Fluid overload is bad news for patients:
1. Causes AKI
2. Prevents organ and patient recovery
3. Increases mortality
Ill share some of the data masterfully presented by @criticalbeansmd today at #KidneyWk starting with the take home points, in case this is the only tweet you see
1. Causes AKI
2. Prevents organ and patient recovery
3. Increases mortality
Ill share some of the data masterfully presented by @criticalbeansmd today at #KidneyWk starting with the take home points, in case this is the only tweet you see

Fluid Overload is very common, is all over the place and it has several definitios.
Patients accumulate weight at least for the first 7 days if the ICU doesn’t have some sort of FLUID STEWARDSHIP program in place. Remember fluids are drugs #KidneyWk.

Patients accumulate weight at least for the first 7 days if the ICU doesn’t have some sort of FLUID STEWARDSHIP program in place. Remember fluids are drugs #KidneyWk.


There is no single situation in which Fluid overload is beneficial for patients. On the contrary. It is bad in every situation, doesnt matter how we slice or present the data. Liberal fluid strategies are always worse #KidneyWk 



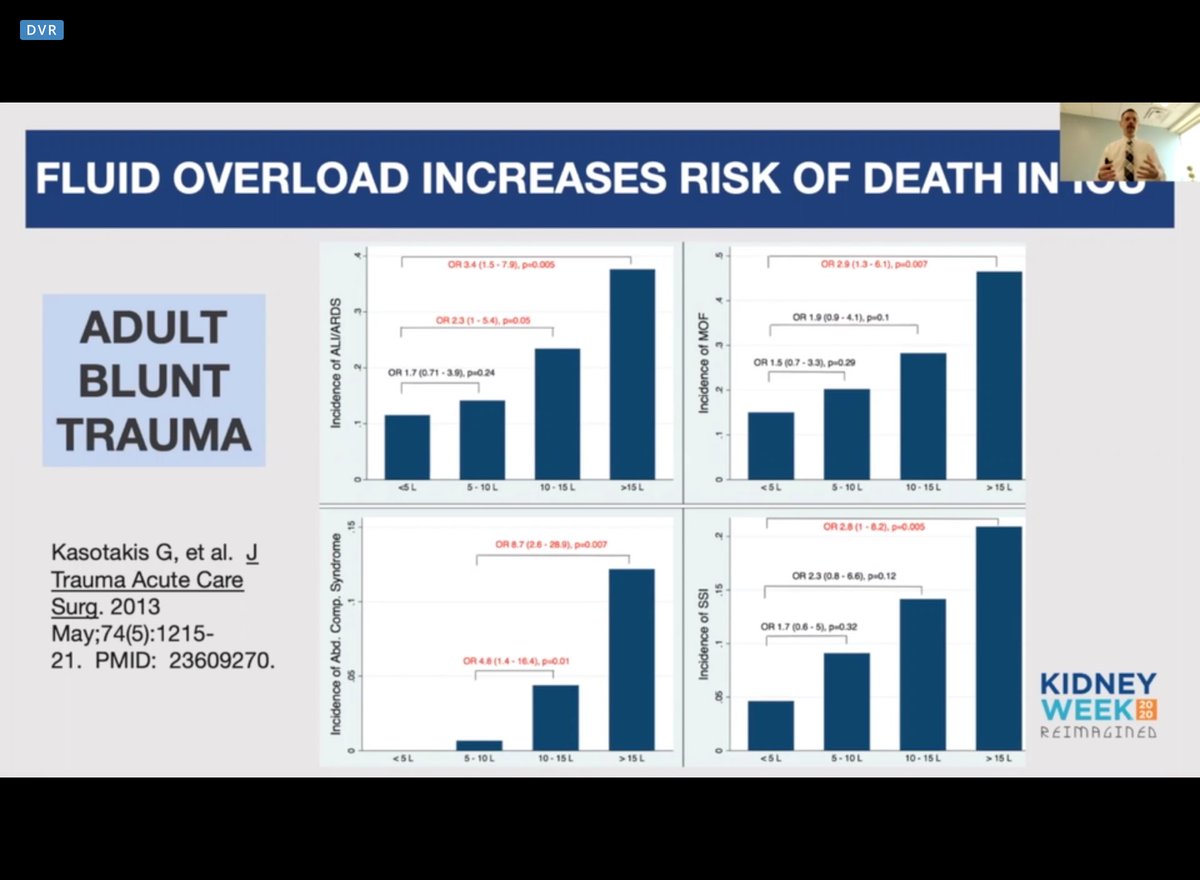



New meatanalisis on fluid overload of hundreds of papers. Look at the RR for mortality!!!! #kidneywk 

In #AKI Fluid Overload is terrible!!! I have some news for you, Kidneys dont like extra fluid either. Say no to “permissive hypervolemia” Waiting for FO to be > 10% increases the risk of mortality by 2 fold. More FO and more time being FO, the higher risk of death. #KidneyWk 







Several studies have shown that fluid overload dont correlate with fluid overload. However this remains an association. So, which are the potential mechanisms?
Some important concepts:
1. BP is not equal to flow
2. Our goal is organ perfussion
#KidneyWk


Some important concepts:
1. BP is not equal to flow
2. Our goal is organ perfussion
#KidneyWk



Fluid goes everywhere causing organ disfunction (gut, liver, skkin, brain, lung, heat, you name it) and no, we cannot infinite “third space”. Venous congestion directly opposes perfusion by impairing capillary drainage. #Kidneywk 







Vol. overload causes all sorts of badness in the beans. I like to summarize them as: Nephrosarca. The picture is consistent with hemodynamic (formerly prerrenal) AKI. It can be misinterpreted as “extravascular volume expanded but intravascular volume depleted” 😵 #KidneyWk 



Intraabdominal hypertension also causes organ disfunction, mainly in the kidneys worsening the whole picture. Half of the patients in ICU have IA hypertension and 20% abdominal compartamental syndrome #Kidneywk 





Organ recovery requires organ perfussion. We need to decongest these patients. The FACTT trial showe us that it feasible to manage patient with only the amount of fluid that is necessary with better outcomes. No more “swell to get well” #Kidneywk 





“Pee to be free (from the ICU)” Truer words have never been spoken. The best approach to fluid managment has not being elucidated. I would argue that prevention is the way to go. Knowing is half the battle. #Kidneywk 



When is the best time for evacuating the extra fluid or how aggressive should we do it? We dont know... yet. Prevention is the first step. FLUID STEWARDSHIP people. Use your vasopressors early and wisely. Yes you can use them with diuretics #diuresisJedi #Kidneywk 







Conclusion slide. Amazing talk. #Kidneywk 

• • •
Missing some Tweet in this thread? You can try to
force a refresh