Can contact tracing work for #COVID19?
Much effort assumes contact tracing works for COVID - surveillance testing assumes so
I’ve had major concerns - this paper reinforces it.
For fast pandemics, we cant act only on what has been successful before
1/
jamanetwork.com/journals/jamai…
Much effort assumes contact tracing works for COVID - surveillance testing assumes so
I’ve had major concerns - this paper reinforces it.
For fast pandemics, we cant act only on what has been successful before
1/
jamanetwork.com/journals/jamai…
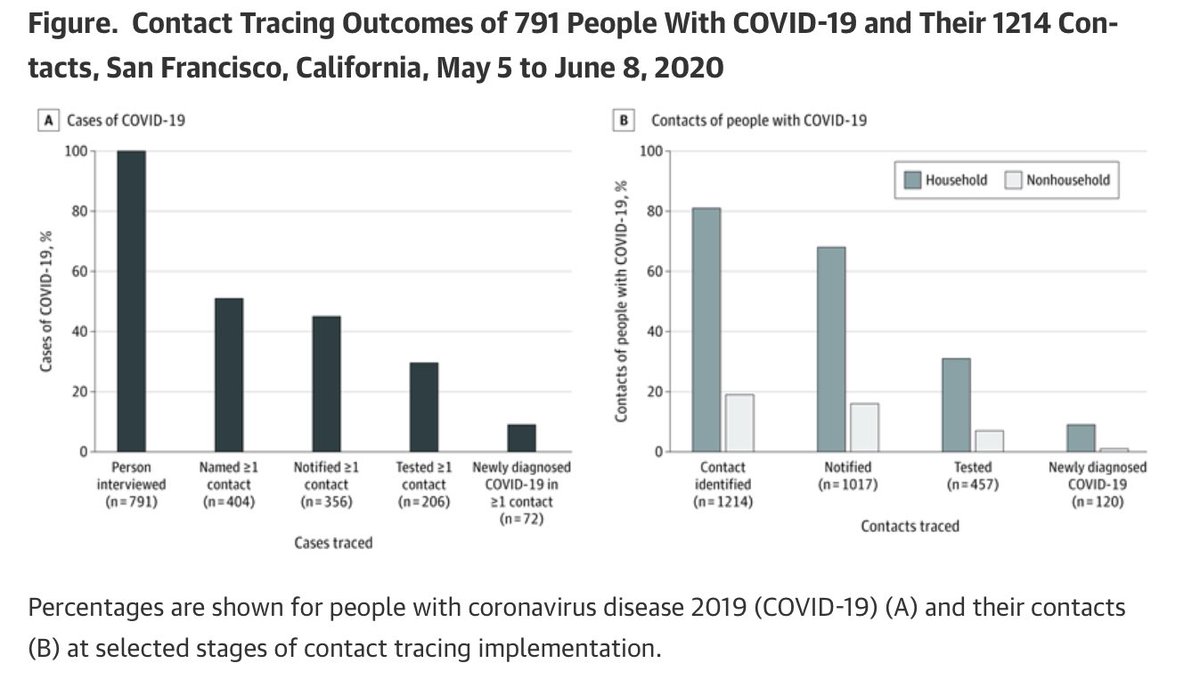
In this paper, 791 #COVID19 positive people were contact traced AND universal testing was recommended for their close contacts.
Ultimately only 120 people were discovered.
2/
Ultimately only 120 people were discovered.
2/
If COVID has an R of ~1.3… those 791 people perhaps led to >1000 additional cases.
If 120 were discovered... ~900 were not.
And this was an organized operation.
3/
If 120 were discovered... ~900 were not.
And this was an organized operation.
3/
Further, it is very likely those 791 people made up only a fraction of the actual positive cases that could have been traced at that time…
It’s possible we find only 10% of actual cases in many places to even start the contact tracing on...
4/
It’s possible we find only 10% of actual cases in many places to even start the contact tracing on...
4/
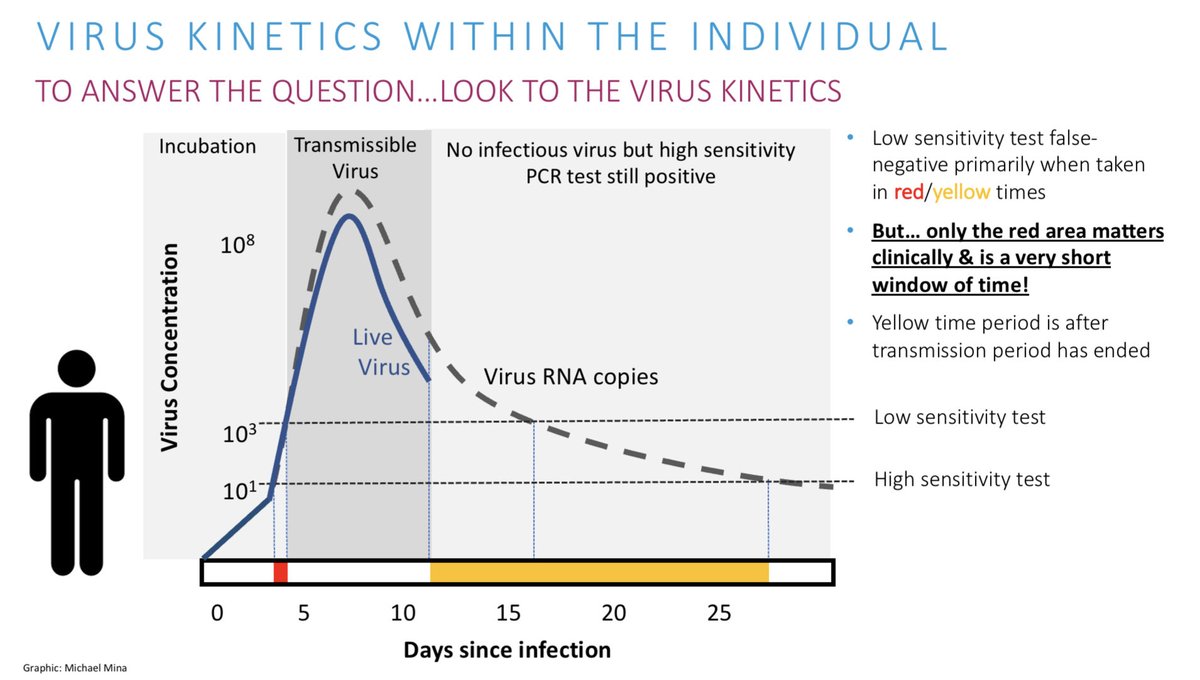
Further, the fraction (120) that were discovered were likely found late, many after infecting others.
Time from a symptomatic case to have symptoms to when contact tested was 4-10+ days.
Likely many contacts obtained results 6-15 days after the case became symptomatic.
5/
Time from a symptomatic case to have symptoms to when contact tested was 4-10+ days.
Likely many contacts obtained results 6-15 days after the case became symptomatic.
5/
Moreso, because many cases were actually asymptomatic, they likely didn’t even get their first PCR test until AFTER they were infectious
So the time from first being infectious to the contacts getting tested could be weeks or more for many.
6/
So the time from first being infectious to the contacts getting tested could be weeks or more for many.
6/
So overall, though 120 positive contacts were discovered through intense contact tracing, many of the contacts may have already themselves gone on to transmit.
Overall, a LOWER bound of 900 were very likely to have never been detected.
7/
Overall, a LOWER bound of 900 were very likely to have never been detected.
7/
Also, given the 791 constituted only a fraction of true positives at the time they were detected (because limited / inconvenient testing), the true number of new cases not detected in the collective weeks after the cases were identified could have been multiple 1000’s
8/
8/
With high #COVID19 cases, we need different models for public health.
Lab based testing / contact tracing can’t work with high cases for this virus.
As this paper showed, delays and massive under detection of infecteds means the effort just scratches the surface.
9/
Lab based testing / contact tracing can’t work with high cases for this virus.
As this paper showed, delays and massive under detection of infecteds means the effort just scratches the surface.
9/
To be clear, when cases are low and contact tracing resources plentiful, contact tracing can be very powerful.
But we shouldn’t let the ways that we’ve always done this dictate the ways we must deal with a fast global pandemic today.
10/
But we shouldn’t let the ways that we’ve always done this dictate the ways we must deal with a fast global pandemic today.
10/
I think a new era of massively distributed at-home rapid tests are our best hope to limit spread without massive lockdowns.
We should push for these so we can bring outbreaks under control & return to a semblance of normalcy as soon as we can – before vaccines.
11/11
We should push for these so we can bring outbreaks under control & return to a semblance of normalcy as soon as we can – before vaccines.
11/11
Also, we do have different somewhat less conventional options for contact tracing that *could* work better.
Backwards contact tracing is a different approach than conventional contact tracing, with greater efficiency for a quick moving virus like this
wellcomeopenresearch.org/articles/5-239
Backwards contact tracing is a different approach than conventional contact tracing, with greater efficiency for a quick moving virus like this
wellcomeopenresearch.org/articles/5-239
Finally. I’m not saying we should not contact trace.
Every case averted can prevent 10’s, 100’s or 1000’s of downstream cases. So we should continue... every bit counts.
We should also not assume contact tracing is sufficient and lose track of other powerful tools.
Every case averted can prevent 10’s, 100’s or 1000’s of downstream cases. So we should continue... every bit counts.
We should also not assume contact tracing is sufficient and lose track of other powerful tools.
• • •
Missing some Tweet in this thread? You can try to
force a refresh