Covid (@UCSF) Chronicles, Day 220
1/ Yesterday was @UCSF Medicine Grand Rounds– we covered the 3rd wave (w/ particular focus on situation in Wisconsin) and how to assess and manage risk in Covid. The conference (70 min) is available here: tinyurl.com/y2to6y9y Worth watching.
1/ Yesterday was @UCSF Medicine Grand Rounds– we covered the 3rd wave (w/ particular focus on situation in Wisconsin) and how to assess and manage risk in Covid. The conference (70 min) is available here: tinyurl.com/y2to6y9y Worth watching.
2/ @ 5:00: First, an update by George Rutherford on the current surge. The U.S. is now at >60K cases/d. This map, from @nytimes, shows that while biggest surge is in the Midwest, unlike surges 1 and 2 this is really a national surge, with only a few exceptions (one of them CA). 

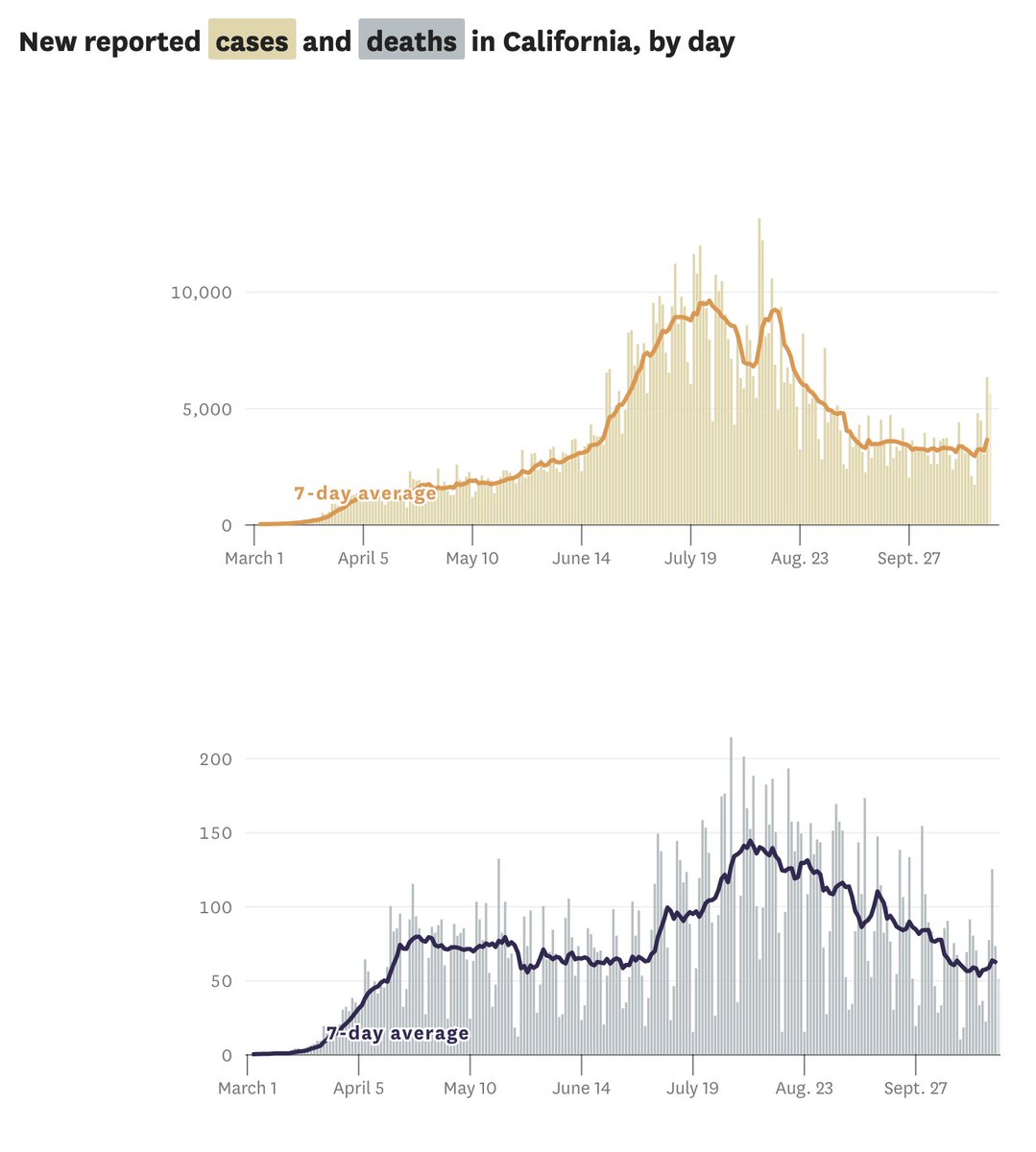
3/ @ 7:30: In California, “no evidence of a 3rd wave…yet.” “I have a feeling that we’re teetering at the precipice, and we need to be absolutely positively clear that we’re doing everything we can to avoid infection.” 
4/ @ 9:30: San Francisco continues to do very well, with R-effective estimate of 0.94. George makes point that the Re is an average across a population, which hides the fact that there are some people that don’t spread at all, while others are super-spreaders. 

5/ @ 10:30: Why is CA doing well? Slide shows various factors, including more use of masks, slow & steady reopening, control of institutional outbreaks, & mature contact tracing system. Maybe some contribution of weather, compared w/ other areas where folks are now forced inside. 

6/ @ 11:40: Compelling graph of states, with frequency of mask usage on Y axis, vs. Covid case rates on X axis. Rutherford: It's simple – “as mask wearing goes down, case counts go up.” 

7/ @ 13:00: While mortality rates are lower, we’re starting to see an uptick in deaths. Current projection: we’ll have 389K deaths by 2/1/21. If really bad behavior, could be as high as 483K; if everybody wears masks, could be as low as 315K.
Note: deaths in World War II: 405K.
Note: deaths in World War II: 405K.
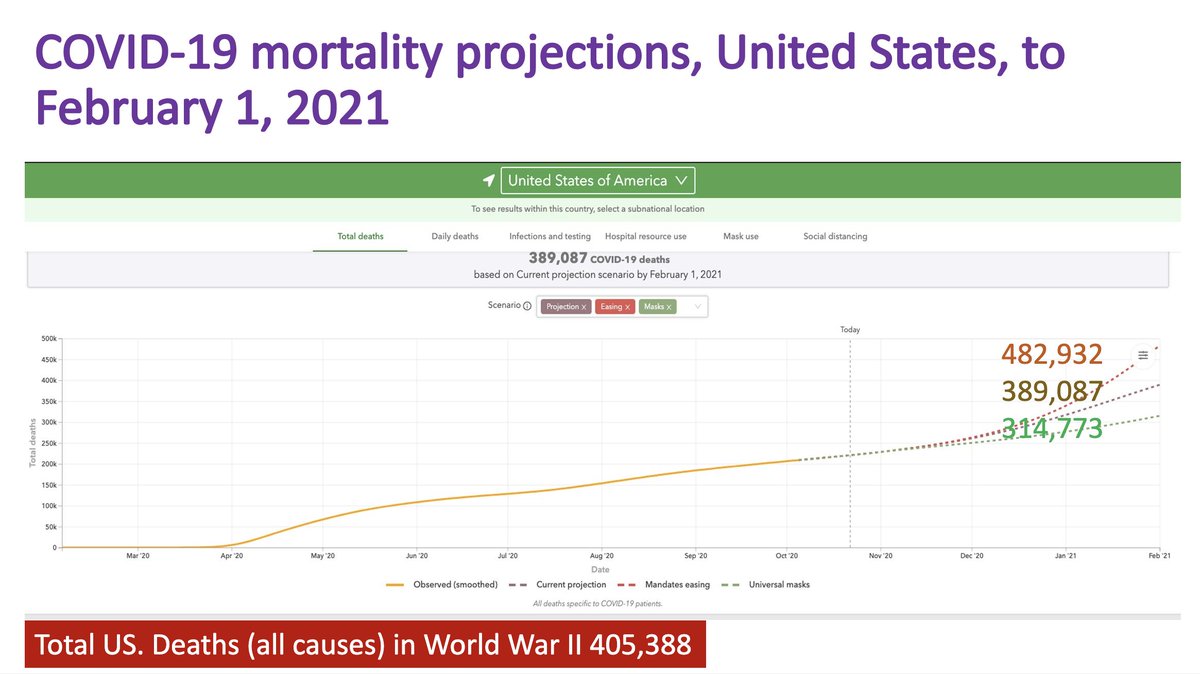
8/ @ 14:00: CDC finds ~300K excess deaths – ~2/3rds directly attributable to Covid, the rest likely related to missed care, miscoded Covid deaths, stress from the pandemic, and more. This excess death number is probably a better reflection of the pandemic’s true toll. 

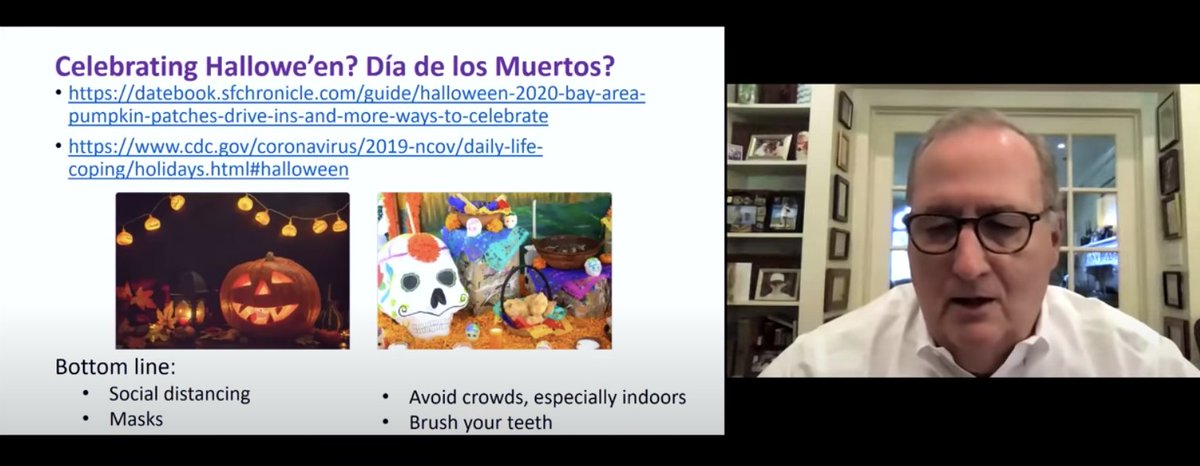
9/ @ 16:00: George’s advice for a safe Halloween? The usual: masks, distancing, etc. "And, when you're done for the evening, brush your teeth."
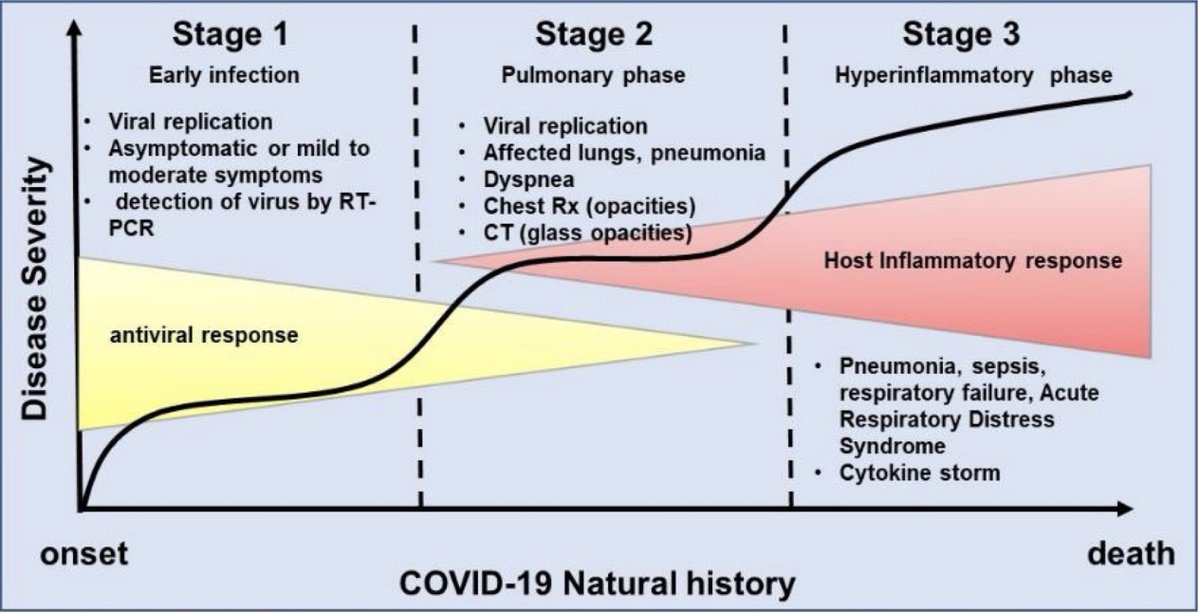
I asked about whether Halloween masks would work for Covid? Answer: “No. Unless you’re playing an ICU worker wearing a PAPR.”
I asked about whether Halloween masks would work for Covid? Answer: “No. Unless you’re playing an ICU worker wearing a PAPR.”
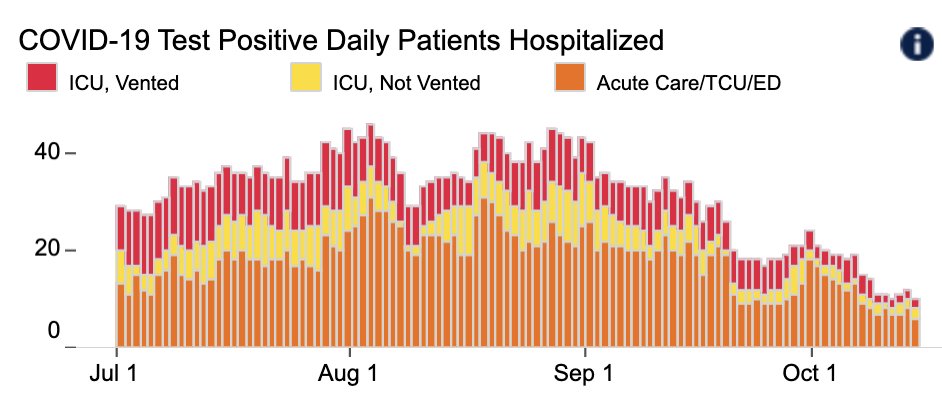
10/ Next up @ 21:30, hospitalist @SheehyAnn and ICU doc Andrew Braun from Univ. Wisconsin. For now, they're seeing only a modest surge, with about ~40 pts (10 in ICU) in a 600-bed hospital, but they’re expecting much more. Northern WI is getting the brunt of it for now. 

11/ @ 23:30: Mask wearing in Madison, WI has been strong, but not true in the rest of the state. A state-wide mask mandate is being challenged in the courts, and it's being ignored in many regions. Ann: “We’ve been begging for a consistent public health mandate.”
12/ @ 25:45: Ann describes what’s happening w/ undergrads. Huge outbreak in early Sept, w/ dorms shut, fraternities/sororities quarantined. They’ve had ~3000 infected students, out of ~45,000 students. Test positivity rate in September was up to 33% (!) among students/faculty.
13/ @ 33:00: we discuss why UW hospital isn't slammed yet. George lists various factors that may be at play: younger pts, masking may be cutting severity. But worry about a lag: w/ young pts being hit first, who will then give it to older people, who will be sick in 1-2 wks. 

14/ @ 36:45, final segment with @JuliaLMarcus, Harvard ID epidemiologist. Our 30 minute conversation is so far reaching and nuanced that I won’t be able to do it justice here. Just a few highlights below. 

15/ March & April: We had a “clear & binary messaging: stay home.” Because it was simple, it was very easy, in a way (though not equitable – some couldn’t stay home). The challenge now is: “how can we do this sustainably" – particularly since we probably have >6 more mths to go.
16/ As we think about the risk of transmission, we’re always making tradeoffs. How do we, as individuals and as a society, make good decisions that we can live with over time? And how do we process not just the potential harms of our choices, but also the benefits?
17/ I asked about my decision to visit my 90 & 84 year old parents in FL. Seeing a loved one, or going to work when you absolutely must – these seem similar to safer-sex education. Abstinence (long term) won't work; key issue is mitigating risk, using a harm-reduction framework.
18/ Lessons from HIV: shaming people for taking risks – “if you cared about people you wouldn’t do this” – doesn’t work well. “We need to try to empathize" – moralistic public health campaigns aren’t effective, in part because they perpetuate stigma & make people go underground.
19/ @ 47:00: I pushed back re: HIV analogy. With Covid, we’re not talking about consensual sex; we’re talking about someone wearing a mask and – if they don't – putting me at risk. Julia agreed: because Covid is much more explosive, we do need mandates in certain settings.
20/ @ 55:00: I asked how we can make 100 incredibly complex & nuanced risk-benefit decisions daily. "It's crazy-making," particularly since we have so little credible guidance from authorities. “It’s like the parents have left the room…unfortunately, we’re on our own,” she said.
21/ We need to factor pandemic fatigue into our thinking – “ ...to focus our efforts on the highest risk settings,” but be a bit more lenient about behaviors that carry lower risks. “People need some ease” – the behaviors we're asking people to do have to be sustainable.
22/ @ 1:03:00: we discuss how things will change if we have partly effective vaccine in '21. Her worry: “I hope we don’t get duped into thinking, ‘oh great, there’s a vaccine, we can throw it all away.’” Even as we (hopefully) move toward "normal," sustainability will remain key.
23/ Fascinating session – again, here: tinyurl.com/y2to6y9y Next Thursday will be regular (non-Covid-focused) @UCSF Medicine Grand Rounds.
Then, Nov 5th: a special post-election Covid grand rounds. @ASlavitt & other special guests will talk Covid & the election. Can’t wait!
Then, Nov 5th: a special post-election Covid grand rounds. @ASlavitt & other special guests will talk Covid & the election. Can’t wait!
• • •
Missing some Tweet in this thread? You can try to
force a refresh