
I don't think that this study by Basavaraju et al from @CDCgov can be taken as evidence that #COVID19 was circulating in the US in December 2019. 1/10
academic.oup.com/cid/advance-ar…
academic.oup.com/cid/advance-ar…
The authors do a careful serological investigation, but it necessarily suffers from testing a large number of samples with an assay that is not perfectly specific. 2/10
The ELISA used by the authors has a stated specificity of 99.3% and the authors tested 519 "true negative" blood samples collected from 2016 to 2019 from healthy adults and suspected hanta virus patients and observed 3 false positives (0.6%) matching this specificity. 3/10
The authors tested 1912 blood samples collected between Dec 13 and Dec 16 2019 and observed 39 positives (2.0%). A Fisher's Exact Test comparing 3/519 to 39/1912 is narrowly significant with p = 0.02. 4/10
However, there is ample reason to expect that individuals recently recovered from seasonal coronavirus infection will have more cross-reactivity to SARS-CoV-2 than random healthy adults. In fact this can be seen in this paper by Freeman et al (ncbi.nlm.nih.gov/pmc/articles/P…). 5/10
Here, ELISA titers are higher in individuals who were recently infected with seasonal coronavirus compared to random healthy adults. This is particularly the case in related betacoronaviruses OC43 and HKU1. 6/10 

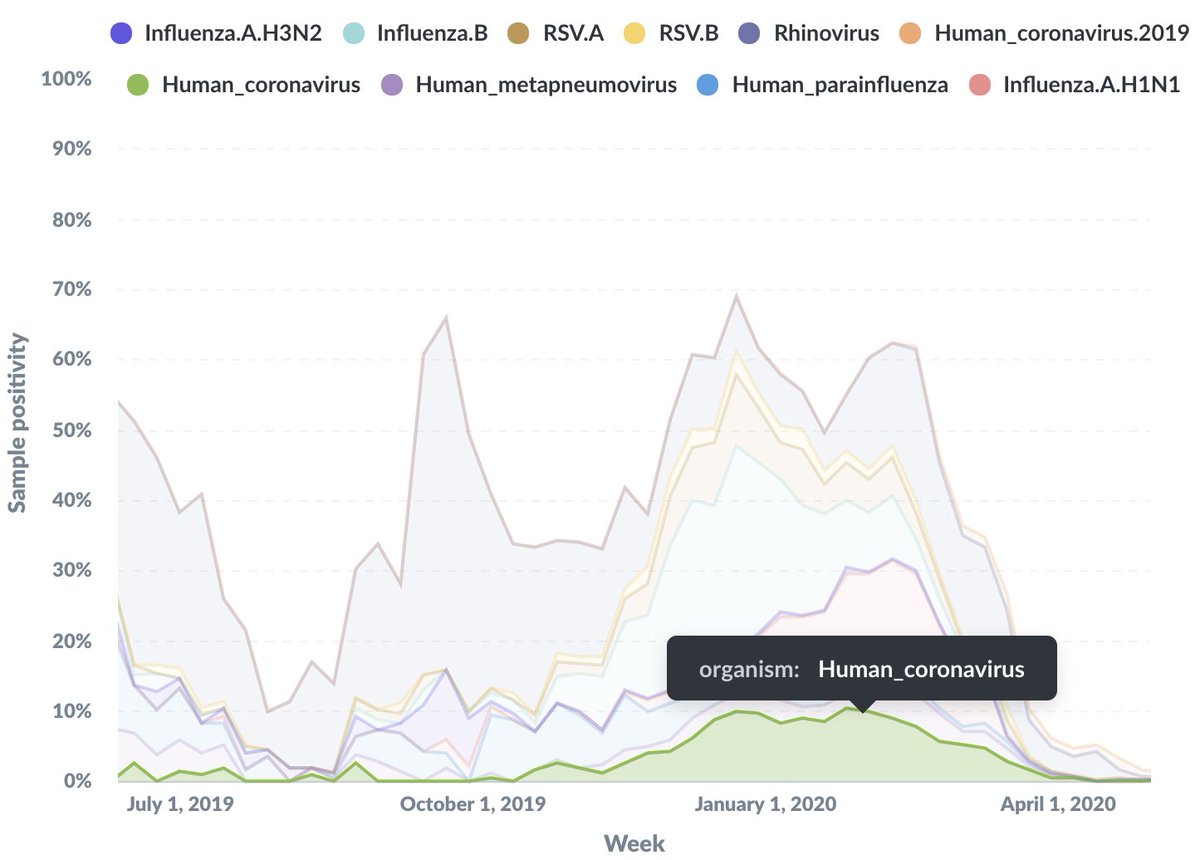
Additionally, we know that seasonal coronaviruses circulate at higher frequencies in the winter. We can see this in @seattleflustudy data where there is significant seasonal coronavirus circulation in Dec 2019. 7/10 
It seems highly likely to me that the 39 "positives" from Dec 13 to Dec 16 reported by Basavaraju et al are due to cross-reactivity from recent seasonal coronavirus infection. It would just take a slight decrease of assay specificity to ~98% to explain this outcome. 8/10
The authors highlight the study's limitation due to "potential cross reactivity with human common coronavirus infection" in the paper's discussion, but it unfortunately didn't make it into the @WSJ story (wsj.com/articles/covid…). 9/10
The other angle to consider is that if we're supposed to believe that 2.0% of random blood donors in Dec 2019 are COVID+ this would translate to millions of infections in the population at large, in which case we would have noticed due to people dying in large numbers. 10/10
Follow up #1: Also, a reminder that we at the @seattleflustudy PCR tested 3600 samples from individuals with acute respiratory illness collected in January 2020 from Seattle and found zero positives for COVID-19. This is a much more specific assay.
https://twitter.com/trvrb/status/1249414295042965504
Follow up #2: This doesn't mean that COVID-19 was completely absent from the US in January 2020, just that prevalence at that time was exceptionally low. Finding 0/3600 COVID+ acute respiratory specimens doesn't square with theoretical 2% ELISA positivity in Dec.
• • •
Missing some Tweet in this thread? You can try to
force a refresh







