1/ #tweetorial Next on the skeptical diagnosis series, I wanted to address cellulitis. I always feel a little angst when I am called to admit a patient w/ cellulitis. Does the patient really have cellulitis? In what % of pts diagnosed with cellulitis is the diagnosis incorrect?
2/ Here, I will focus and diagnosis and mimics. I plan to discuss mng of cellulitis later. Studies show that in 30-33% in patients diagnosed with cellulitis, the diagnosis is incorrect.
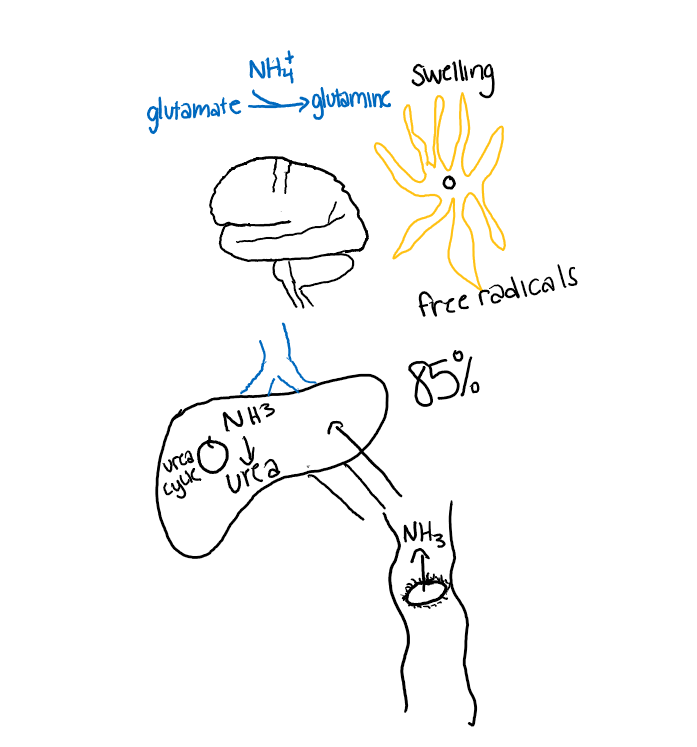
3/ Of those with an incorrect diagnosis, around 85% percent do not need hospitalization and 92% did not need antibiotics. Misdiagnosis is associated with millions in increased healthcare costs and up to 9000 nosocomial infections.
pubmed.ncbi.nlm.nih.gov/27806170/
pubmed.ncbi.nlm.nih.gov/29453874/
pubmed.ncbi.nlm.nih.gov/27806170/
pubmed.ncbi.nlm.nih.gov/29453874/
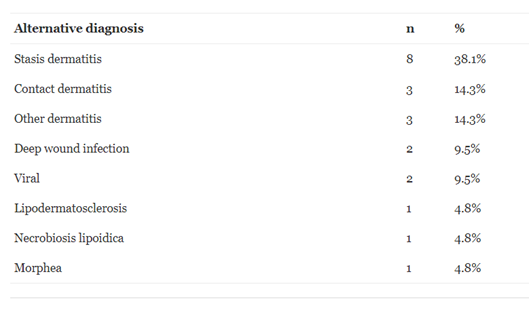
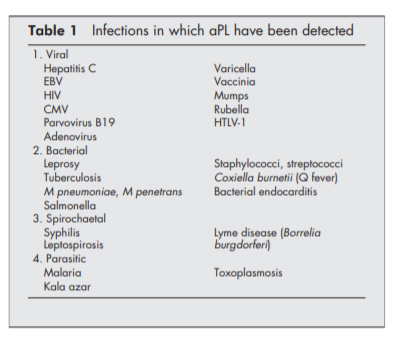
4/ What are the most common mimics? Stasis dermatitis is #1. “Bilateral cellulitis” is almost never cellulitis. Without open wounds, bilateral cellulitis is extremely rare. However, stasis dermatitis can also be unilateral as well. Table source: pubmed.ncbi.nlm.nih.gov/21426867/ 
6/ The diagnosis is difficult b/c that there is no gold standard to diagnose cellulitis. Erythema and ⬆️warmth are commonly seen in other conditions causing inflammation or stasis.
7/ Gout can cause erythema of the skin and leukocytosis and fever. Uric acid is not always elevated in an acute flare. Clues to gout is erythema overlying a joint, a history of gout, and improvement with anti-inflammatory agents.
9/ Cellulitis usually presents as unilateral, irregular spreading erythema w/ poor demarcation. There is associated swelling and ⬆️warmth. The swelling can often have a dimpled appearance d/t lymphatic involvement.
Table source: pubmed.ncbi.nlm.nih.gov/22794815/
Table source: pubmed.ncbi.nlm.nih.gov/22794815/

10/ In those w/ cellulitis, inflammatory markers are commonly ⬆️ but lack of ⬆️inflammatory markers does not r/o cellulitis & inflammatory markers are non-specific: Fever- 30-80%, WBC- 30-50%, ESR 60-92% ,CRP 75-95% ,Blood cultures + <10% of time
Source: pubmed.ncbi.nlm.nih.gov/22794815/
Source: pubmed.ncbi.nlm.nih.gov/22794815/
11/Procalcitonin levels are not reliable (pubmed.ncbi.nlm.nih.gov/30051724/). 1 prediction model, the ALT-70, uses asymmetry, leukocytosis, tachycardia, and age (pubmed.ncbi.nlm.nih.gov/28215446/). This model had a sensitivity (98%) and negative predictive value (91%) (pubmed.ncbi.nlm.nih.gov/30003987/)
12/ However, very few models that are well validated per this 2019 review:(pubmed.ncbi.nlm.nih.gov/30844076/). Dermatology evaluation also shown to improve diagnosis.
13/ Conclusions:
☄️In 30% of cases, diagnosis of cellulitis is incorrect.
☄️Incorrect diagnosis leads to increased cost, hospitalizations, and nosocomial infection risk.
☄️ If bilateral, dx is unlikely to be cellulitis.
☄️ Venous stasis is the most common cellulitis mimic.
☄️In 30% of cases, diagnosis of cellulitis is incorrect.
☄️Incorrect diagnosis leads to increased cost, hospitalizations, and nosocomial infection risk.
☄️ If bilateral, dx is unlikely to be cellulitis.
☄️ Venous stasis is the most common cellulitis mimic.
14/
☄️Most w/ cellulitis have CRP ⬆️ but this is non-specific and normal inflammatory levels do not r/u cellulitis
I welcome other thoughts from #dermtwitter.
Main sources (others as referenced): jamanetwork.com/journals/jama/…
pubmed.ncbi.nlm.nih.gov/22794815/
☄️Most w/ cellulitis have CRP ⬆️ but this is non-specific and normal inflammatory levels do not r/u cellulitis
I welcome other thoughts from #dermtwitter.
Main sources (others as referenced): jamanetwork.com/journals/jama/…
pubmed.ncbi.nlm.nih.gov/22794815/
Also, check at this great graphic from @LizzyHastie on ddx for a red leg:
https://twitter.com/LizzyHastie/status/1219042698755067904
• • •
Missing some Tweet in this thread? You can try to
force a refresh