1/Recapping some teaching points from @CPSolvers VMR today to keep me from refreshing NYT and 538 every 2 minutes. Thanks to @Flower_freeland for presenting an awesome case today.
clinicalproblemsolving.com/morning-report…
clinicalproblemsolving.com/morning-report…
2/ Case: A 28yM diagnosed w/uveitis about 4-5 weeks prior p/w N/V, weight loss, diffuse weakness. Most uveitis is anterior involving the iris (iritis). Anterior usually painful (front of eye in innervated). Infections commonly unilateral, autoimmune may be bilateral 

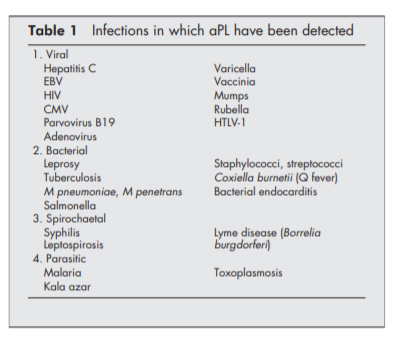
3/ Up to 50% of anterior uveitis is HLA-B27+. Lymphoma is an important mimic. Because the patient is from Vietnam, TB is the first thing that came to my mind. With TB, you should also thing of histo (and other funi). Knowing an immune status is important is working-up infection
4/Infectious causes of CNS disease & uveitis: Viral HSV, CMV, West Nile, HTLV-1, AIDS, SSPE, bacterial: bartonella, Whipple's, TB, leprosy, lyme, syphillis, ProtozoaL toxoplasmosis, PJP, parasite: gnathostomiasis (especially since patient from Vietnam) ncbi.nlm.nih.gov/pmc/articles/P…
5/ I do not focus on autoimmune disease as much here, but the below podcast has a great overview on autoimmune disease and the eye.
healio.com/news/rheumatol…
healio.com/news/rheumatol…
6/ PE showed white plaque on tongue, ptosis L eye, and ⬇️ muscle strength. Labs w/ lymphopenia (ALS 670), Na 128, HIV +. No CD4 count available. ALC correlates w/ CD4, ALC <1200 has +PV of 100% for CD4 <200 in HIV in 1 study but insensitive (NPV 32%). pubmed.ncbi.nlm.nih.gov/15477187/
7/MRI w/ scattered ring enhancing lesions. In HIV pts with multiple CNS ring-enhancing lesions, + toxo IgG, and compatible syndrome 90% probable dx is toxo. PCR is less sensitive. CNS lymphoma can have multiple lesions as well. 

8/@Estefroide also shared this great mnemonic for ring-enhancing lesions:
D: demyelinating disease (incomplete rim)
R: radiation necrosis or resolving hematoma
M: metastasis
A: abscess
G: glioblastoma
I: infarct, inflammatory, infectious
C: contusion
A: AIDS
L: lymphoma
D: demyelinating disease (incomplete rim)
R: radiation necrosis or resolving hematoma
M: metastasis
A: abscess
G: glioblastoma
I: infarct, inflammatory, infectious
C: contusion
A: AIDS
L: lymphoma
9/ Results of LP w/ 12 WBC (90%L) & multiple - inf w/u presumptively diagnosed w/ toxo (serology not available). Thanks @AnnaBriker and @RobWeberMDPhD for the great discussion. Always enjoy throwing thoughts (and zebras) around with @k_vaishnani & @TheRealDSrini in the chat.
• • •
Missing some Tweet in this thread? You can try to
force a refresh