
Is there a radiation dose-response relationship for rectal cancer managed non-surgically?
Short answer: Yes - at least based on published patient series
Longer answer: See our #ESTRO2020 Poster Highlight - or thread below
#rectalcancer
#radonc
postersessiononline.eu/173580348_eu/c…

Short answer: Yes - at least based on published patient series
Longer answer: See our #ESTRO2020 Poster Highlight - or thread below
#rectalcancer
#radonc
postersessiononline.eu/173580348_eu/c…


Non-operative management of rectal cancer is becoming increasingly important - more and more patients are offered observation instead of surgery if they have a complete response after (chemo-)radiotherapy #radonc #ESTRO2020 

Most published series are only reporting on that select group of patients - the ones who got a complete response. That's great if we want to understand if observation is a safe strategy for those patients #ESTRO2020
thelancet.com/journals/lance…
thelancet.com/journals/lance…
But it doesn't tell us how large a proportion of *all treated* patients can get long term control without surgery. Or really give us any robust information as to whether we can increase that number by altering our treatment up front #ESTRO2020 #radonc
We are particularly interested in whether dose escalation has a role to play!
I've previously explained why dose escalation to the primary tumour probably doesn't help much in the neoadjuvant setting:
But how about for organ preservation? #ESTRO2020
I've previously explained why dose escalation to the primary tumour probably doesn't help much in the neoadjuvant setting:
https://twitter.com/cancerphysicist/status/1330194799195009031
But how about for organ preservation? #ESTRO2020
We systematically searched the literature for studies of non-operative management of rectal cancer; which:
1) Included the total patient cohort treated, not just those managed with observation
2) Reported the dose to tumour
3) Reported total proportion without surgery at 2 years
1) Included the total patient cohort treated, not just those managed with observation
2) Reported the dose to tumour
3) Reported total proportion without surgery at 2 years
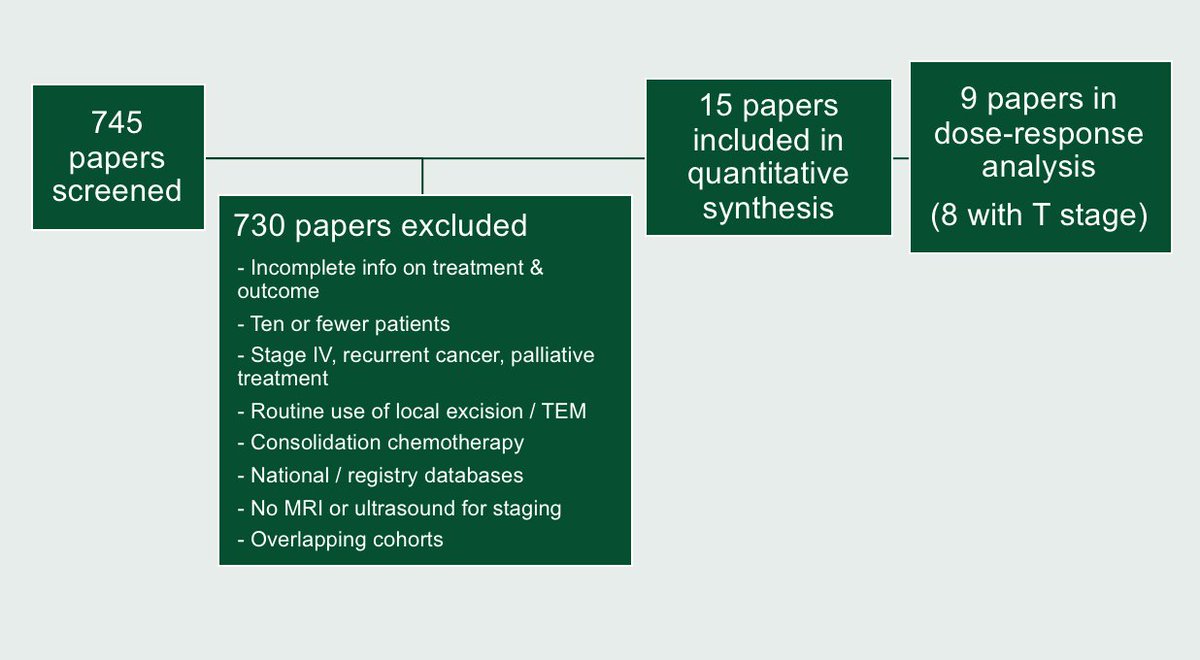
Now, out of the 15 papers that we found, 6 of them didn't systematically screen patients for complete response. So we couldn't trust that they actually allowed everybody to avoid surgery who could do so - i.e. their estimate of 'proportion managed without surgery' will be biased
One more tricky part: Some of the patient cohorts were treated with brachy or Papillon boosts - so estimating the tumour dose wasn't super easy ...
#ESTRO2020 #medphys
#ESTRO2020 #medphys
For one cohort, I actually had MRI-based dose plans, so getting exact EQD2 doses was possible. And for another (Papillon) cohort, I got information on tumour thickness and individual prescriptions + applicators - so I could estimate the average tumour EQD2
#ESTRO2020 #medphys

#ESTRO2020 #medphys


For others, I did a lot of approximations, based on average cohort tumour size and application information ...
(Side note: We're improving on this! People have kindly shared individual patient dose data with me, so we'll do better for the final publication!)
#ESTRO2020
(Side note: We're improving on this! People have kindly shared individual patient dose data with me, so we'll do better for the final publication!)
#ESTRO2020
But altogether, we were able to estimate a dose response for local control (without surgery) as a function of tumour EQD2, using a weighted and bounded logistic regression. Our best estimate:
D50 = 71Gy
gamma50 = 1.1
#ESTRO2020 #radonc
D50 = 71Gy
gamma50 = 1.1
#ESTRO2020 #radonc

One more important thing:
We know that smaller / early stage rectal cancers are more likely to respond to RT. There is an obvious risk that the observed dose-response relationship is purely due to cohorts with early cancers also receiving higher doses
#ESTRO2020 #radonc
We know that smaller / early stage rectal cancers are more likely to respond to RT. There is an obvious risk that the observed dose-response relationship is purely due to cohorts with early cancers also receiving higher doses
#ESTRO2020 #radonc
So we controlled for this! We used a IPD meta analysis based measure of relative response probability, adjusted the data points accordingly, and allowed for different upper bounds for T1-2 and T3-4 cancers
thelancet.com/journals/lanon…
#ESTRO2020 #radonc
thelancet.com/journals/lanon…
#ESTRO2020 #radonc
Even when doing this, we still saw clear dose-response
- and we found different upper bounds for the maximum local control we can expect to achieve for early (~80%) and advanced (~65%) cancers.
D50 = 66Gy for T1-2 and 85Gy for T3-4
#ESTRO2020 #radonc
- and we found different upper bounds for the maximum local control we can expect to achieve for early (~80%) and advanced (~65%) cancers.
D50 = 66Gy for T1-2 and 85Gy for T3-4
#ESTRO2020 #radonc

Does this provide definite evidence of a dose-response relationship? Obviously not. We still need randomized trials ... but that's why we are currently doing them! 😉
APHRODITE ctru.leeds.ac.uk/aphrodite/
WW3 clinicaltrials.gov/ct2/show/NCT04…
OPERA clinicaltrials.gov/ct2/show/NCT02…
#ESTRO2020 /END
APHRODITE ctru.leeds.ac.uk/aphrodite/
WW3 clinicaltrials.gov/ct2/show/NCT04…
OPERA clinicaltrials.gov/ct2/show/NCT02…
#ESTRO2020 /END
• • •
Missing some Tweet in this thread? You can try to
force a refresh



