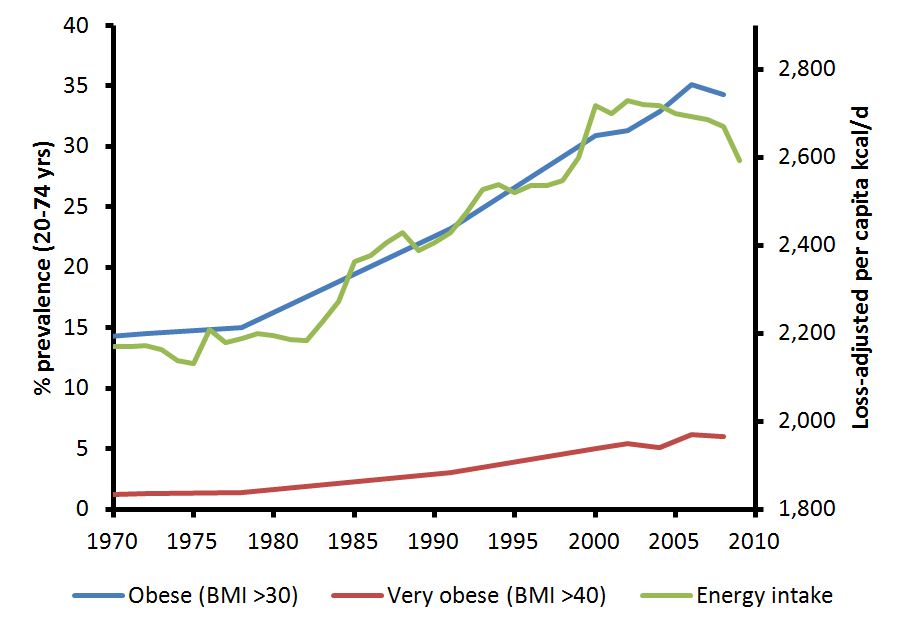
1/ In honor of #WorldDiabetesDay2020, and to directly address two significant public health threats of the 21st century, I want to discuss very-low-energy-diets and low-energy-diets as a potential treatment for obesity and T2DM. [thread]
2/ Total Diet Replacement (TDR) strategies have been extensively studied and found to be an effective dietary intervention to promote a Calorie deficit and reduced food intake. 

3/ I originally became interested in TDR interventions reading the many works of Dr. Thomas Wadden, demonstrating clinically significant short-term weight loss with VLEDs. [Tsai & Wadden, 2006] 

4/ Also, many people forget that the Look AHEAD study utilized meal replacements, albeit with a more conservative daily caloric goal, as part of their treatment strategy. [Wadden et al., 2009] 

5/ My interest peaked when I came across the DiRECT trial, a cluster-randomized trial of formula-based LED, and revealed that glycemic control is directly related to the amount of WL. Notably, T2DM remission was not only possible but likely if >/=15 kg was lost. 



6/ These findings have been repeated with even more impressive remission results (achieving T2DM remission & normoglycemia in 61% & 33%, respectively) in a cohort of young, Middle-eastern and N African individuals with T2DM for </= 3 yrs. 

7/ So...where did this concept come from? The seminal work was done by Roy Taylor and colleagues through the development of the Twin-Cycle hypothesis and subsequent validation studies: COUNTERPOINT and COUNTERBALANCE studies.
⬇️
⬇️
https://twitter.com/MichaelAlbertMD/status/1323755321601478656?s=20
8/ Exciting right?!! But is it sustainable? That is the million-dollar question for any lifestyle intervention. Tsai and Wadden 2006 found that VLED/LEDs may have issues with weight regain with participants regaining anywhere from 41-62% of the initial WL at 12 months. 

9/ In fact, I tried a LED for 6 days to get a glimpse into some of the challenges. Over the week, I lost 2.5 lbs. You can read more about my trial here.⬇️
https://twitter.com/MichaelAlbertMD/status/1324435424765304837?s=20
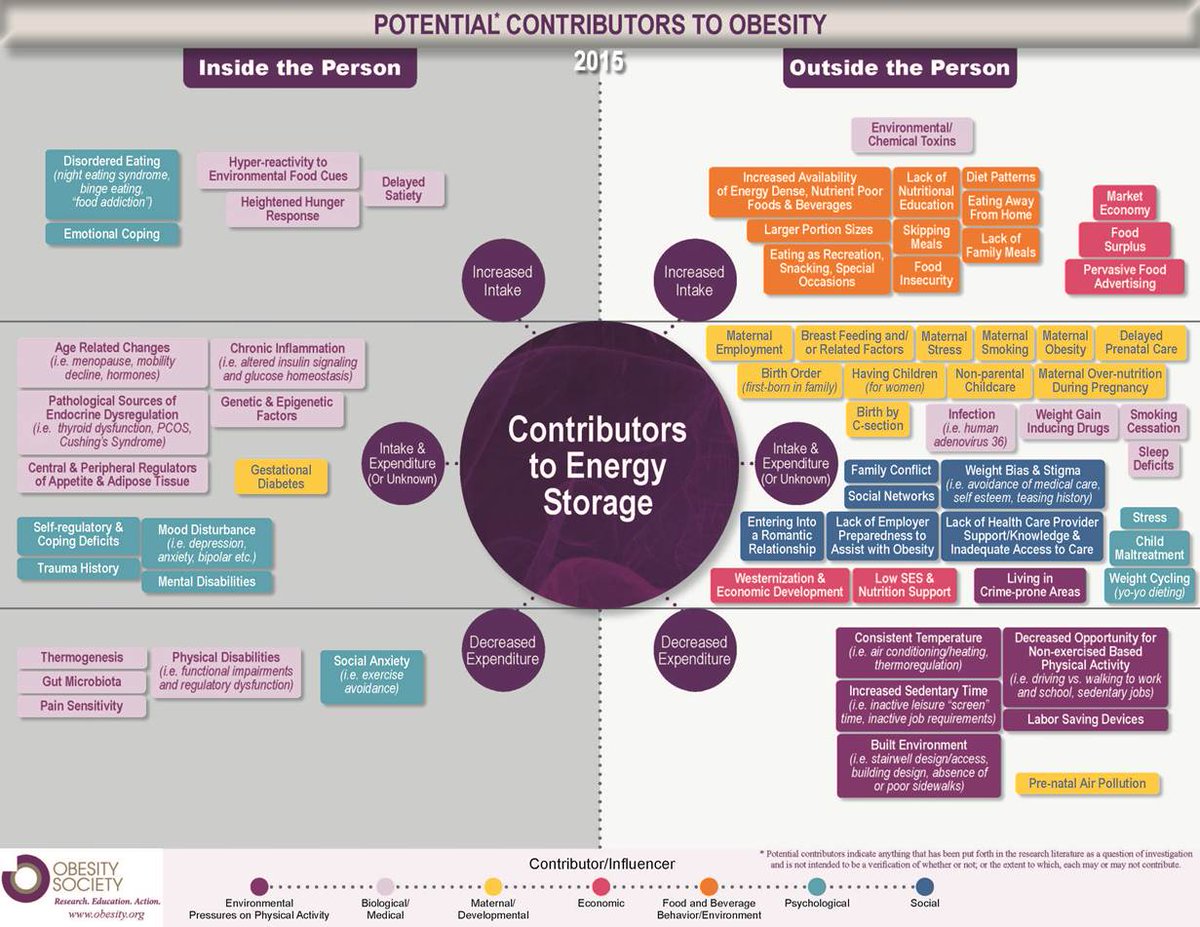
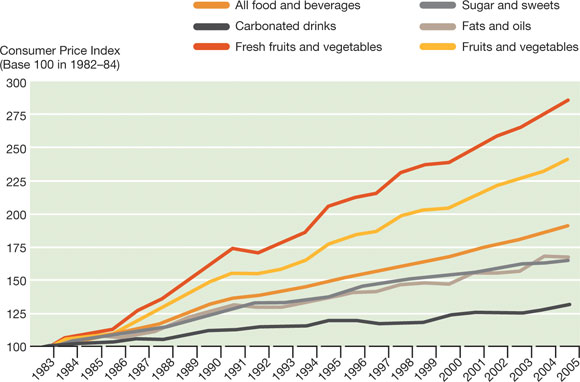
10/ And while hunger in the physical sense was not too bad, my cravings or what I call "THE HUNGRY BRAIN" was rough. I wanted to EAT despite being FULL. Food images, the smell of food, or any reference to food were triggering, which I believe plays a major role in wt regain.
11/ One way to combat these counter-physiological processes occurring in the brain is to use anti-obesity medications.
Johannsson et al., 2014
---
Wt loss maintenance is more successful w/ GLP1a [Lepsen et al., 2015]
Johannsson et al., 2014
---
Wt loss maintenance is more successful w/ GLP1a [Lepsen et al., 2015]

12/ Or use a high protein diet, which has been shown to lead to less wt regain. [Aller et al., 2014] 

13/ Or maybe a longer food reintroduction phase: 6 wk > 1 wk, with individuals being able to exhibit increased eating restrain with more gradual food reintroduction.
[Gripeteg et al., 2010]
[Gripeteg et al., 2010]

14/ Also, I am encouraged by the results of a prez @ #OW2020, which was a retrospective analysis of a TDR program @ UPMC.
@6 months...
Avg Wt loss ~17%
Mean ⬇️in A1c ~1.5%
What's more? They included patients with T2DM of different durations and used anti-OB meds to help w/ WL.

@6 months...
Avg Wt loss ~17%
Mean ⬇️in A1c ~1.5%
What's more? They included patients with T2DM of different durations and used anti-OB meds to help w/ WL.


15/ My hope is that we continue to identify evidence-based approaches to not only manage but remit T2DM. These interventions need greater financial support for their implementation. And of course, we should individualize approaches based on patient preferences.
16/ If you want to read a great overview on this topic discussed above, I encourage you to check out this summary by @BrownAdey: onlinelibrary.wiley.com/doi/10.1111/nb…
• • •
Missing some Tweet in this thread? You can try to
force a refresh