My paper on #COVID19, children, and schools is now published, with new material added.
"We can no longer afford to overlook the role children play in transmission if we hope to contain the virus."
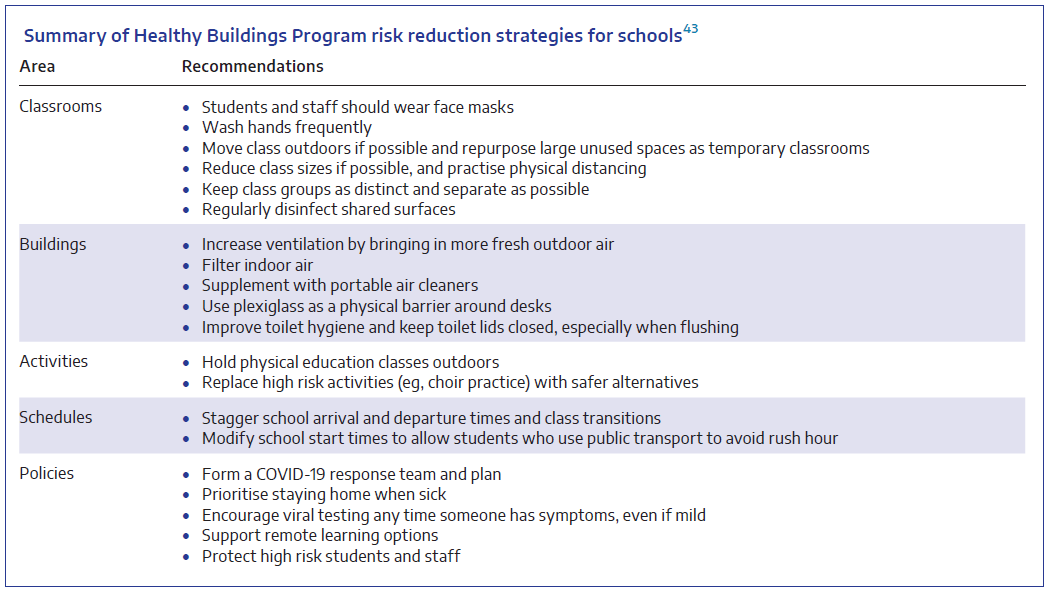
Precautions must be put in place in schools. #auspol
onlinelibrary.wiley.com/doi/full/10.56…
"We can no longer afford to overlook the role children play in transmission if we hope to contain the virus."
Precautions must be put in place in schools. #auspol
onlinelibrary.wiley.com/doi/full/10.56…
Important note:
The figure quoted for mortality in the paper is the case fatality rate, which is applicable to hospitalised children (a thankfully uncommon occurrence).
The infection fatality rate (mortality among all children who become infected) is probably 1000 times lower.
The figure quoted for mortality in the paper is the case fatality rate, which is applicable to hospitalised children (a thankfully uncommon occurrence).
The infection fatality rate (mortality among all children who become infected) is probably 1000 times lower.
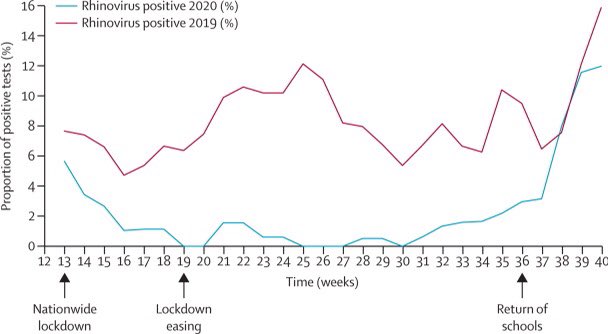
However, infections in children remain extremely important, because children can transmit the virus to older adults and other at-risk persons, who have far greater risk for mortality.
We will also not be able to control the pandemic unless we address transmission by children.
We will also not be able to control the pandemic unless we address transmission by children.
Translations are available here:
🇩🇪 Deutsch:
translate.google.com/translate?hl=d…
🇪🇸 Español:
translate.google.com/translate?hl=e…
🇫🇷 Français:
translate.google.com/translate?hl=f…
🇳🇱 Nederlands:
translate.google.com/translate?hl=n…
🇯🇵 日本語:
translate.google.com/translate?hl=j…
🇵🇹 Português:
translate.google.com/translate?hl=p…
🇩🇪 Deutsch:
translate.google.com/translate?hl=d…
🇪🇸 Español:
translate.google.com/translate?hl=e…
🇫🇷 Français:
translate.google.com/translate?hl=f…
🇳🇱 Nederlands:
translate.google.com/translate?hl=n…
🇯🇵 日本語:
translate.google.com/translate?hl=j…
🇵🇹 Português:
translate.google.com/translate?hl=p…
If you click on a link to one of the translated versions and see a message about cookies, try reloading the page.
You may need to reload the page more than once, but it should work after a couple of tries.
You may need to reload the page more than once, but it should work after a couple of tries.
• • •
Missing some Tweet in this thread? You can try to
force a refresh