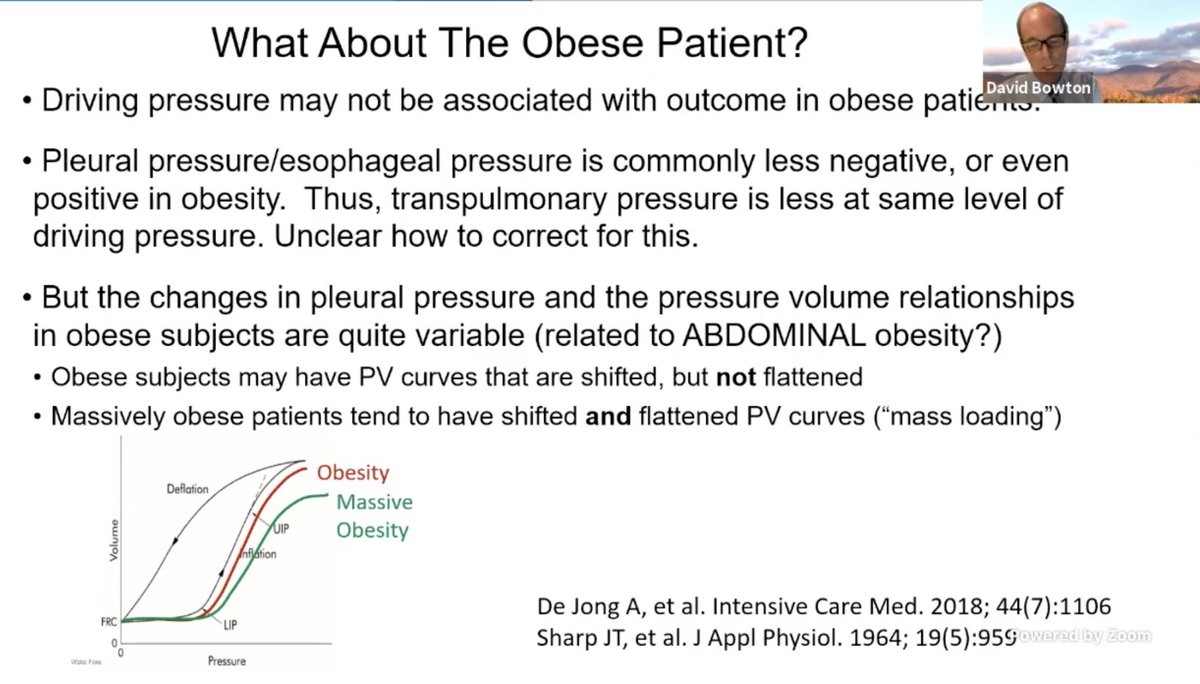
@DavidBowton: Esp in obese patients (esp abdominal obesity), DP not associated with improved outcomes, likely due to miscalculation of the DP. So the DP < 15 can't be extrapolated across the board.
#CHEST2020

#CHEST2020
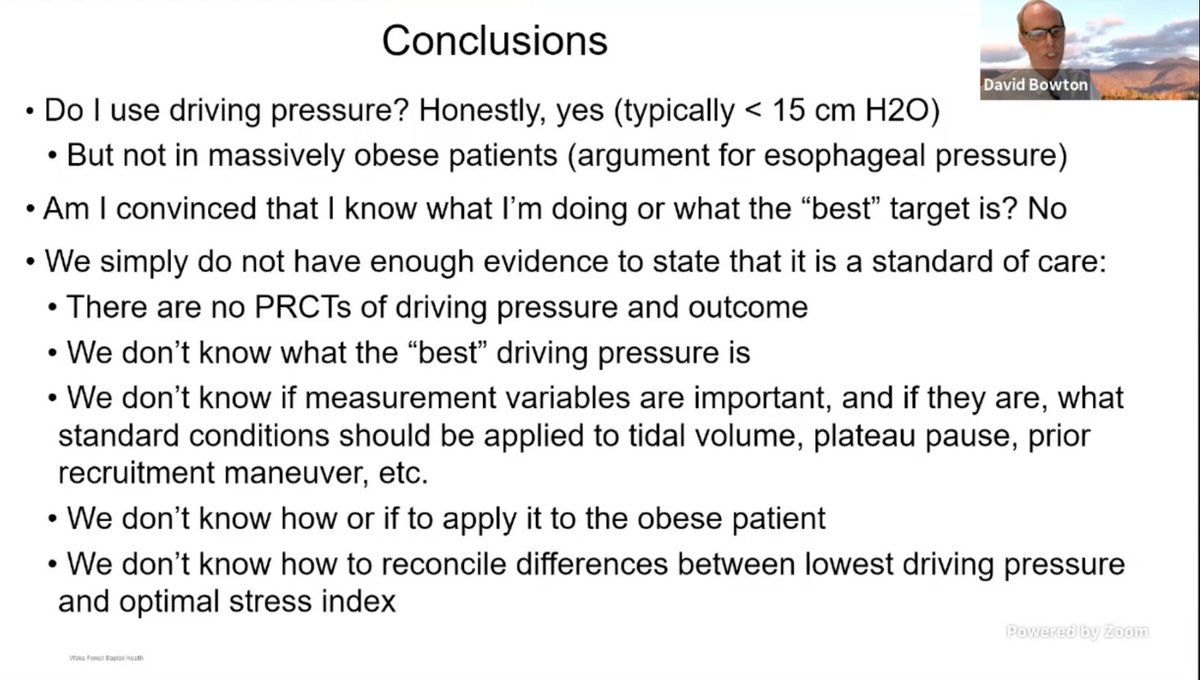
So basically @DavidBowton agrees with @GallodeMoraesMD that DP < 15 is likely beneficial but reminds us to keep caveats in mind:
- divergence with stress index
- special patient populations
OK folks, heading to my own session now. @virenkaul out!
- divergence with stress index
- special patient populations
OK folks, heading to my own session now. @virenkaul out!
Link to the The Clinical Effect of an Early, Protocolized Approach to Mechanical Ventilation for Severe and Refractory Hypoxemia
Mentioned in the session by Dr. Oeckler
rc.rcjournal.com/content/early/…
Mentioned in the session by Dr. Oeckler
rc.rcjournal.com/content/early/…
• • •
Missing some Tweet in this thread? You can try to
force a refresh