(1/7) Report by Ministry of Health, Israel, showing children more likely to be infected than adults, are mostly asymptomatic, can be superspreaders, that school clusters spread into the community, and that school reopening accelerated the epidemic there.
gov.il/BlobFolder/rep…
gov.il/BlobFolder/rep…
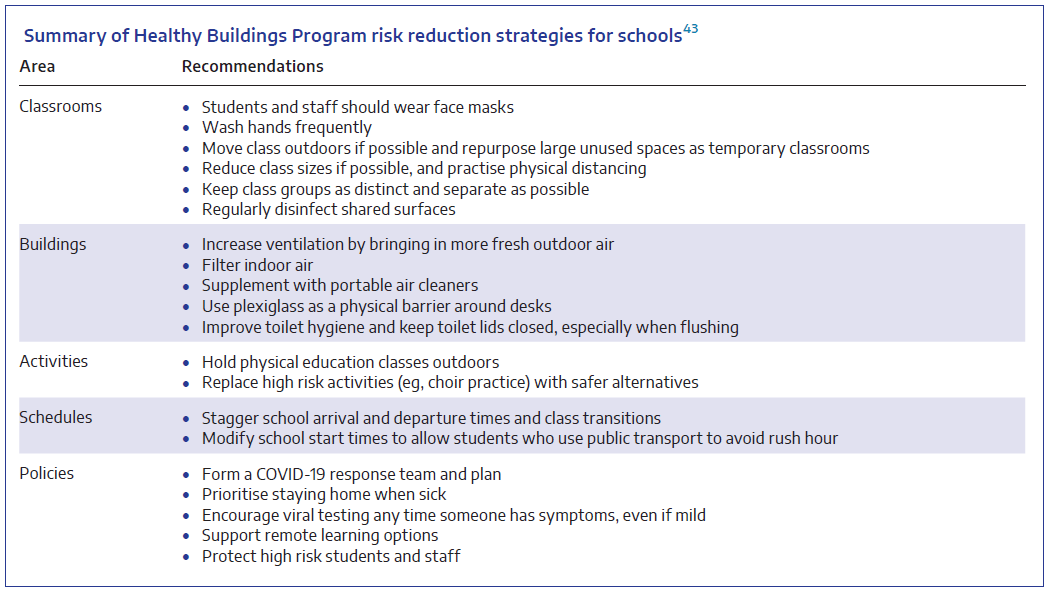
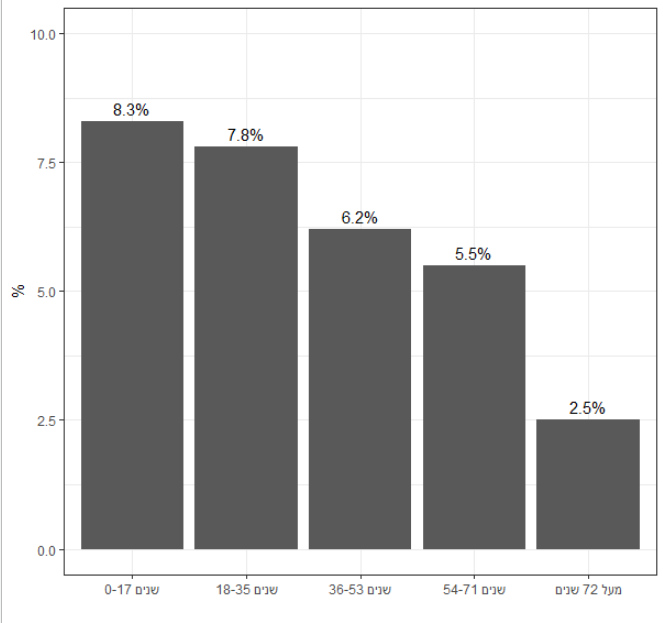
(2/7) As shown in the figure below, children were more likely to test positive than adults (8% vs. 6% of all PCR tests conducted in Israel).
Children were also more likely to test positive for #SARSCoV2 antibodies than adults (7% vs. 2 - 5%).
Children were also more likely to test positive for #SARSCoV2 antibodies than adults (7% vs. 2 - 5%).
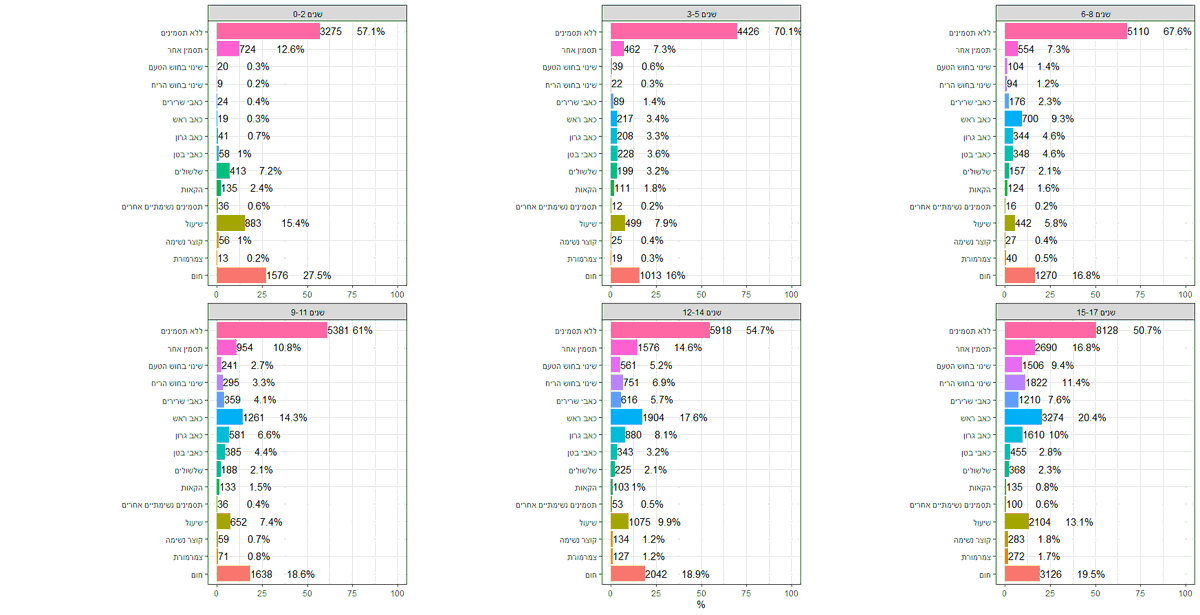
(3/7) Most children with #COVID19 were asymptomatic (51-70%).
As shown in the figure below, children of pre-school & primary school age were more likely to be asymptomatic than older children.
The top (pink) bar indicates the proportion who were asymptomatic in each age group.
As shown in the figure below, children of pre-school & primary school age were more likely to be asymptomatic than older children.
The top (pink) bar indicates the proportion who were asymptomatic in each age group.
(4/7) Across Israel, 350 people who infected at least 10 others were identified. Of these superspreaders, 17 (5%) were children.
Seven children each infected 10 people, three children each infected 12 people, and one child infected 24 people.
Seven children each infected 10 people, three children each infected 12 people, and one child infected 24 people.
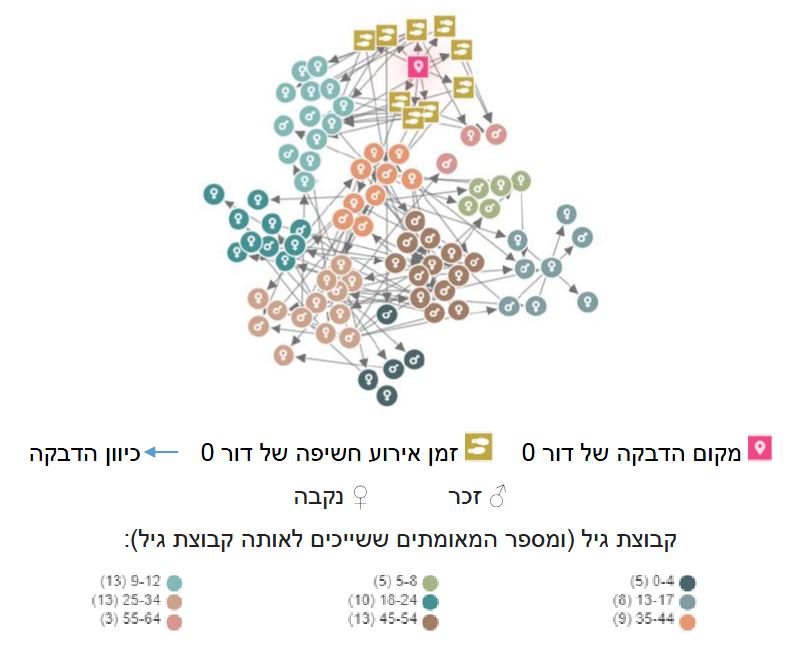
(5/7) Infections in schools ultimately spread into the wider community.
In this figure, a #COVID19 cluster at a primary school is depicted. The cluster initially involved 5 teachers and 20 students, and ultimately affected 79 people.
In this figure, a #COVID19 cluster at a primary school is depicted. The cluster initially involved 5 teachers and 20 students, and ultimately affected 79 people.
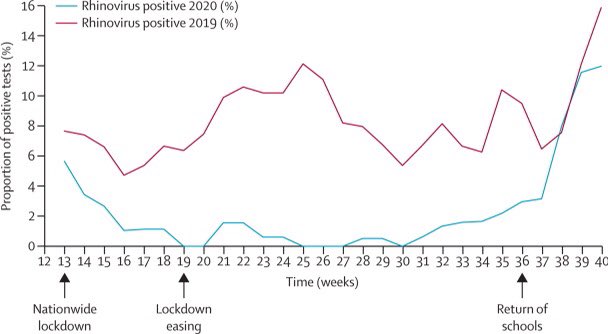
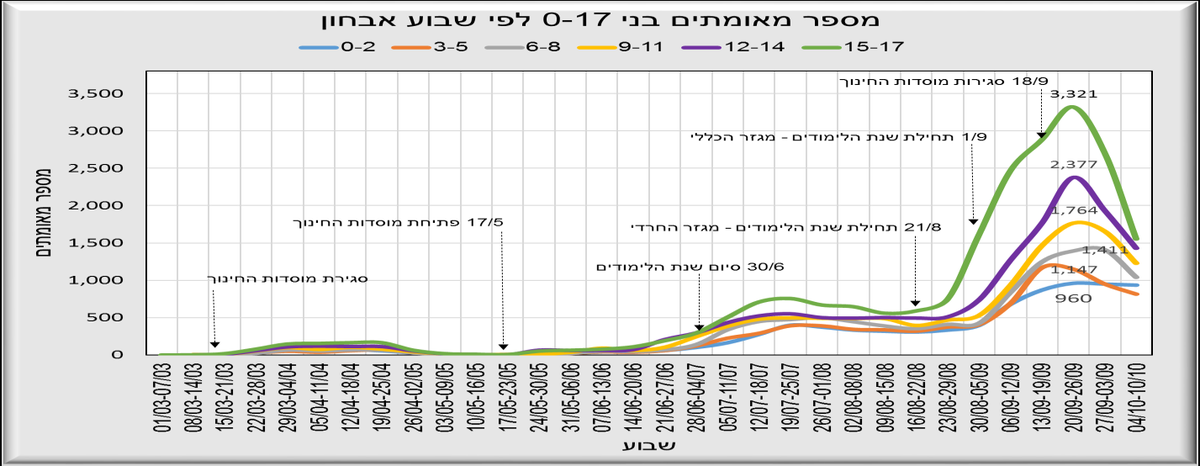
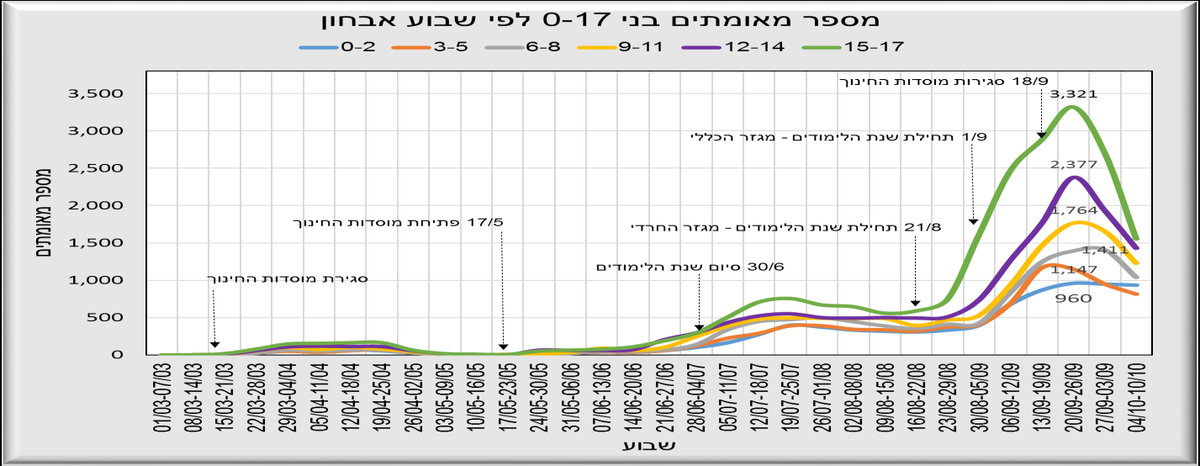
(6/7) As shown in the figure below, there was a marked rise in new cases following the reopening of schools on 1 September.
However, schools were not the only factor, as cases were already rising in the oldest age group (15-17 years).
However, schools were not the only factor, as cases were already rising in the oldest age group (15-17 years).
(7/7) The authors of the report conclude that the reopening of schools may accelerate the spread of #SARSCoV2, unless community transmission is low.
The authors recommend the return to schools be gradual.
The authors recommend the return to schools be gradual.
Addendum: It has been pointed out to me that schools for the Ultra-Orthodox community reopened on 21 August, slightly before the rest.
This may explain the earlier rise in cases which was most apparent in the 15-17 year age group.
This may explain the earlier rise in cases which was most apparent in the 15-17 year age group.
• • •
Missing some Tweet in this thread? You can try to
force a refresh