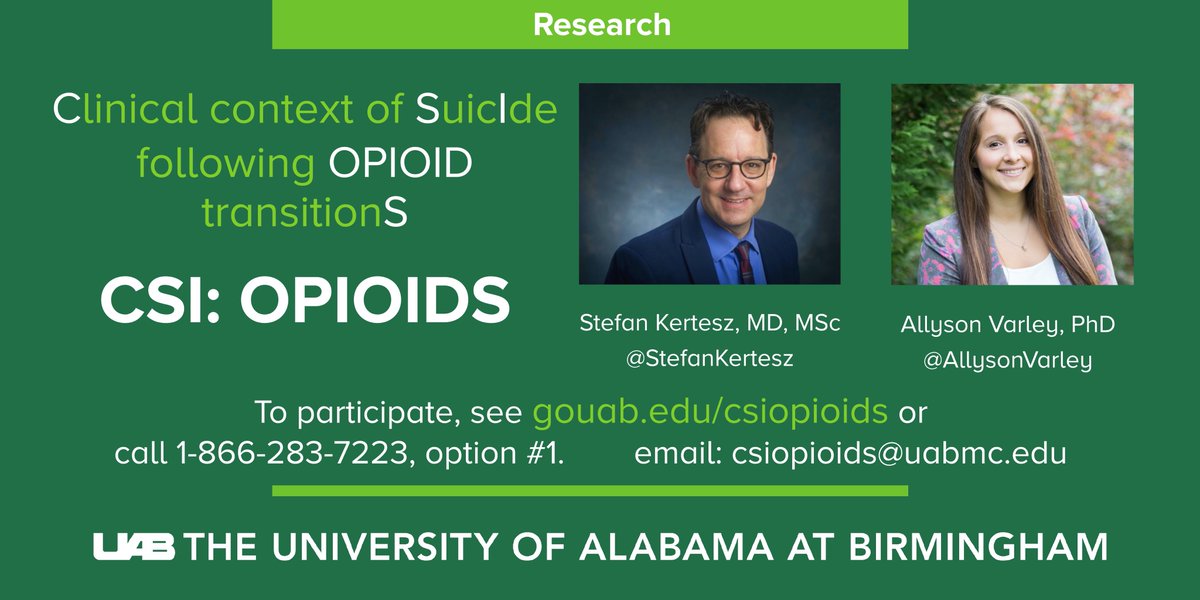
1/Last week we launched CSI:OPIOIDs, our research survey for bereaved families+friends who have lost a person with pain to suicide during a change in opioid prescribing. I want to say why this matters (fyi: it's at go.uab.edu/csiopioids ,or type URL if click-thru fails). First:
2/The recruitment letter approved by our ethical review board at @UABNews (called an IRB) is here: drive.google.com/file/d/19BRmWH…
3/Our team is inspired by the work of patients and families who have already come forward and spoken about this serious issue. We have been inspired by the painstaking efforts of people like @PainPtFightBack to record every death that comes to light.
4/Our team consists of over a dozen people who are working together, making sure that recruitment is done correctly, many at UAB. The team also includes nationally recognized experts on suicide and in Veterans' care
5/Some have asked: Why can’t we just study deaths that have already been recorded by families on Facebook or Twitter? There are two reasons:
6/First: The ethical issues involved.
Before we can seek health information about anyone, we need *consent* to do so, to interview them, etc. Everything we do as scientists requires consent, after review by a university IRB.
Before we can seek health information about anyone, we need *consent* to do so, to interview them, etc. Everything we do as scientists requires consent, after review by a university IRB.
7/Second: The need for precise details: a report on Twitter or Facebook does not give enough information to help us say in a scientifically defensible way, “here are how these tragedies happened and what steps would have prevented them.”
8/To clarify: CSI:OPIOIDs is a confidential survey with no pay or reward for anyone.
If it succeeds, it will show there are family members or friends of a loved one who are willing to share details of a suicide in a survey, about what they think happened.
If it succeeds, it will show there are family members or friends of a loved one who are willing to share details of a suicide in a survey, about what they think happened.
9/Our study name “CSI:OPIOIDs” is meant to imply the future steps.
Our *future goals* are to ask consenting survivors if they will be willing to be interviewed in a detailed and structured way. This can’t happen until we find out if they are out there.
Our *future goals* are to ask consenting survivors if they will be willing to be interviewed in a detailed and structured way. This can’t happen until we find out if they are out there.
10/If we could do all the above detailed work right away, we would. My colleague @AllysonVarley and I have submitted applications to research agencies since 2018. We have put hundreds of hours into this, all unpaid, building the study plan and teaming up with suicide scholars.
11/However, we have to do this first.
We have to show that bereaved survivors will trust us.
If we don’t do that, then these deaths will not be studied because smart grant reviewers will read our proposals and say “what makes you think you can EVER do a study like this?”
We have to show that bereaved survivors will trust us.
If we don’t do that, then these deaths will not be studied because smart grant reviewers will read our proposals and say “what makes you think you can EVER do a study like this?”
12/On the other hand, if 50 survivors step forward and say, “we care, and we want to discuss these deaths, and make sure they are paid attention to,” then 2 things will happen:
13/ 1st: Their deaths will be impossible for policymakers, including agencies like CMS, DEA, NCQA and Congress to ignore
2nd: It will make it harder for reviewers to say “Your idea can never work and we won’t fund any studies on this"
2nd: It will make it harder for reviewers to say “Your idea can never work and we won’t fund any studies on this"
14/I have spoken many times as an advocate, but in this, @AllysonVarley and I speak as scientists. At this point, we can’t state scientifically what makes a suicide the outcome of an opioid reduction. Suicide is not caused by ONE thing. It’s complicated. 

15/Some people may think problems after opioid reduction are simple.
Some say, “taper slowly and there will be no suicides.” Others say, “never reduce opioids, and all will be fine.”
We understand these thoughts.
And we don’t think these views are based on evidence.
Some say, “taper slowly and there will be no suicides.” Others say, “never reduce opioids, and all will be fine.”
We understand these thoughts.
And we don’t think these views are based on evidence.
16/*Evidence* is needed because health systems will not change what they do, clinicians will not change their practices, and regulators and payers will not change what they do, unless offer more serious understanding of these catastrophic events.
17/Many patients with pain and their families understandably distrust scientists, experts, and researchers.
Patients in pain experience stigma, have difficulty finding adequate care, and observe professionals willing to dismiss the traumas they experience.
Patients in pain experience stigma, have difficulty finding adequate care, and observe professionals willing to dismiss the traumas they experience.
18/When experts say that they already know how to explain serious problems, without studying them, that oversimplifies. It tends to convey stigma, intended or not. We saw that recently in the student paper at Brandeis. 

19/As scientists, we *cannot know what our research will show in advance*.
What we can commit to is to work with care, to respect ethical rules, and to be instructed by the team we have recruited: family members, experts in opioids and pain, and experts in suicide.
What we can commit to is to work with care, to respect ethical rules, and to be instructed by the team we have recruited: family members, experts in opioids and pain, and experts in suicide.
20/I hope that some are familiar with my years of advocacy in this area, publicly speaking out, authoring manuscripts, testifying, and advocating with policymakers and government officials for protections for patients in pain
21/And advocacy isn’t enough.
Federal, state, & other agencies will reshape care when we can offer a scrupulous, scientific understanding of incredibly tragic events, i.e. suicides of patients after they lost access to pain care. These are events we think should never happen.
Federal, state, & other agencies will reshape care when we can offer a scrupulous, scientific understanding of incredibly tragic events, i.e. suicides of patients after they lost access to pain care. These are events we think should never happen.
22/For people who wish to see more of our scientific work on this topic, here is one recent article by @BethDarnall , Dr. Megan McCullough, @AllysonVarley and me from @JournalGIM :
link.springer.com/article/10.100…
link.springer.com/article/10.100…
23/We welcome questions on Twitter or to email csiopioids@uabmc.edu
Or click the link. If the "click through" from Twitter does NOT work (which I've seen recently, type into browser --with "https" first - 'go.uab.edu/csiopioids"--
Please share!
Or click the link. If the "click through" from Twitter does NOT work (which I've seen recently, type into browser --with "https" first - 'go.uab.edu/csiopioids"--
Please share!
• • •
Missing some Tweet in this thread? You can try to
force a refresh